The Mighty's PTSD Educational Resource
Editor's Note
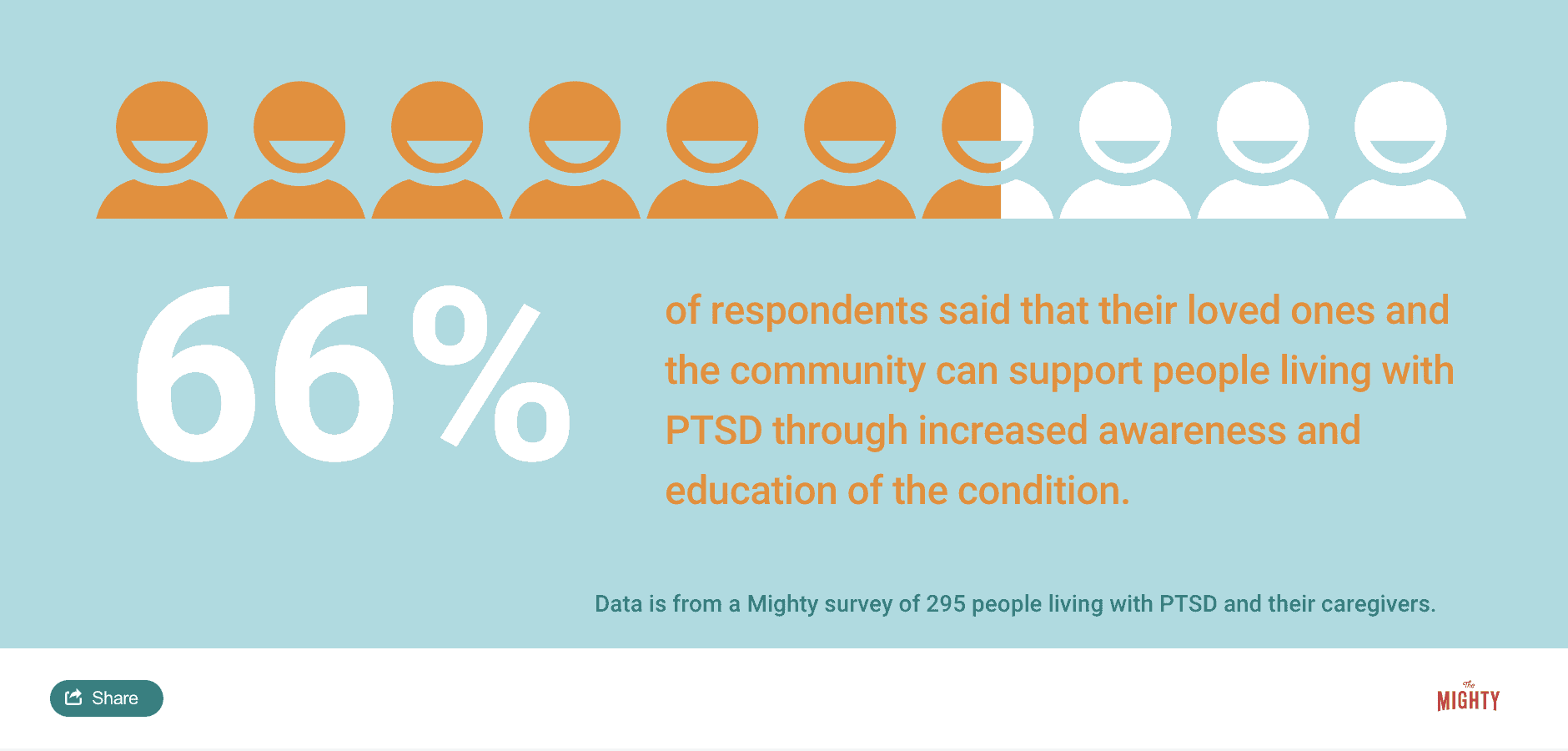
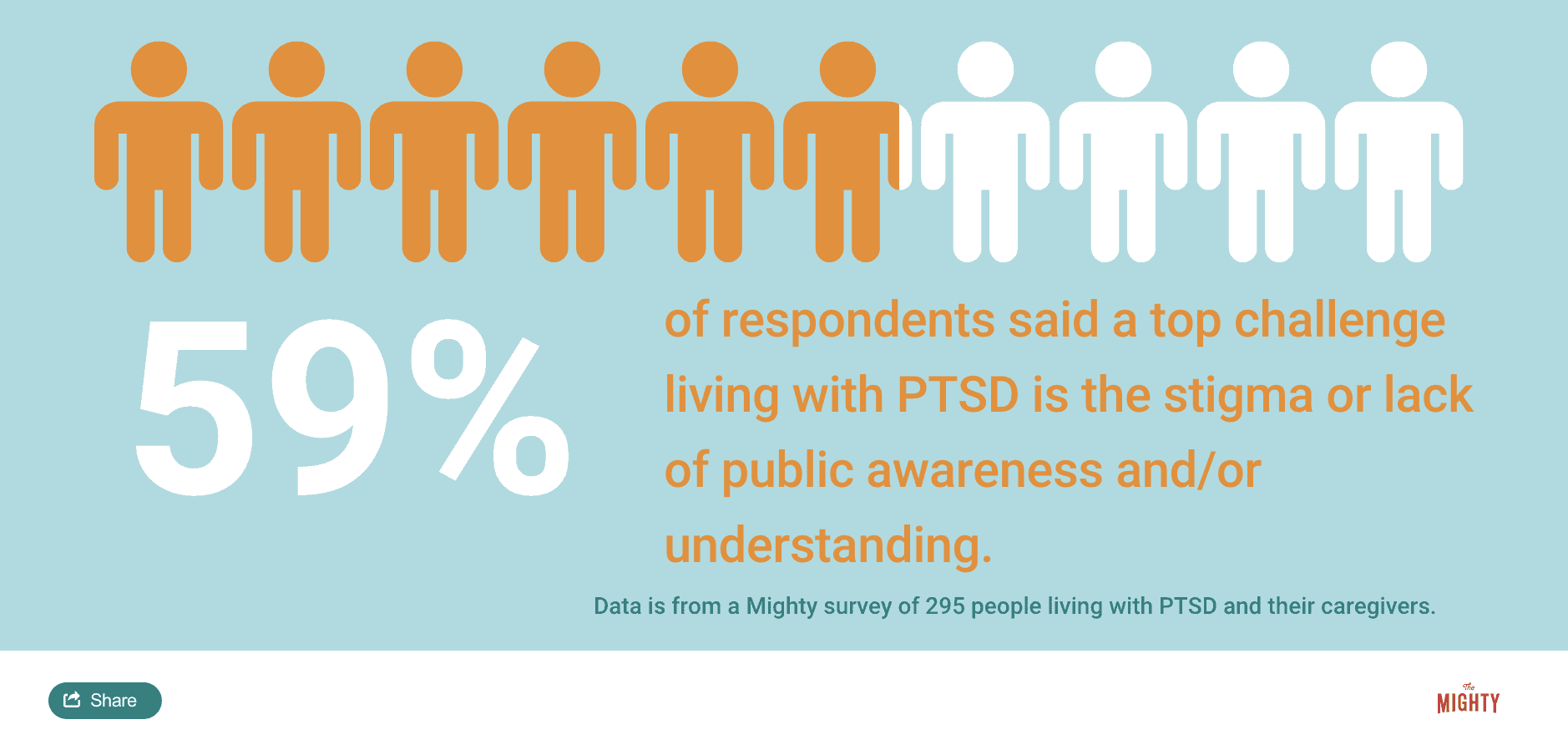
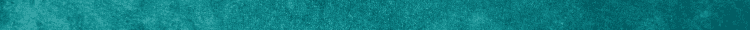
The Mighty’s educational content combine the expertise of both the medical and patient community to help you and your loved ones on your health journeys. For the PTSD Educational Resource, we interviewed two mental health experts, read the latest studies and surveyed nearly 300 people living with PTSD and their caregivers.
PTSD at a Glance:
- Post-traumatic stress disorder (PTSD) is a mental health condition that can occur after experiencing a traumatic event.
- Approximately 8% of Americans will experience PTSD at some point in their life, with the condition more common among women.
- Although PTSD is sometimes attributed with veterans, it can be caused from any traumatic event, including physical, emotional or sexual abuse, natural disasters, crime, or medical trauma.
- There are many different treatment options for PTSD, including therapy, medications and lifestyle changes, and clinical research studies continue to identify new options.
