13 Things to Know About Getting Diagnosed With Rheumatoid Arthritis
I had never heard of rheumatoid arthritis before being diagnosed in 2015 at 31 years old. I started experiencing flare-ups five years earlier when my primary care doctor referred me to a rheumatologist due to my family history of lupus (another autoimmune disorder). A couple of years later, after a lot of tests, additional specialists, and lots of confusion, the rheumatologist landed on my diagnosis: seronegative rheumatoid arthritis.
I can’t say the diagnosis was helpful in understanding my condition. I left the doctor’s office with prescriptions, being told the importance of taking them, a follow-up date, and yet no knowledge of what rheumatoid arthritis was or what it meant to live with an autoimmune condition. Every day I’m still learning what it means for me to be living with rheumatoid arthritis since being diagnosed.
Here’s what I’ve learned so far that I wish I would have known six years ago about getting diagnosed with rheumatoid arthritis.
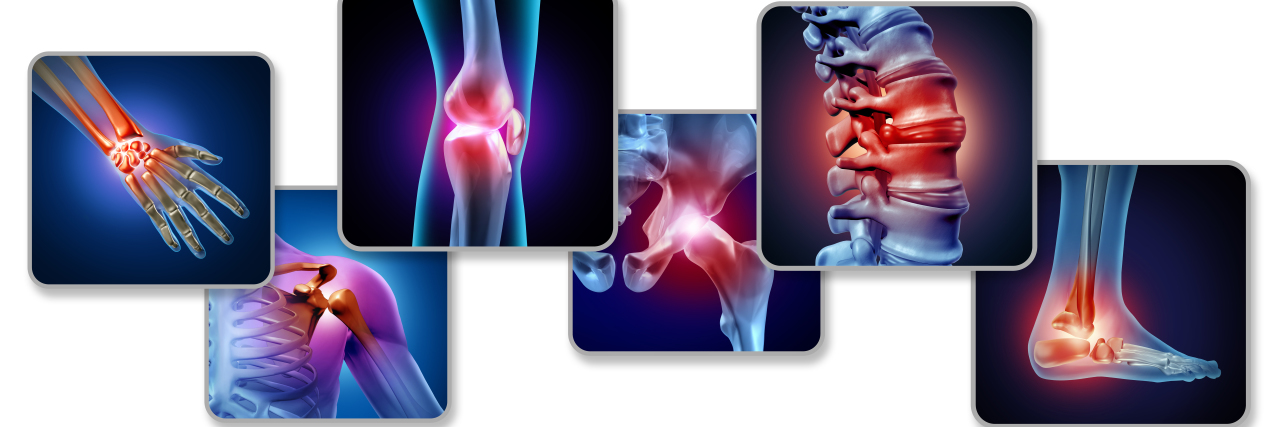
1. Rheumatoid arthritis is a chronic autoimmune and inflammatory condition where the immune system does not work properly.
It causes inflammation of the joints as well as other symptoms, and can affect people of all ages.
2. There are multiple types of rheumatoid arthritis, including seropositive, seronegative, and juvenile rheumatoid arthritis.
3. Seronegative RA does not present with a positive RA factor or the antibody anti-cyclic citrullinated peptide (anti-CCP) in a person’s blood work.
Seropositive RA means either the RA factor or anti-CCP is present. A rheumatologist will be able to tell you which kind you have and how they came to that conclusion.
4. A rheumatoid arthritis diagnosis can happen quickly or take a long time.
Sometimes it comes quickly. Sometimes it can take a while. For some people, the diagnosis may change over time such as a seronegative RA diagnosis changing to a seropositive RA diagnosis.
5. Rheumatoid arthritis symptoms can be mild or debilitating.
RA symptoms experienced can vary from mild to severe and include joint pain, stiffness, fatigue, bone erosion, and deformities.
6. Rheumatoid arthritis can be both a visible and invisible chronic illness.
There are a variety of experiences and hidden symptoms that may be experienced by people living with rheumatoid arthritis. Living with RA can sometimes feel like having a visible and invisible illness depending on the symptoms experienced at any given time. This has been hard to navigate and explain what I’m going through when it impacts how I am able to show up in my relationships or different roles in my life.
7. Support resources are available for people newly diagnosed with rheumatoid arthritis.
The Arthritis Foundation is potentially good support and a place to find information, tools, and resources to connect with others, education, and life after diagnosis. I found it particularly helpful as I didn’t know anyone else when I received my diagnosis and I didn’t know what kinds of questions to ask to advocate for myself or where to find resources for support and learning more about my condition.
8. The rheumatoid arthritis diagnosis and treatment journey can be different for each patient.
For me, this was and continues to be the case because the symptoms, treatment, and complications connected to RA within my body interact with my other medical conditions, creating an overlap of symptoms and contradictions that can be hard to pull apart to gain clarity. Advocating for my rheumatologist, neurologist, and primary care physicians to be in communication with each other has been helpful, especially when things get complex and confusing beyond just me.
9. The fatigue is real.
Flare-ups are real. The experience of living with rheumatoid arthritis at every point is real.
10. Shifting and adapting may be required in life with rheumatoid arthritis.
Sometimes the way I am able to engage in different areas of my life such as work and social engagements has to shift if I’m in a rheumatoid arthritis flare-up or just don’t have the energy. I remind myself that this is OK, even if it is bumping up against my internal stigmas of what I “should” and “shouldn’t” be able to do. Adaptive equipment such as my walker, keyboard, mouse, and special grips help me with doing day-to-day activities when my symptoms are high as well.
11. Support and help may be needed at different points and in different ways.
For me, this has included parenting, which has been hard. But, the support especially during my flare-ups or on my harder days helps me be there for my active 15-month-old daughter in different ways while also being able to lean on support.
12. Stress management, self-care, and other strategies can make a difference when you live with rheumatoid arthritis.
This has been true for me as stress exacerbates my symptoms and contributes to RA flare-ups. So, having my boundaries in place and my evolving self-care plan is medically necessary for all aspects of my health and life. Water aerobics, seated yoga and meditation, and adaptive sports have also helped me continue to do the things I love, manage my stress, and engage in self-care.
13. It’s OK to not feel OK.
It’s also OK to feel OK. All feelings are valid. Rheumatoid arthritis for me feels like being on two different roller coasters at once — a physical one and a mental-emotional one. You are not on this journey alone.
Getty image by wildpixel.