Very few things I have experienced are quite as demoralizing and challenging as a migraine cycle that just won’t stop.
Currently, I live with the diagnosis of “chronic migraine,” which means that I experience head pain most days and a migraine attack on at least half of the days of every month. As you can imagine, such pervasive pain makes managing the basics of daily living intensely challenging.
But occasionally, this baseline level of head pain goes a step further, and I experience a period of weeks (or even months) where my migraine attacks are more severe and persistent than usual.
When this happens, migraine pain responds to typical medications and interventions with less and less effectiveness, and my daily focus becomes managing the pain or attempting to keep it from escalating (even more so than during my normal routine).
When this happens, the term my neurologist and I use is “migraine cycle” or “migraine flare.” Clinically, this is commonly referred to as “status migrainosus” or “intractable migraine” – defined as an especially severe and long-lasting form of migraine headache, affecting less than 1% of people and lasting longer than 72 hours.
An ideal migraine treatment would include preventative treatments that would keep a patient from ever experiencing such a flare. However, for chronic migraine patients who continue to search for an effective prevention plan, these cycles happen; and they are incredibly challenging, difficult to break, and frustrating to manage.
Part of what makes a severe migraine cycle so hard is that each one is slightly different, and traditional medications and tools often aren’t enough to cut through the pain for lasting relief. Each person who experiences status migrainosus will have an individual plan for combatting their pain. Unfortunately, no “one size fits all” approach or silver bullet currently exists. But there is hope. It is possible for these cycles to break and for the pain to lift. This is something I must constantly remind myself of when I’m experiencing a flare, because sometimes getting to that point involves an absolutely grueling stretch of time that demands buckets of perseverance and patience.
Below, I’m sharing six things that help me to break out of an intractable migraine cycle (this list has been developed over the eight years I have lived with chronic migraine). Disclaimer: this is not medical advice, it is just my experience and perhaps will give you some ideas to discuss with your own doctor.
1. Short-course steroid taper
I have tried many tapers various steroids to break migraine cycles and consider them one of my “last line” interventions for intractable migraine. My neurologist and I try to limit my use of steroids due to systemic stress on the body and the long list of disruptive side effects they come with (intense insomnia and irritability are the worst for me) However, around day 3 or 4 of a steroid taper, I consistently feel some relief (even if it is very minimal) and am able to lean less on my acute rescue medications. I have done steroid tapers lasting from 3-14 days. They aren’t a magic cure, and I have had times where they haven’t helped nearly as much as I hoped, but they are one of the most dependable tools in my arsenal for managing status migrainosus.
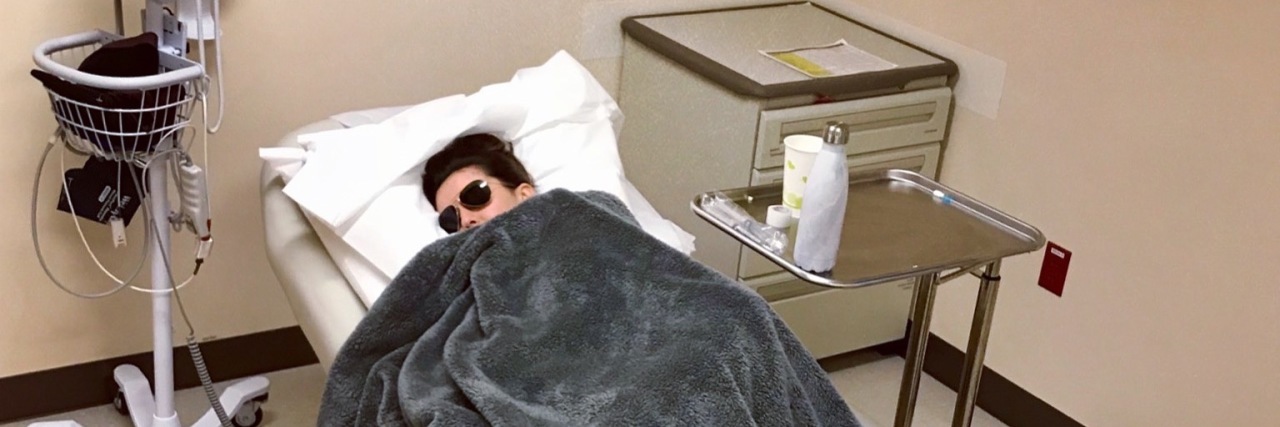
2. Outpatient infusion
I’ve done a handful of different types of outpatient infusions and found them to be very “hit and miss” in terms of their effectiveness in breaking intractable pain. However, an intense migraine cycle can land me in a pretty desperate place, and if something has helped at all in the past, I am usually willing to try repeating it. Although many infusion medications haven’t helped me, certain combinations have provided short windows of relief. There have also been times where I’ve gone in for an infusion, only to have my pain escalate back to 9/10 that same day, which is always heartbreaking. There is no right or wrong way to approach infusions when it comes to managing intractable migraine, and when I’m making decisions about what I “should” do, I try to constantly remind myself that every single person’s experience is as unique as their fingerprint, and to trust my intuition.
