At the age of 4, I was diagnosed with severe asthma and attention-deficit/hyperactivity disorder. During sophomore year of high school, I developed multiple allergies out of blue. I became allergic to corn, all tree nuts, and cats to name a few. Junior year became the ultimate battle for my health. In 2008, I could not tolerate most foods and vomited shortly after having a meal. I ate the same frozen TV dinner for two years because I could tolerate it. During this time, I became extremely ill and weighed only 95 pounds.
Most of the doctors had a hard time diagnosing my illness. Eventually, I discovered the source of my illness from a colonoscopy and endoscopy. I had an ongoing allergic reaction that wrecked havoc on my body. With patience and a specialized diet, I started to gain my weight prior to the start of my freshmen year in college for the fall 2010 semester.
My physicians recommended I relocate to Arizona since it is historically known to be therapeutic to asthmatics, so I decided to pursue a bachelor’s degree in aerospace engineering at Arizona State University. During my freshman year, my health significantly improved; however, it did not last. My body adjusted to the new environment and I had multiple relapses. I had two medical withdrawals for a series of asthmatic flares during the fall 2011 semester and 2014 semester. Throughout my undergraduate experience, I juggled a rigorous academic schedule with a medical schedule.
In my undergraduate experience, I had difficulty with a professor of one of my critical courses. Based on my program, I cannot take any future upper division engineering courses without passing this course and it is only offered in the fall semesters. During the beginning of the fall 2013 semester, I was treated for bronchitis at the hospital. I followed up with my professor regarding the current situation. I provided medical documentation and a copy of my homework assignment because I wanted to demonstrate to her good faith and my dedication to the program. I asked for a possible extension on our first homework assignment because I was very ill and did not have a chance to go over the homework during the teaching assistant’s office hours. She replied, “The graders will accept late homework, but with a penalty. You are probably best off to turn in what you have this morning.”
I decided to email the dean of the department about my concern regarding this course. I was allowed an extension; however, this action created a volatile environment. I failed the course and wanted to pursue a grade appeal. During a grade appeal, the student works with the dean designee, who served as a mediator between the professor and myself. However, I followed the dean designee’s advice to not pursue a grade appeal due to the lack of evidence.
In the fall 2014 semester, I took the course for the second time and missed two labs due to illness. Throughout the semester, I emailed my lab TA regularly to ask when it would be convenient for me to make up these labs. In short, my TA was not aware of my professor’s lab policies. As a result, I had to complete my lab reports during finals week so my professor could turn the grades in on time. Although I was given a two-day extension, my other classmates had two weeks to complete each lab report with assistance from the TAs. I did not have assistance from the TAs because they were studying for their finals. Ultimately, I failed my final exams and received a D for the course.
I decided to pursue a grade appeal again because I felt I was treated unfairly and had a better case. The grade appeal process took five months to complete. Although I won the appeal, I was exhausted and emotionally drained. As a result, I had to repeat the course for a third time.
In the fall 2015 semester, my professor decided to add a new policy to her syllabus. I believe this policy served as retaliation to my grade appeal of the lab reports in the previous semester. The policy stated, “Any student with more than one lab absence, regardless of whether the absence is excused or unexcused, will not receive a passing grade in the course.” Despite this new policy, I missed only one lab and passed the course.
It’s scary that I may not graduate due to financial aid regulations. “Satisfactory academic progress” is one criterion used for my financial aid. In order to receive financial aid, you must not exceed the maximum amount of credit hours for your program and have a pace rate above 67 percent. Currently, I am a senior and have five classes left until graduation. Unfortunately, I have exceeded the maximum amount of credit hours due to my medical withdrawals. I have to pursue a SAP appeal and explain my extenuating circumstances for prolonged graduation despite having a good pace rate of 82 percent. This is one of the problems that students with chronic illnesses may run into.
Currently, I am writing a creative non-fiction about college students living with chronic illnesses for my honors project. Throughout my undergraduate experience, there were no support groups on campus for this issue and I wanted to know if there were other students like me. I created a survey to understand public opinion, which I have received over 200 responses. Additionally, I have over 40 students to interview about their unique college experiences.
From my research, it seems most colleges have inadequate policies regarding college students living with chronic illnesses. One of the biggest challenges I found is absence policy. Many students I surveyed said their colleges and universities do not consider a medically documented illness as an excused absence. They rely on the professors to create their own policies for illnesses. On the other hand, most universes allow students to make up their assignments for religious accommodations or university sanctioned events. Unfortunately, my research showed that there are some professors who are not willing to give these students an opportunity to make up their missed assignments. As a result, the student may be forced to withdraw from the course or contact the dean and director of the department to reach a resolution.
Recently, I created a petition on change.org called “Conquer the Chronic Life: A call to action for parents and students.” The petition is designed to raise awareness and create a new bill. This bill would allow a medically documented illness as an excused absence at all colleges and universities, so the student has an opportunity to compete their program.
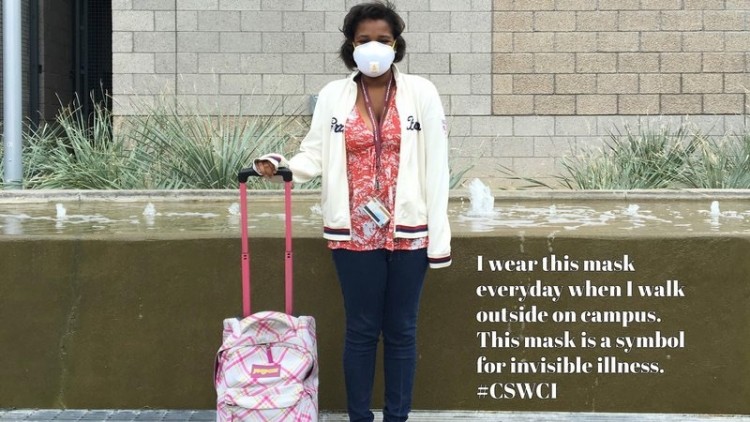
Additionally, I created the hashtag #CSWCI (college students with chronic illnesses) to create a community, which I hope will become an organization some day. I plan to release a book on May 3, 2016, which is World Asthma Day. I would like future college students to learn from my undergraduate experience.
The Mighty is asking the following: What’s the hardest thing you deal with as someone with a chronic illness, and how do you face this? What advice and words of support would you offer someone facing the same thing? If you’d like to participate, please send a blog post to community@themighty.com. Please include a photo for the piece, a photo of yourself and 1-2 sentence bio. Check out our Submit a Story page for more about our submission guidelines.
