Alison Darcy, PhD, wants to make therapy accessible — so accessible, in fact, all you have to do is log in to Facebook. Woebot, Darcy’s brainchild, is a chatbot that delivers cognitive behavioral therapy (CBT), one of the most widely used types of evidence-based therapy for mental illness, through Facebook messenger.
“I think people are talking about [mental illness] a lot more, which is great,” Darcy, a Stanford-trained clinical research psychologist as well as the CEO and founder of Woebot, told The Mighty. “At the same time we live in this really connected world where so much information is available at our fingertips, and we’re drowning in apps, but we still haven’t really solved this issue of getting really good care into the hands of people in a way that integrates seamlessly with their life.”
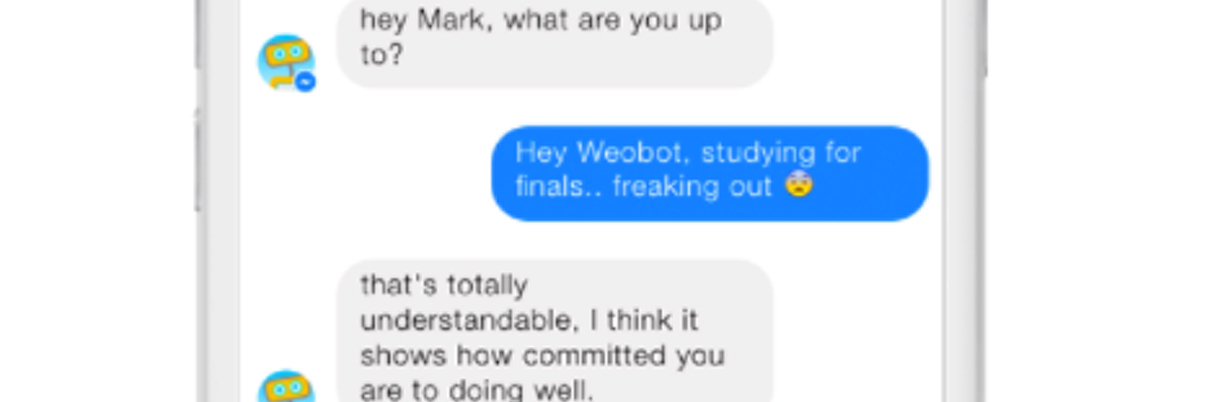
Woebot, Darcy hopes, will fill this void. Through Facebook messenger, Woebot checks in with you every day, asking questions about your day and how you are feeling. After a week of check-ins, Woebot provides users with a mood chart so they can see their progress or identify difficult periods over time. And unlike traditional therapists — humans who need to sleep — Woebot is available all day, every day.
“What I really like about CBT is that it is real practical, it’s really about problem-solving,” Darcy explained. “It’s about looking at the thought patterns you have now and the behavior patterns that you have now that are undermining you on a day-to-day level… As [Woebot’s] getting to know you, he teaches you things, and that relationship kind of builds over time and he challenges you.”
Woebot was originally designed for college students, but Darcy believes the app has the potential to help anyone interested in CBT. “I think anybody who actually likes the idea of CBT therapy could benefit from Woebot,” she said, adding:
It goes back to this conversational style, it’s just very easy and flowing. Personally speaking, I find that it’s easier for a robot to play a word game with you as a way of teaching you what a cognitive distortion might look like then it has been to semi-lecture somebody in the context of an actual therapy appointment.
From the data Darcy has collected, she’s found those who use Woebot see results faster than with other forms of CBT. In a small controlled study conducted by Darcy and several colleagues, those using Woebot reported a significant reduction in their depression and anxiety as compared to those who used self-help books for two weeks. “One of the really significant things about that is that when you look at the [results], it usually takes about four to five weeks to see that kind of a response to traditional, in-person therapy,” she added.
While there are many mental health apps available, Darcy says Woebot is the only chatbot that uses CBT. Another chatbot, Joy, launched last year, can also track your mental health, using Facebook messenger to send you daily check-ins and different coping strategies.
Those interested in using Woebot can try the chatbot for free using Facebook messenger. After the two-week trial periods ends, Woebot continues at a rate of $39 per month. The cost, Darcy explained, works out to be less than 5 percent of the cost of other standard CBT therapies and around 40 percent of the cost of most copays.