3. Deep sleep
This one is tricky. For me, one of the most disheartening parts about status migrainosus is that sleep will often incubate migraine pain. Sometimes I wake up literally baffled at how pain can escalate so much when I am supposedly “resting” and “restoring my body.” Going to sleep with my head hurting only to then wake up with excruciating pain is one of the most trying and heart-wrenching aspects of a bad migraine cycle. But, there is something to be said for the power and potential of deep sleep to help break a pain cycle.
During an aggressive headache cycle, I will sometimes combine my typical rescue medications with a sedating medication from my neurologist. This strategy has a pretty unreliable success rate for me; it is probably around 30%. But, because I know that sleep is important when your body is fighting so hard, I continue to experiment with and hopefully find combinations of tools that will help me to achieve the goal of resting my body. So, even though this strategy doesn’t consistently “work” to break my pain, I do think it is an important aspect of my treatment.
4. Hibernation bubble
When I’m in a bad migraine cycle, I have to be extremely intentional about my energy, activity, and interaction. This includes phone calls, text messages, outings, etc. When things are at their worst, pain-wise, I retreat to my “hibernation bubble”. I’ll put my phone on airplane mode, cancel all appointments and focus completely and solely on nurturing myself through the pain in whatever way I need in any given moment. Sometimes this means downloading a new audiobook and literally listening to it for 6 hours straight in bed with the curtains closed. Other times it means sitting on the floor of my shower for temporary pain relief. Or getting into comfortable clothes, grabbing my ice hat from the freezer, and listening to repeats of a favorite TV show for distraction. Other times it’s letting myself cry and feel the hurt and pain (even though crying escalates the pain). In my hibernation bubble, I put zero expectations on myself and make managing my pain the top priority. It’s a temporary state where I keep telling myself, “do what you need to do and nothing else”. Relying on this bubble of safety is a way to get me through when I feel like I can’t do “it” anymore.
5. Time and patience
I almost cringe writing this because I know that when you are in the middle of weeks of unrelenting pain, this feels like the most unhelpful advice in the world. However, for me, it truly is one of the bedrocks of getting through status migrainosus. I repeat mantras that remind me of the impermanent nature of everything. One of my favorites is: this can and will change. Sometimes, when I am doing everything I can to break the pain and it isn’t working, the only thing that keeps me going is the knowledge that it simply cannot last forever. I remind myself that I have experienced migraine cycles that felt never-ending before, and have I always come out of them… eventually.
6. Urgent care/emergency room
The last resort is always to visit urgent care or the emergency room. Part of what makes this such an undesirable option is you never know what you’ll get (care-wise) until you’re actually there. I have gone into the ER with written instructions from my neurologist. Some doctors follow the list exactly, and others decide that “they know best” and do something completely different. This is so hard and stressful. However, when you are truly at a breaking point with your pain, sometimes it is necessary. Many migraine patients have horror stories from the ER, but I can say with a grateful heart that, on the whole, my experiences have been more positive than negative.
If you do find yourself in the position of having to go to the ER, a few things I’ve found helpful are:
- Have a plan of what to ask for with your headache specialist
- Pack ice packs/sunglasses/headphones/hat
- Make sure to bring someone who is familiar with your migraines and can advocate for you.
It can be absolutely soul-crushing to go through the experience of getting migraine treatment in the ER and then have your migraine escalate the next morning, but there is no shame in reaching a point where you need help, even if it is temporary.
Some treatments I have tried that haven’t helped me (but have worked for others!) and might be worth talking to your doctor about:
- Nerve blocks
- SPG (spenopalatine ganglion) blocks (can be used both as acute and preventative treatment)
- Regular outpatient infusions
Lastly, some patients with intractable migraine wind up being admitted to the hospital for inpatient treatment for a few days. This is something I haven’t personally done, but I’ve gotten extremely close to needing (have even scheduled admittance dates) a handful of times. It’s a very scary place to be and can feel downright apocalyptic to have migraine pain so severe it requires hospitalization. But it is a widely used tool for out of control migraine pain, and something worth considering when the circumstances call for it.
The people who endure status migrainosus are some of the toughest people around. It’s an isolating battle fought behind closed doors and blackout curtains. But, I want you to know that if you’ve been to that dark place, fighting that agonizing unseen enemy — I see you, I understand your pain and I am in total awe of how strong you are.