To the Psychiatrist Who Said It ‘Wouldn’t Be so Bad’ to Have OCD During the COVID-19 Pandemic
Editor's Note
If you struggle with obsessive-compulsive disorder (OCD), the following post could be potentially triggering. You can contact the Crisis Text Line by texting “START” to 741-741. To find help, visit the International OCD Foundation’s website.
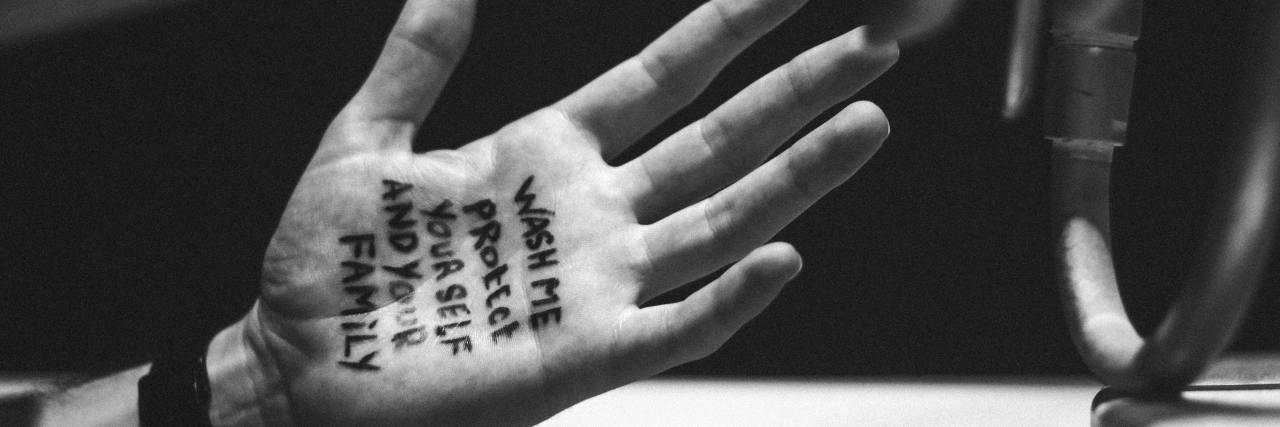
In case you missed it, The Wall Street Journal published an opinion piece on March 31, 2020, written by Dr. Aboujaoude, a psychiatrist and professor of psychiatry at Stanford University. The article is titled “We All Need OCD Now.” Given the current events that are unfolding related to the coronavirus (COVID-19), the new viral strain in the coronavirus family that affects the lungs and respiratory system, the CDC has released a variety of protocols for cleaning and sanitizing our hands, environments and frequently used objects. In this article. Dr. Aboujaoude writes about a patient of his who has obsessive-compulsive disorder (OCD), and then ends the article by suggesting that, “[a] little OCD, right now, wouldn’t be so bad.” He recommends: “we can look to people like [his] patient for discipline and inspiration.”
First and foremost, I want to thank Dr. Aboujaoude for his work in the field of mental health and psychiatry. Psychiatry is a discipline that requires years and years of hard work, persistence and determination. I have the utmost respect and appreciation for all doctors, especially during these trying times. That said, I do think it is worth sharing an alternative opinion to your article, doctor.
I have the unique experience of being both a rising mental health professional and a person with OCD. I was motivated to enter the field of mental health due to my own journey with mental illness. Doctor: from mental health professional to mental health professional, I feel this article invalidates the experience of our clients/patients. Anxiety can be viewed as evolutionary to an extent, yes; it can protect (and has protected) our ancestors from disease, illness and harm for many years. However, the diagnostic criteria for OCD, as set forth in the DSM-5, requires the presence of “clinically significant distress or impairment in social, occupational or other important areas of functioning” in order to make a diagnosis. “Clinically significant distress” means that people with OCD feel the impact of the disorder on their daily functioning and quality of life. They do not see it as something enjoyable, virtuous or beneficial. It is a debilitating disorder that makes normal tasks of living difficult to manage. A person with an OCD diagnosis is tormented every day by the “clinically significant distress” created by this monstrous disorder.
Additionally, a goal of treatment when working with people who have OCD is to engage with them in intensive exposure and response prevention (ERP) therapy. In this therapy, the person with OCD (under the guidance of a therapist) purposefully exposes themselves to the feared stimulus (i.e., germs) and then resists the urge to perform the normally performed compulsion (i.e., washing hands). Therefore, the crux of the therapy revolves around retraining the brain to sit with the anxiety and wait for it to gradually decrease, ultimately determining that the perceived threats are not nearly as bad as we thought (or do not exist at all). Describing compulsive cleaning behaviors as “evolutionary” is harmful to the person with OCD and provides reassurance that their behaviors are rational and necessary. This will ultimately impede progress with regard to overcoming OCD and improving the person’s quality of life.
Now, from just a person with OCD, this article brought up a lot of feelings for me concerning my own experience with the disorder and my treatment process. I’ve been in ERP therapy consistently for about a year and a half now. I’ve overcome many of my biggest fears through this therapy modality. But OCD still plagues me each and every day. It still makes me feel “clinically significant distress.” I would be lying if I said the coronavirus pandemic hasn’t thrown my treatment for a loop.
Doctor, I’ve spent years retraining my brain to understand the threats I perceive are not as bad as I think they are, or don’t exist at all. But suddenly, the threat is real. I am nervous about losing the progress I have made in therapy when this is all over. Many people will be able to go back to a somewhat “normal” way of living, eventually. People will slowly start shaking hands again and eating finger food again. People will stop carrying hand sanitizer everywhere. But for us who are living with contamination OCD, it won’t be that easy. We will be faced with possibly having to retrain our brains all over again. We are working tirelessly during this time to not lose the progress we have made in therapy doing ERP, while still following the necessary protocols right now due to the virus. It is a struggle, now more than ever, to not let OCD win.
Doctor, as I mentioned at the beginning of this piece, I have an indescribable amount of respect and admiration for the work you do as a psychiatrist and a professor. Working in the field of mental health is no easy task, and unpredictable life events (like a global pandemic) can test even the most foolproof and evidence-based theories of treatment (and our patience). However, I think it is important to advocate as a member of the OCD community, especially given the current events.
Struggling with anxiety due to COVID-19? Check out the following articles from our community:
- What to Do If the Coronavirus Health Guidelines Are Triggering Your Anxiety or OCD
- 8 Soaps You Can Use to Help Prevent the Spread of Illness
- How Can You Tell the Difference Between Anxiety and COVID-19 Symptoms?
- Which Face Masks Prevent Against Coronavirus?
- 6 Tips If You’re Anxious About Being Unable to Go to Therapy Because of COVID-19
Photo by Dhaya Eddine Bentaleb on Unsplash