Medically reviewed by Dr. Anthony Zannas, MD, MSc, PhD.
What is PTSD? | PTSD Management | Clinical Research For PTSD | How To Talk To Others About PTSD | How To Find A Health Care Provider For PTSD | How To Support Someone With PTSD | Join A Private Group For PTSD | How To Get Help In a Crisis
What Is Post-traumatic Stress Disorder (PTSD)?
Post-traumatic stress disorder (PTSD) is among the most common mental health conditions in the United States. PTSD can develop after experiencing a traumatic event such as physical, emotional or sexual abuse, crime, motor vehicle accidents, a natural disaster or medical trauma, among others. Not everyone who experiences trauma will develop PTSD, and it’s not uncommon for the symptoms to appear months or sometimes years after the trauma has ended.
You may already know about some of the stereotypical symptoms associated with PTSD, like flashbacks. Flashbacks cause people to feel like they are re-experiencing traumatic events — they lose awareness of the present and it feels like they are back in time. Flashbacks are part of a group of PTSD symptoms known as intrusive symptoms. Other intrusive PTSD experiences can include recurrent and involuntary memories of your trauma or distressing dreams.
PTSD can cause many other symptoms, and not everyone will experience flashbacks or intrusive symptoms. Other common experiences people with PTSD have can include avoiding triggers or reminders of the traumatic event. People with PTSD may avoid people and places associated with trauma, but sometimes the triggers are more subtle. For example, you may also avoid objects (like a certain color clothing), activities or conversations that remind you of the trauma. Some people with PTSD also experience dissociation, where they feel detached from their surroundings or even their body. Some people with PTSD may also forget or unconsciously block out parts of their traumatic experiences.
Other symptoms of PTSD mimic other mental health conditions like depression and anxiety. People with PTSD may lose interest in activities they once loved, have difficulty sleeping, feel more irritable or angry, startle easily, have trouble concentrating, and experience constant hypervigilance, sometimes described as “waiting for the other shoe to drop.”
Sometimes the symptoms of PTSD go beyond what’s traditionally considered PTSD and may include additional symptoms like difficulty regulating emotions, significant distrust of the world, suicidal ideation and feeling different or separate from other people. This is referred to as complex post-traumatic stress disorder (C-PTSD), and is more common among people who have survived chronic or ongoing trauma at some point in their life.
Read more about PTSD symptoms from fellow Mighties here:
- Fawning: The Fourth Trauma Response We Don’t Talk About
- 12 Life-Impacting Symptoms Complex PTSD Survivors Endure
- What Happens When Repressed Memories of Trauma Begin to Resurface
What Causes PTSD?
PTSD is a condition that can be caused by experiencing or witnessing a traumatic event such as physical, emotional or sexual abuse, crime, a natural disaster, serious injury or death or combat. It is normal to experience a fight-flight-freeze survival response during a scary or dangerous situation. Not everyone will develop PTSD, however, for some people the trauma and related symptoms don’t go away and interfere with their daily life. They are eventually diagnosed with PTSD.
Sometimes there is a misconception that the traumatic event or events that lead to a person’s PTSD must be violent or related to military service. Although combat-related PTSD is probably the most widely recognized form of PTSD, most people who experience PTSD are not military veterans. In our PTSD survey, 6% of Mighty members said that their PTSD was related to “war and conflict.” It was the least common cause of PTSD reported on our survey.
The most common cause reported by 67% of our members was a form of abuse during childhood. Some of our members attributed their PTSD to causes such as loss of a loved one (35%) or a serious medical issue (33%). A person’s PTSD may have multiple causes and can sometimes lead to complex PTSD (C-PTSD). The symptoms of C-PTSD are similar to PTSD but can include additional symptoms like difficulty regulating emotions. Seventy-eight percent of our members identified their PTSD as chronic or complex.
Check out these resources for more information about potential causes of PTSD:
- “The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma” by Bessel van der Kolk M.D.
- “Waking the Tiger: Healing Trauma” by Peter Levine
- International Society For Traumatic Health Studies
- Sidran Institute
- CDC-Kaiser Permanente Adverse Childhood Experiences (ACE) Study
Common PTSD Misconceptions
PTSD is often represented in the media as exaggerated, showing only one or two symptoms (often flashbacks) and portraying a quick recovery. You may have seen shows where characters have PTSD and after “facing their fears,” they no longer experience PTSD symptoms.
