The 3 Languages I Speak at the Hospital as the Mom of a Child With Special Needs
Nine years ago I started this journey with our third child, but not yet as a nurse — more importantly, as a mom of a child with special needs. Little Wade stayed in the NICU for the first three months of his life. Our lives had been thrown into this world of surgeries and doctors and hospitals and specialists. It was like I had stepped onto another planet with its own language and ways of doing things, completely different than anything I had ever known. So we did what any parent would do and we jumped right in.
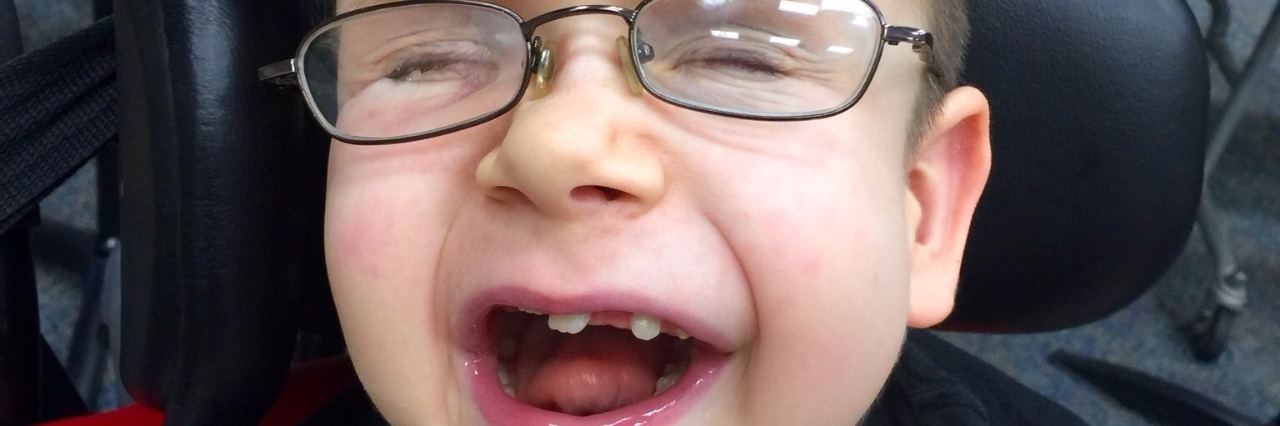
Little Wade had a pretty rough start: more than 50 surgeries in the first five years with accompanying hospital stays. He would quit breathing without explanation and we wouldn’t know what to do, except bag him to keep him alive. We’d call the doctors, rush him to the hospital, try different medicines, position him differently, try different foods, anything they said to do, we did. It got so bad that he was life-flighted six times in three months; each time we were told the same thing: “His MRI looks fine.” I had started to guess that it was likely something to do with his head, but since he was non-verbal I could never know for certain. For years we went on like this. His oxygen saturations dropped into the 30s while we frantically bagged him back up. We went to the hospital only to be looked at in pity. I was the “poor special needs mom” who just doesn’t want to let go. And I couldn’t convey to them that yes, he does have special needs, but they only see him when he’s sick. They don’t see him when he’s happy and playing with his toys and grabbing his feet to put in his mouth.
Trying to find answers, we took Wade to Seattle, Cleveland, Dallas, and then back to Houston. We found a neurosurgeon at Texas Children’s who had trained in Chicago, which was our next destination. Reluctantly, we went to see him. It started out like all the other appointments: me explaining in my mom language what was going on. Wade would just quit breathing. He said, “His MRI is unremarkable. It’s what I would expect for someone with Pfeiffer syndrome.” And I said, yes, I understand that. But I’m telling you something is wrong. When he lays down, he’s fine, but when I sit him up he starts crying and pushing back to lay down, he starts hitting his head. I asked if we could do an ICP monitor to see if there’s pressure in his brain. By now, I had surmised through my research that his shunt wasn’t working right and perhaps it was over-draining since his ventricles were always flat on the MRIs. The doctor said sure, why not. So he went into the operating room the next day. When the doctor was walked in he came over to me and said, “If I know one thing, it’s that I don’t know everything and these kids always surprise me. So let’s just see what we find.”
Wade was sent to the PICU for observation while the ICP monitor was in place. A few hours later, the doctor came to check on Wade. He walked in and went to the ICP monitor display at the head of the bed, calculated some numbers and said, “Do you see that number?! That number is 90. His ICP is 90! Normal is 0 to 20, 20 when you’re laughing, but it goes right back down.” He hurried away and we were immediately scheduled for emergency surgery to replace Wade’s shunt.
Being in a hospital can be isolating. You’re in another world, with signs that are not in the language you know, with people who don’t understand you or what you’re going through. Sometimes, or rather, most of the time, you’re the last to know the plan, even though you are the one living it. Many times I sat in his hospital room feeling as if I, myself, were a void, questioning my own value, my own ability to care for and speak for my son because no one asked what I thought.
And then, one day I decided to go to nursing school. I intended to get some letters behind my name so someone would listen to me, so I could be part of my own son’s team, not really fully understanding that I am his team, and the medical team is just the periphery.
Over the years I have became aware that we all have the same goals, but speak three different languages:
First, there is “mad mom” — the version of me when I am crying and mad when trying to tell you there’s something wrong. I can’t tell you why, it’s just a feeling and I know that something is different.
Second, there is the “medical” language — this is the language I learned from other parents. It sounds something like, “I am concerned that Wade’s ICP is increased because we know that despite his MRI being unremarkable, he does have decreased CSF flow in the posterior portion of his brain due to the venous congestion relative to his Pfeiffer syndrome, and this is not the normal disease pathway for hydrocephalus.”
Third, there is the “data” language. This I began to understand as I am now in administration in the hospital. I am learning that I need to be able to “quantify my claims and stratify down as much as possible so we could put numbers to it and justify.”
What I’ve learned through all this is that as an advocate, it’s about taking an experience and translating it into something meaningful for all three areas that intersect patient care: the person(s) receiving care, the person giving care, and the person ensuring we get paid for it and are able to keep the lights on.
We want to hear your story. Become a Mighty contributor here.