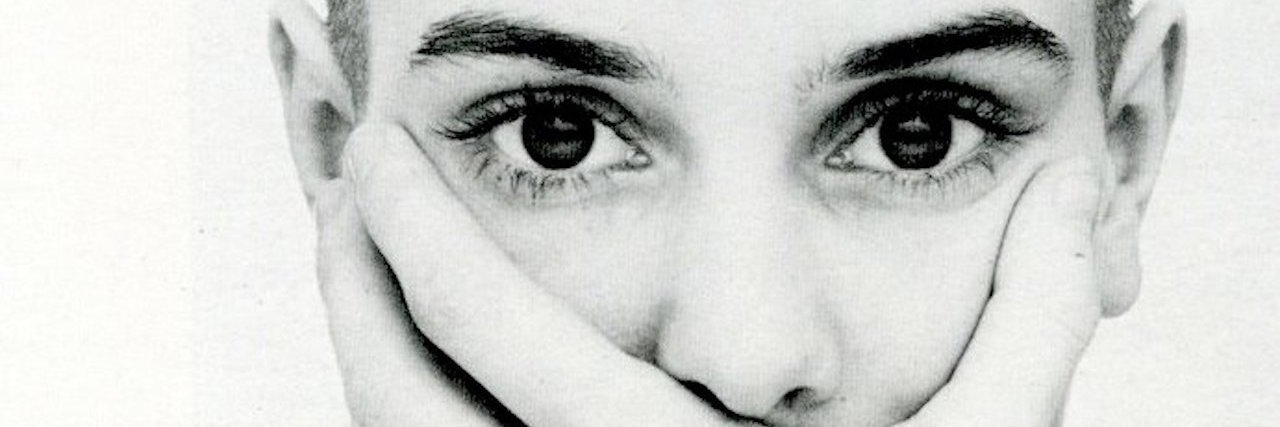
This week, Sinead O’Connor posted a video on her Facebook page. In it, she said she felt alone, abandoned and like she was only living not to die. That the “stigma doesn’t give a shit who you are.” It’s an unbelievably raw video and one that hit me hard because, like Sinead, I too have bipolar disorder. And I too have felt the isolation, loneliness and fear that comes with the illness. And the facts are this: 1 in 4 people worldwide will struggle with mental illness at some point in their lives. The WHO states that depression is the leading cause of disability world-wide.
So why do people like Sinead still struggle alone and in silence? It’s mind boggling.
1. Mental health care is not a priority for governments.
The cost of treatment for mental illness is staggeringly high and the irony is, many individuals who are struggling with illnesses such as bipolar disorder simply cannot work. Social assistance barely covers basic necessities, if that. In my experience, treatment is an out-of-pocket expense, therapy costing upwards of 200 dollars per session, and even more if someone requires multiple sessions per week. You do the math. I’ve found many individuals who need immediate care are relegated to waitlists lasting six months to one year. The only option for many is the emergency room where they end up waiting hours, only to be either discharged or held in a facility which does not promote what the individuals needs most: love, care, support, kindness. It is simply to keep them alive until they are discharged back into the world. Alone.
2. Stigma kills.
The stigma surrounding mental illness is still a major issue in many communities. Homelessness, poverty and poor nutrition is a major concern for individuals suffering and we, as a society, have a responsibility to not only refrain from judgment, but to offer compassion and understanding. We have to educate ourselves, challenge norms, question policies and call out intolerance when we see it. By doing so, we help remove the fear many people feel when struggling with mental illness. Therapy appointments should never be hidden. Bad days should never be spent alone. And emergency plans should be implemented among loved ones and friends of those struggling. Mental illness is just that — an illness. It’s just like any other illness and no one is to blame for that. So let’s not.
3. Asking for help should never be scary.
Videos like Sinead’s are not the first and I’m sure they won’t be the last. But what if there was always someone to call? What if asking for help was as simple as saying, “Can you come over? I don’t want to be alone.” We often view asking for help as a weakness or a burden. But the weakness is refusing to offer help. The weakness is looking down on individuals who find the strength to ask for help. Asking for help is a terrifying experience because when we do ask, we aren’t sure how we will feel if we are denied. What will happen if we are left alone? It may make us worse and that is not a reflection of us, it’s a reflection of how we perceive weakness. Asking for help takes courage, but so does saying “I’ll be right there.” We aren’t asking you for a miracle — simply company. Be with us. Let us cry. Hold onto us. Love us and care for us for a while, just as you would with any other sick person.
In Sinead’s words, “if you have a family member suffering from mental illness, care for them, tenderness, love. Care for them. Visit them in the hospital.”
If you or someone you know needs help, visit our suicide prevention resources page.
If you need support right now, call the National Suicide Prevention Lifeline at 1-800-273-8255, the Trevor Project at 1-866-488-7386 or text “HOME” to 741-741. Head here for a list of crisis centers around the world.
We want to hear your story. Become a Mighty contributor here.
Lead image via Sinead O’Connor Facebook