But those living with PTSD know the condition is not straightforward and recovery isn’t just about “facing your fears.” To learn more about PTSD misconceptions, we reached out to The Mighty community to learn about what they wish others knew about PTSD.
Here’s what they had to say:
- “[PTSD] triggers are very unpredictable. What you can manage today can be overwhelming tomorrow.”
- “Please stop assuming that if I have PTSD, it’s due to a military background. There are many, many other ways to get PTSD, but it’s embarrassing when people say, ‘Military?’ and I have to say, ‘No.'”
- “The exhaustion and fatigue that comes with the constant fighting within your soul, heart, mind and body fighting to survive and function.”
- “[PTSD] is real [and] it’s not going away just because my trauma was some time ago.”
- “It’s a very invisible illness that I will be managing the symptoms of for my entire life and it affects every aspect of myself (emotionally, mentally, and physically).”
You can also read stigma-busting stories about PTSD here:
- PTSD Affects First Responders Too–Hear One Story
- Why Trauma Survivors Shouldn’t Think They Are ‘Lazy’
- Why Trauma Survivors Can’t Just ‘Let It Go’
PTSD Management
Although the symptoms of PTSD seem overwhelming, you can recover from the condition and heal from your trauma. The first step to PTSD management is finding someone you feel safe with to talk about your experiences, whether that be a doctor, therapist or a loved one. Seeking treatment may sound scary, especially since trauma and PTSD generate so much fear. The process, even though it may be difficult at times, is worth it.
Lauren Rockwell, Mighty contributor and trauma expert, said:
“Trauma can feel like carrying a heavy weight. Imagine that someone tells you to hold a bowling ball only with your right hand and walk for ten miles. That would be a very difficult endeavor. Now, imagine someone gives you an ergonomic backpack to hold the ball. It still feels heavy, but over time, you gain muscle and the task becomes a little bit easier. The purpose of finding treatment for PTSD is to develop tools to help carry trauma in a way that’s not debilitating, so that you can focus on other important parts of your life.”
There are many tools people living with PTSD can explore on their own and with the help of a therapist or other health care professionals. Because each person’s trauma and PTSD is unique, everyone’s “toolkit” will look different. That’s why it’s important to not compare one person’s recovery journey to another’s.
Some tools and techniques used to help manage PTSD include trauma therapies, medications and lifestyle management strategies.
Trauma-focused therapies use different approaches to help you process your emotions, thoughts and memories around the event or events that caused your PTSD. There are several different research-backed approaches to trauma therapy for PTSD. Here are just a few:
- Prolonged exposure therapy (PET) helps you gradually face the triggers you avoid to reduce trauma-related fears and reactions. In this form of therapy, you and a therapist slowly face trauma-related memories, feelings and situations. In this way, you (and your body) will learn not to fear or avoid reminders of past trauma, which can help reduce your PTSD symptoms.
- Cognitive processing therapy (CPT) can help you change negative thoughts and beliefs connected to your trauma. A therapist will help you understand how your trauma affects your thoughts, feelings and beliefs. You will work to reframe your thoughts and beliefs around the trauma as well as learn adaptive coping strategies to manage difficult trauma reminders when they pop up.
- Eye movement desensitization and reprocessing (EMDR) is another therapy that can improve PTSD symptoms. EMDR helps you process traumatic memories using a technique that likely mimics how your brain organizes memories in REM sleep. During EMDR with a therapist, you will recall traumatic memories while you move your eyes bilaterally (left-right) or use other forms of bilateral stimulation like tapping. EMDR helps many people shift their trauma so it no longer causes present-day distress.
Medication therapies can be used to help reduce PTSD symptoms. Usually, you will be prescribed medications that are also used to treat depression and anxiety. Most commonly, doctors prescribe selective serotonin uptake inhibitors (SSRIs) or serotonin-norepinephrine uptake inhibitors (SNRIs). These medications are typically prescribed by a psychiatrist or a general practitioner.
Self-care and lifestyle changes can also help manage PTSD symptoms. To learn more about what management strategies have helped people living with PTSD, we reached out to the Mighty community. Here’s what they had to say:
- “I do adult dot-to-dots. They are harder than the little kid ones — you have to pay so much attention it helps distract your mind and it works almost every time.”
