Most of the time, my pain is invisible. It aches, stabs, burns in my joints (or other places), tucked away where no one can see. It keeps me up at night or makes me whimper in my sleep as I turn over, where only my husband can hear. It lies behind a straight face with maybe an occasional grimace. Sometimes it’s the reason behind fashion choices like loose pants that may seem like eccentric, oblivious-scientist choices to others. It may look like restless fidgeting when I try to get comfortable, often shifting between positions as each previously-fine position quickly becomes not-fine.
• What is Ehlers-Danlos Syndrome?
• What Are Common Ehlers-Danlos Syndrome Symptoms?
Pain that is invisible brings its own set of challenges. In fact, pain alone, by itself, is inherently invisible. As Elaine Scarry wrote in “The Body in Pain,” “to have great pain is to have certainty; to hear that another person has pain is to have doubt.” This is clear even in the way that doctors and other clinicians ask patients to rate and describe pain. I hate rating my pain on a scale from one to 10, even though just about every clinical visit where pain is brought up requires it – and even though I have even gotten used to it and even begun thinking of my pain in numbers. But there is no way to calibrate my personal pain scale to someone else’s, or to some universal scale. I never know if the number or description I give to the doctor is understood as something worse, better, or just different than I intend.
In fact, as a side note, research has shown discrimination exists in the treatment of pain for different groups, such as women. Studies have found that women’s pain tends to be treated less aggressively despite reporting higher severity, that for acute abdominal pain despite similar reported pain scores women tend to be less likely to receive opioid painkillers and tend to wait longer for pain treatment, and that the perception of women with chronic pain is that doctors tend to be biased in their treatment of their pain because of their gender. If pain were not subjective, there would be less reason for these disparities. (Disparities in health and healthcare have also been found for people who are less wealthy/are socioeconomically disadvantaged, are not white, or are not heterosexual. The New York Times also has a nice overview of this issue: “When Doctors Downplay Women’s Health Concerns” by Camille Noe Pagán.)
The invisibility of pain can also be annoying or frustrating in day-to-day life. For example, I mostly do fine walking. Standing, though, has become more problematic for my hips and knees. And standing on a moving train? My hips and knees can pop out all over, which can be very painful. But on the (relatively infrequent) occasions where I take the subway, this isn’t obvious from the outside. I look like any other young woman. People aren’t jumping up to offer me their seats, the train conductor doesn’t use the intercom to remind people to give up priority seating to the elderly or disabled when I board, and when a seat frees up I’m in the same pool as everyone else when it comes to trying to politely and without making eye contact leap over and around each other to be the first to snag it. Of course, I wouldn’t consider myself as bad off as some others who need a seat on a train and who might obviously qualify for priority seating. But my point is that from the outside, none of the internal battle is obvious. People can’t see from the outside that I might need that seat a little more than the average young woman around my age. Then again, I also can’t see from the outside who might need that seat more than me.
However, when my invisible pain becomes somewhat visible, even just for a little while, I don’t really like it. When someone asks me if my neck is OK because I have my heating pad on it at work, I hate the attention and the awkwardness of trying to figure out how to answer. I usually just say, “Yeah, it’s fine,” and quickly change the subject.
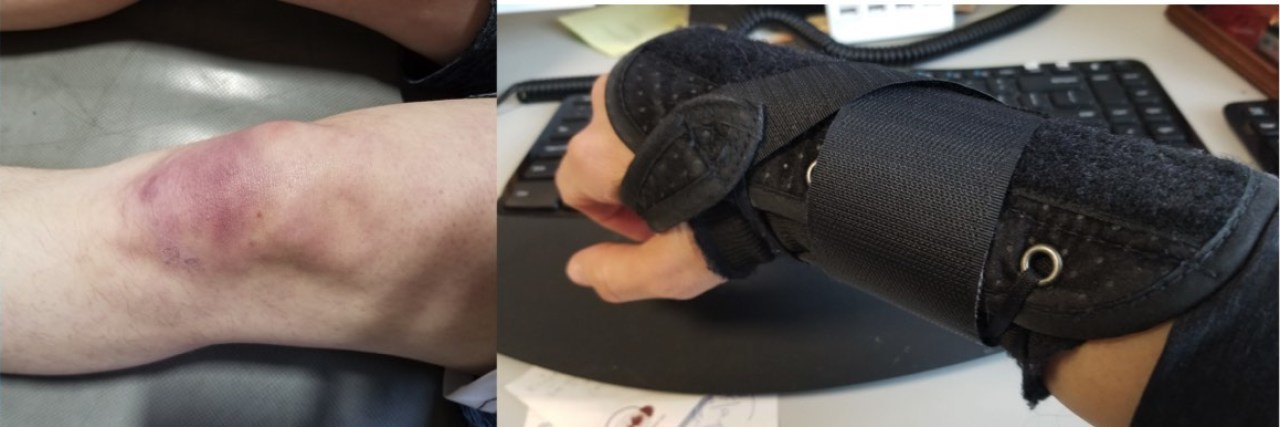
In college I became known as someone who always had bruises on her knees and legs even though I almost never had a clear reason or memory of getting one, which mostly was funny but occasionally was annoying or confusing. When I have tape on a joint, or a small brace, I hate the question, “What’d you do?” I recognize that people are simply trying to politely express concern and/or compassion in culturally appropriate ways, but I never know how to answer. Options that flit through my head often include:
“I didn’t do anything.”
“None of your business.”
“Saved two children, an old woman, a kitten, and three puppies from a burning building.”
“Was born with bad genes. You?”
Even friends who are somewhat aware of my pain but maybe aren’t my usual confidant, if they ask whether my back is hurting when they notice my restless fidgeting and re-positioning in a seat, it can feel awkward.
I’ve thought a bit about why this is, and I don’t know if I really know the answer, but I think that it is at least partly the result of warring emotions and drives within me. And I would assume within others who share similar issues and dilemmas. One is that I don’t like looking “other.” Very few people do. It’s probably at least partly an evolutionary trait. We don’t like to stand out, and specifically we don’t like looking weak. On the other hand, when we might need assistance or compassion, we maybe do sort of kind of want that to be clear. Communities can come together around those who need help and support them, and when we’re hurting it’s natural to want that. When friends get together to take turns cooking meals for their friend who just had a baby, or just moved, or just broke a leg, it is wonderful and helpful and it makes you feel good and wanted and important. Of course, chronic pain and/or illness can be a bit of a special situation, one that societies and cultures aren’t necessarily great at handling – what about when the problem never goes away? But it still makes me feel simultaneously cared for and embarrassed when one of my friends offers me a more comfortable chair in her home “for my back.”
I’m trying to be more comfortable with openly using aids like braces or tape or heating pads. I remind myself that it is silly to sacrifice my own comfort and health for the sake of other people’s thoughts or comments. When people ask about it, I’ve even been trying to work up the courage to talk to them about why I might need these things (when it’s appropriate). Awareness is a good thing. But it can still be draining educating others, answering the same questions over and over, dealing with sometimes nosey people, and fighting embarrassment.
This story originally appeared on The Chronic Athlete.