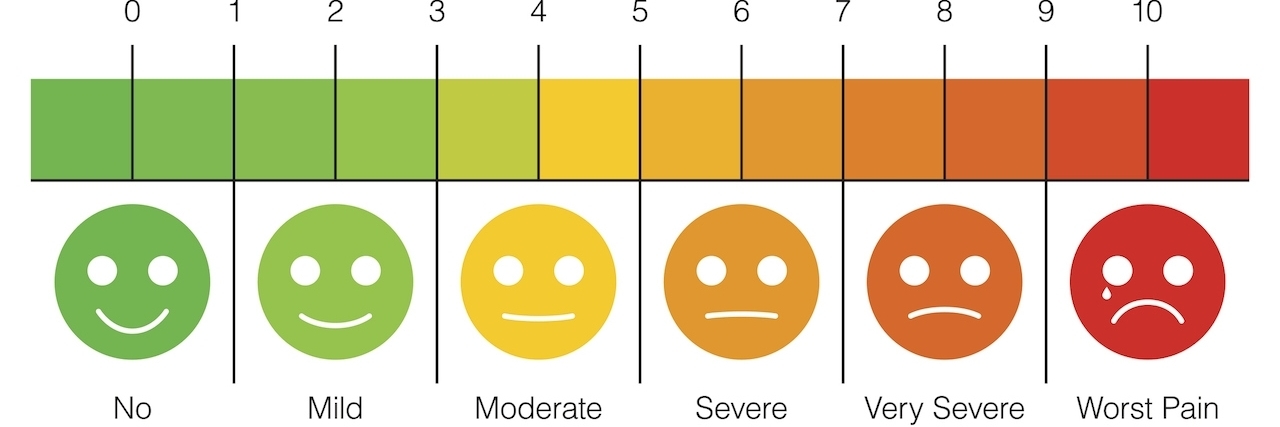
If you’ve ever visited a medical facility with the complaint of “pain” they’ve probably asked you to rate it on a scale of one to 10, with one being no pain at all and 10 being the worst pain imaginable. This question was probably difficult to answer, even if they showed you the chart with the faces. I might even venture to guess that unless you are someone who has dealt with a good variety of pain, you could be rating a cold as high as an 8 — and, unless you are dying of it, it is probably unlikely to help the doctor that you think a cold is an 8. However, because so many people cry wolf in this way, it could mean serious things are being majorly overlooked.
I am by no means a medical professional, but I’ve had to fine-tune my answer to this question over many years. I find that if I feel perfectly normal (hah!) I’m a one, so almost never. My baseline is maybe two or three, implying in my head that things hurt but I’m used to it and it is in no way an emergency. If I make it to a five I’m in a lot of pain — you know, the “stabby” kind or “I just woke up and feel like I got run over by a bus” kind (no, not literally. See how hard it is to explain pain?). Anything above a seven should at least land me in a doctor’s office, if not a hospital, like that time I had a kidney infection — a solid seven there. I tried to convince myself I could push through the pain. As it turns out I could not (only made it two hours — actually five if you count the ER visit, but still, I felt like a wimp!).
I also like to always compare my pain to the times when it was so bad I was throwing up. I figure that might be an 8.5 (10 numbers only seem like too many until you can’t decide…) And I’ve never experienced this, but I’m going to put gunshot wound as a 10, because I cannot imagine the physical pain that would put me in but I do know it would be a lot, and that television characters probably don’t express nearly enough pain when they are shot.
But that’s just how my mind works with this system. Now to be fair, I’ve had nurses tell me that what I describe and the numbers I allot to said pain are what they think should be accurate, so maybe I’ve conquered the system. Of course, in praising me they always seem to have all those people in mind who think their cold is an eight. So maybe it’s just a hard system to decipher.
Unfortunately, I don’t have much to offer up in terms of alternatives. I myself have a hard time describing a type of pain unless it is “stabby,” because sometimes “dull” doesn’t seem like enough and any other term is not what I’m looking for (“achey” apparently just implies that there is pain that is not “stabby”).
One things is for sure, though, I can always tell you if something is in pain and if it is in more pain than before. Wait no, that’s not right. I can’t do that, either.