- “I manage my outbreaks of anger with sensory distractions. If I am feeling very angry and tense (a symptom of my PTSD), I grab the fluffiest and softest blanket I can find and wrap myself in it. The softness of the blanket just kind of calms me.”
- “Sewing, knitting, crochet or really any hands-on craft. It helps keep my mind focused on one task instead of my symptoms. Oh, and cooking, definitely cooking.”
- “I engage in positive self talk. I remind myself that the current situation [I’m in] isn’t [the same] situation that caused the PTSD. I also sometimes do a ‘reality check,” i.e. ‘Today is (name of day), I am (name of activity) at (name of place).’ It tends to help bring me back to earth.”
- “Dim lights make me feel less overstimulated.”
- “Yoga with Adriene on Youtube.”
- “Making a few daily habits helps me a lot, like creative writing and exercise. It helps provide me with some consistency in my day when everything feels chaotic.”
- “Spending time in nature reduces my stress. Just even sitting outside in the sun for a few minutes helps. I like gardening because I feel like I’ve accomplished a task and have spent some time outside.”
A common theme among the individuals interviewed about PTSD was the importance of tracking symptoms and being able to recognize the mental, physical and emotional factors related to PTSD. Recognition of symptoms is an important step in managing any condition or disorder, which is why we created this PTSD-specific symptom tracker to help support you on your recovery journey:
![]()
You can also find other management resources here:
- Coping strategies from The National Center for PTSD
- Meditation tips for PTSD
- Coping With Trauma-Related Dissociation by Boon, Steele and van der Hart
Clinical Research for PTSD
Clinical trials are research studies that investigate the use of medications, diets, therapies, treatment devices or diagnostic tests for health conditions. Sometimes people are dissatisfied with currently available treatment options for their diagnoses or the side effects of their treatment. Sometimes there just aren’t enough effective treatments available. These people may find participating in a clinical trial beneficial. Individuals may also want to help advance research for health conditions they care about. You may see these trials referred to as clinical studies, clinical research studies, studies and research.
Clinical research studies aren’t limited to physical health conditions. There are many clinical trials for mental health conditions, too. If you want to explore other options for possible relief of your PTSD symptoms, you may want to consider participating in a clinical trial or research study.
To learn more about clinical research, please ask your doctor or visit:
What Does PTSD Recovery Look Like?
So what does PTSD recovery actually look like? Lauren Rockwell, Mighty contributor and trauma expert, said people living with PTSD often focus on symptom management and coping techniques:
“Treatment can help lessen trauma symptoms. Therapy can be incredibly helpful in this process by helping you recognize your symptoms, identify your triggers, be able to predict better whether a situation will worsen or resurface symptoms and ultimately, improve your ability to manage your trauma symptoms.”
What managing symptoms looks like day-to-day depends on the therapy goals you set with your therapist and health care team. Liscenced psychotherapist and trauma expert Annie Wright, LMFT, says:
“The first thing you and your therapist should do is set your therapy goals and define what success looks like together. A good therapist should be creating a treatment plan for you based on those goals, and actively checking in helping you move towards them.”
Recovery from trauma can take time and it’s not something that can be “fixed” overnight. If you’re feeling frustrated that your trauma recovery is taking longer than expected, Wright shares this reminder:
“It’s very important not to try and force yourself into change too soon. Treat whatever symptoms you have with respect. Because when you blast through them, when we try and create change too fast, you can run the risk of retraumatizing yourself. It takes time, but change is possible.”
How To Talk To Others About PTSD
Talking about PTSD can be difficult, especially when each person’s experience with the condition varies. We created this worksheet to help you break down and define the more nuanced aspects of your life with PTSD for those in your support system: friends, family, coworkers or even health care professionals. Here you can identify your triggers, how you like to be distracted when you’re overwhelmed and even what someone can do to best support you when you need it most.
