The Patient Side of the Opioid Discussion That Needs to Be Heard
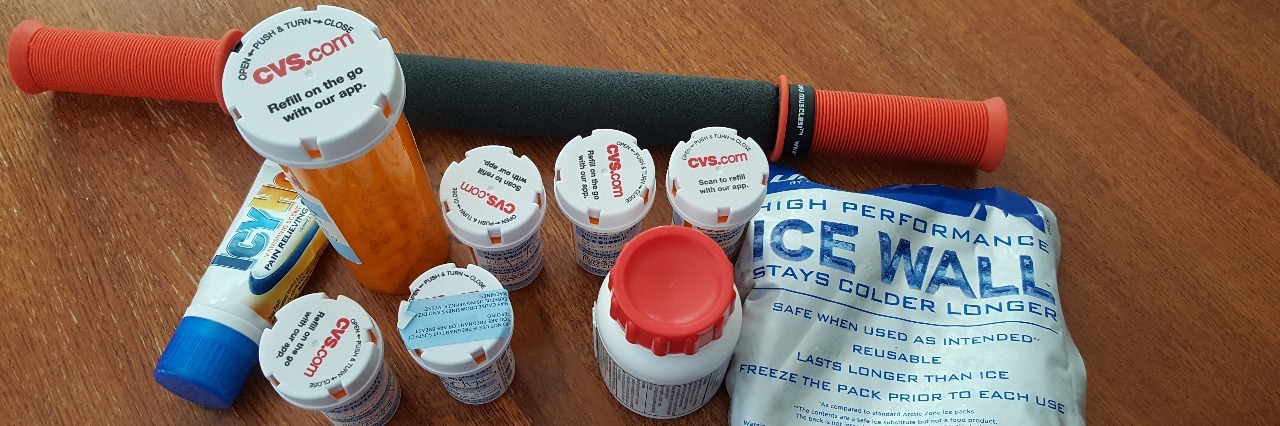
On Monday evening I took my weekly dose of methotrexate which means Tuesday sucked. I couldn’t stay home Tuesday as I usually do. I had a meeting at school and another at church. In the midst of the metho burn and the lupus/fibromyalgia medieval torture techniques, I sought out my kitchen cabinet for some relief before going to bed at 2:30 in the afternoon. Alas, the bottle of Norco was down to four lonely tablets. I stood there debating. Do I take a precious tablet or do I save it for an even rainier day? After quick yet painful deliberation, I left all four huddled together in the bottom of the bottle. I went upstairs to grin and bear it. After all, with these recent attacks on opioid use, these may be my last four. I was already hurting enough to want my legs pulled off, but I might hurt even more next week.
I got that bottle of 30 tablets almost six months ago after being drilled by my doctor about my use to make sure I am not addicted and to make sure I am responsible enough to care for myself. I felt that, as a pain patient, I was believed to be unable to use reason when it comes to my own body.
Don’t I have other options? Certainly.
1. Massage — Works wonders on me! It isn’t covered by my insurance, and at about $100 a session isn’t realistic as an ongoing treatment.
2. Physical therapy — Love it! My insurance covers some of it. But, I am being denied it for some unknown reason, and no one will return my call to explain why. My physical therapist is just as confused as I am.
3. Acupuncture — Also works. It’s also not covered by insurance. While not as expensive as massage, the cost still adds up too quickly. Yes, I understand that it might be a placebo effect. If it works, so what?
4. Other prescription pain meds — I have tried Lyrica, Cymbalta, Amitriptyline, Topomax, and Gabapentin. The Gabapentin works best for me, but makes me sound asleep. Therefore, I take it at bedtime.
5. Over the counter meds — Acetaminophen helps me with headaches and minor pains. It does nothing for the major pain. All the others thin my blood. I am already too short of platelets.
6. Medical cannabis — Been there, done that, wrote the book. It did help me. It also was too much of a burden on my family because of the stigma surrounding it, much like the opioid crisis.
7. Hot baths, stretches, meditation, etc. — Check, check, and check. I do all that and more.
8. Opioids — An option eroding away by government policies, media hype, and well-meaning public out to save me from myself.
I don’t need to be saved from myself. I need to be saved from my lupus. A cure would eradicate much of this discussion. For me, lupus is controllable to some extent. So why is society hell bent on taking away one of my necessary tools to control it? I need my opioid of choice, not to escape the world but to join it.
How can I be viewed as a drug addict when a 30-pill bottle lasts a good six months? Why am I being treated like a child just because I have a chronic disease? I have been using Norco for four years now. Might I become addicted in the future? Maybe, but I doubt it. It should have happened four years ago when I was taking multiple pills a day.
I am not alone in my ability to responsibly use painkillers to control my condition. Far from it. Of course I know people who have struggled with major addiction issues, who lost everything they had to drugs, some even their lives. Who hasn’t? But, who doesn’t know someone with major chronic pain issues? There are millions of us.
I am not going to quote statistics. I will leave that to the experts. I am also not so naive as to believe I could beat addiction should it ever grab hold of me. However, I am currently in the midst of a battle with a disease that wants to steal my very life and everything I hold dear in it. Being a part of my family, having a place in this world — these are the things that matter most to me.
What the h-e-double-hockey-sticks is going on that I and others like me are being denied our rights to pain relief?
Where are our advocates? I haven’t the stamina. When my own doctor says I should be able to double my Gabapentin dose because he can, I haven’t the words to remind him that I am not him. He is twice my size. He does not share my diseases. Has he forgotten that individuals do not all respond the same to medications? Should I change doctors? Do you know how changing doctors looks to a pharmacist or an ER physician looking to write or fill a pain prescription?
Help! Somebody get to that opioid discussion table! I’ve seen Britt Johnson out there working to get our voices heard. Still, we patients are being left in the dust. This needs to change.