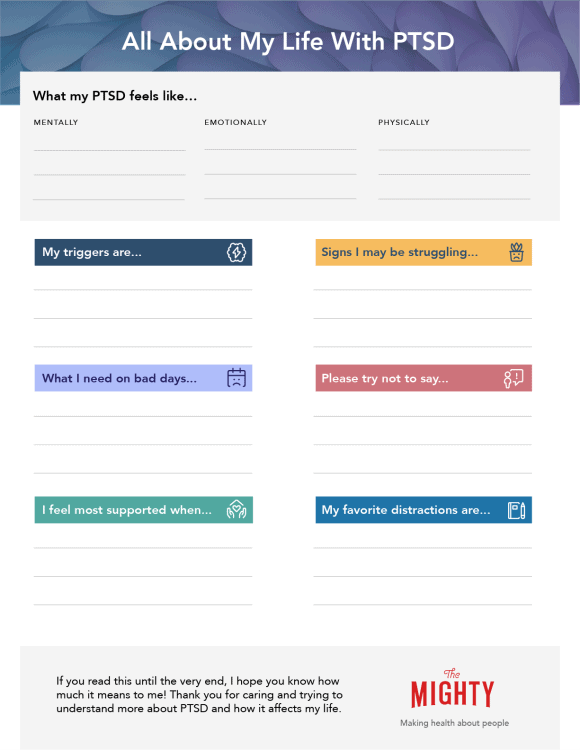
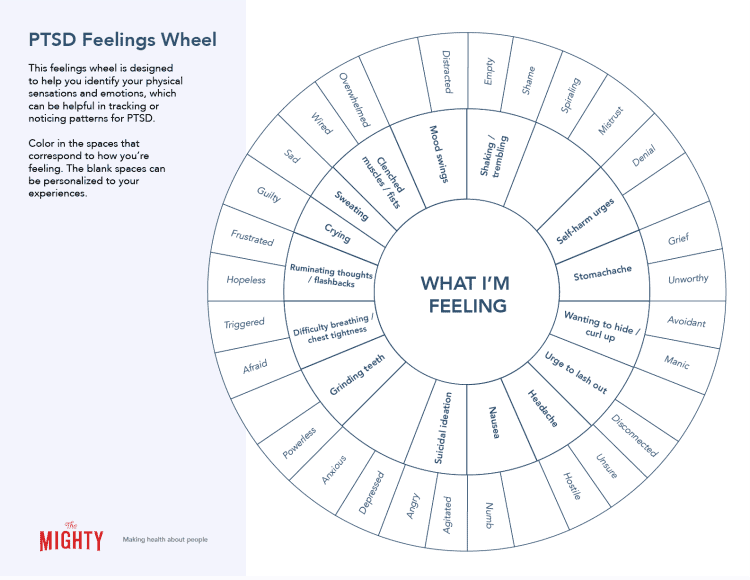
Identifying and attributing emotions to specific events or physical symptoms can be especially tough when your PTSD is triggered. To help in those moments where you might need extra support, we created this Mighty feelings wheel with common physical sensations and emotions associated with PTSD. It’s a great visual tool for sharing with loved ones or someone on your treatment team. As a bonus, coloring in the sections that best match what you’re feeling can be a welcome distraction, too!
Talking To A Health Care Provider About PTSD
The idea of finding a health care provider to help manage PTSD symptoms can feel overwhelming at first and you may be asking yourself these questions about the process:
- Who is the best person to help me with PTSD?
- Will they understand what I’m going through?
- There are so many different types of mental health professionals — which one is best for PTSD?
- How do I find a therapist?
- How do I know a therapist is a good fit for me?
If you’re in need of a little encouragement during this process Kevin Varner, MA, NCC, LPC, want you to know:
It takes courage to be vulnerable, to ask for help, to do something for the first time, and that’s okay–all of you is welcome here.
How To Find A Health Care Provider For PTSD
Each person on a PTSD health care team has an important role to play in trauma recovery. How you assemble this team will vary for everyone. A general practitioner is often the “gatekeeper” to other professionals who specialize in PTSD. However, depending on the type of insurance you have, you may be able to make appointments directly with mental health specialists who can help with PTSD symptoms.
It’s important to know that different mental health professionals will manage PTSD in different ways. For example, a psychiatrist is an M.D. who can prescribe medications for mental health conditions. Medications may play an important role in trauma recovery, and having a good relationship with a psychiatrist can be helpful in finding the best medication to fit your needs.
Another important person to help with trauma recovery is a therapist. Therapists can help someone process trauma through non-medication methods. Every therapist has a different way of working and may use structured therapy techniques shown to help trauma, like prolonged exposure therapy (PET) or eye movement and eye movement desensitization and reprocessing (EMDR).
Searching for a therapist can feel like trying to find the perfect pair of jeans. It is completely normal to “shop around” for a therapist who fits your personality and needs the best. A good therapist won’t get frustrated or mad if they aren’t chosen after the first meeting, or even after several meetings. They know that processing trauma is difficult and finding a good fit is key because they will help work through some of the most important and difficult moments in a person’s life. When looking for a therapist to help with PTSD symptoms, the most important thing is to make sure you find someone you feel safe around.
Next, it’s important to find someone who is properly credentialed and trauma-informed. Any therapist you work with should have a license from your state in good standing. Every state has a database where you can double check a therapist’s license. In addition, trauma therapy is a specialized version of therapy, and trauma-informed therapists take additional classes to receive advanced training. Know that therapists who have trauma training are not always private practice therapists — public and community centers for mental health also have trauma-informed therapists on staff.
If a trauma-informed therapist isn’t located nearby, you still have several options. Sometimes a therapist is willing to work on additional trauma training to best support your needs in treatment or will work with a supervisor or mentor who does have trauma training. You can also consider telehealth with a trauma-trained therapist anywhere in your state. While telehealth may feel less personal at first, it can be more accessible than a traditional office location. Telehealth visits allow a person to control their environment and can make it a more comfortable place to have a therapy session.
Starting the search for a therapist can be done online and contacting an office to set up an appointment doesn’t always require a phone call: Some offices can make appointments through online forms and even email. You can also ask your general practitioner to make you a referral to someone they’d recommend and if you have insurance, the company will have a list of therapists you can contact who accept your insurance.
To begin the search online, you can search for local therapists using the search functions on these websites:
- Psychology Today Therapist Finder
- GoodTherapy Therapist Finder
- ISSTD Therapist Finder (trauma-specific database)
It can be nerve-wracking to go to your first therapy appointment — this is normal! Discussing trauma-related symptoms for first time (or even 10th time!) can be difficult. That’s why we created a downloadable discussion guide to help you prepare for a visit with a health care professional about PTSD. We hope this guide helps you get the most out of your appointments:
PTSD Health Care Provider Discussion Guide
How To Support Someone Living With PTSD
Behind every person living with PTSD, there is a caregiver or support system willing and wanting to help. We recognize it can be hard to know where to begin, so that’s why we went straight to the source.
Here’s some advice from Mighties living with PTSD:
- “One word: validation.”
- “I need lots of encouragement and patience when I am struggling. Words or phrases like ‘You have got this’ or ‘I am proud of you.’ Reminding me that I am strong and they will not abandon me when I am struggling. Just being there because they love me.”
- “Too often people say they are ‘here for you’ but don’t give you the space and time to talk, or dismiss how you’re feeling or your experience. I wish they would understand that time doesn’t always heal. Some days a trigger will take you right back to that moment and there’s nothing you can do about it [and] in those moments the best thing is to talk.”
- “Don’t tell us to ‘stay calm’ or that there’s ‘no reason to cry’ (or whatever emotions we have).”
- “A lot of people can be overwhelmed when a loved one is experiencing a trigger. Just be there for them. You probably don’t even have to say anything. Just your presence is calming enough.”
- “Remind them they are safe. Understand that each day, hour or minute can be different. Hold them when they need it. Be encouraging – remind them where they were before and how much further they are now. Remind them that their brain has suffered an injury [and that] they are not broken, they are recovering.”
- “Educate yourself about PTSD.”
- “Ask ‘how can I help?'”
Join a Private Community for PTSD
If you live with PTSD or trauma symptoms and want to connect with other Mighties who’ve been there, check out The Mighty’s private PTSD community. Join the conversation around PTSD and trauma, learn more about PTSD resources, and become part of a PTSD family who gets it.
In this private community, you’ll find:
- Monthly themes
- Downloadable resources
- Community discussion prompts
To join the community, click here.
How To Get Help In a Crisis
If you find yourself feeling so overwhelmed and hopeless that you don’t want to live anymore or you’re making plans to die, reach out for help immediately. You are valuable and important. You’re not alone. Call a loved one or your therapist or reach out to a crisis hotline:
If you are feeling suicidal, there is hope.
- You can call the National Suicide Prevention Lifeline 24/7 at 1-800-273-8255
- You can reach the Crisis Text Line 24/7 by texting “START” to 741-741
- You can call The Trevor Project, an LGBT crisis intervention and suicide prevention hotline, 24/7 at 1-866-488-7386
If you are hard of hearing, you can chat with a Lifeline counselor 24/7 by clicking the Chat button on this page, or you can contact the Lifeline via TTY by dialing 800-799-4889.
To speak to a crisis counselor in Spanish, call 1-888-628-9454.
Head here for a list of crisis centers around the world.
For additional resources, see the American Foundation for Suicide Prevention and SAVE (Suicide Awareness Voices of Education).
You can read the following stories from people who’ve been there:
- If You Feel Like You’re ‘Losing’ to Your Mental Illness, This Is Your Reason to Stay
- For When Your Only Thought Is Suicide
- The Difference Between Wanting to Die and Wanting the Pain to Stop
- Dear Suicidal You
And for additional messages of hope, click here.
You are not alone.
This PTSD Educational Resource was created with support from many Mighty contributors, medical experts and therapists. You can learn more about the individuals interviewed for the creation of this resource here:
- Annie Wright, LMFT
- Kevin Varner, MA, NCC, LPC
- Lauren Rockwell, MA, LPA
- Vicki Peterson, Mighty Super Contributor
- Hilda Antje Vanderheide, Mighty Leader
- Megan Glosson, Mighty Leader
- Amelia Blackwater, Mighty Leader
- Leslie A. Zukor, Mighty Leader
And to the 200 Mighties who took our PTSD survey and our Mighty community who answered community prompts to help inform this resource, thank you!
1VA.gov: Veterans Affairs. (2018, September 13). Retrieved from https://www.ptsd.va.gov/understand/common/common_adults.asp
2Lancaster, Cynthia, et al. “Posttraumatic Stress Disorder: Overview of Evidence-Based Assessment and Treatment.” Journal of Clinical Medicine, vol 105, 2016
3Roberts, Andrea L., et al. “Witness of Intimate Partner Violence in Childhood and Perpetration of Intimate Partner Violence in Adulthood.” Epidemiology, vol. 21, no. 6, 2010, pp. 809–818. JSTOR, www.jstor.org/stable/20788233.
4Attfield, Kathleen R., et al. “Injuries and Traumatic Psychological Exposures Associated with the South Napa Earthquake — California, 2014.” Morbidity and Mortality Weekly Report, vol. 64, no. 35, 2015, pp. 975–978. JSTOR, www.jstor.org/stable/24856765.
5Green, B. L., Epstein, S. A., Krupnick, J. L., & Rowland, J. H. (1997). Trauma and medical illness: Assessing trauma-related disorders in medical settings. In J. P. Wilson & T. M. Keane (Eds.), Assessing psychological trauma and PTSD (p. 160–191). The Guilford Press.
6 “Summary and Recommendations.” Quality of Care for PTSD and Depression in the Military Health System: Phase I Report, by Kimberly A. Hepner et al., RAND Corporation, 2012, pp. 91–104. JSTOR, www.jstor.org/stable/10.7249/j.ctt1b3h9mp.14. Accessed 10 Oct. 2020.
7Ibid
8What Is Posttraumatic Stress Disorder? (n.d.). Retrieved from https://www.psychiatry.org/patients-families/ptsd/what-is-ptsd
9Schiavone, F. L., Frewen, P., McKinnon, M., & Lanius, R. A. (2018). The Dissociative Subtype of PTSD: An Update of the Literature. Retrieved from https://www.ptsd.va.gov/publications/rq_docs/V29N3.pdf
10Symptoms of PTSD. (n.d.). Retrieved from https://adaa.org/understanding-anxiety/posttraumatic-stress-disorder-ptsd/symptoms
11Ibid
12Ibid
13Prolonged Exposure (PE). (n.d.). Retrieved from https://www.apa.org/ptsd-guideline/treatments/prolonged-exposure
14Cognitive Processing Therapy (CPT). (n.d.). Retrieved from https://www.apa.org/ptsd-guideline/treatments/cognitive-processing-therapy
15VA.gov: Veterans Affairs. (2018, August 10). Retrieved from https://www.ptsd.va.gov/understand_tx/emdr.asp