9 Things You May Not Know About Pediatric Medical Traumatic Stress
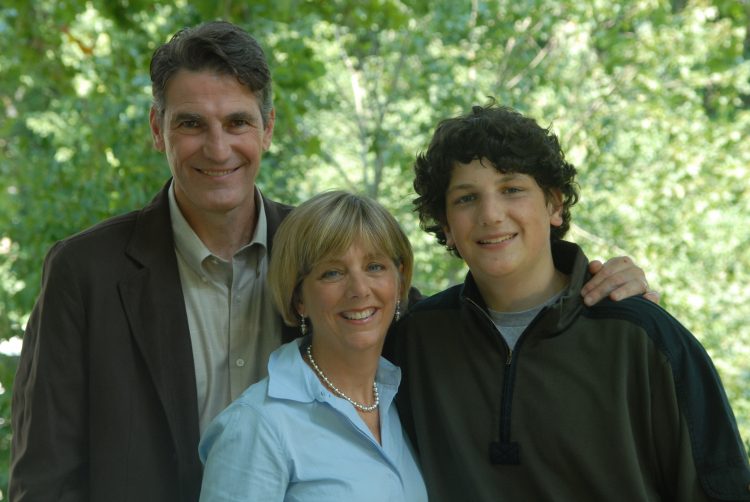
More than a decade ago, I heard a doctor say three words: “Ryan has cancer.” My son — a happy, energetic, adventurous and inspiring 12-year-old — had cancer. The word “osteosarcoma” followed. And soon we embarked on a journey that included 30 months of chemotherapy, 15 surgeries, the amputation of his right leg and over 150 days of physical therapy. The cancer came back five times. He beat it four.
Throughout his treatment, Ryan never let his illness get him down. He seemed invincible. Yet, he wasn’t. And my husband, my daughters and I weren’t either. The truth is, 30 percent of mothers whose children undergo cancer treatment suffer full symptoms of post-traumatic stress disorder (PTSD) long after the treatment is over. Children who survive their battles suffer from PTSD at a rate of 20 percent. Fathers and siblings face the same stress, pressure and anxiety. And, too often, hospitals are not adequately equipped to address it.
I know it, because I lived it. But many people are still unaware of pediatric medical traumatic stress.
Here are nine things to keep in mind if your child has just been critically injured or handed a life-changing diagnosis.
1. Childhood illness and injuries can lead to serious consequences for a child.
It’s no surprise that physical pain can traumatize a child. And the hospital is a scary place, no matter what your age is. But the effects of childhood illness or injury can be as serious and long-lasting as the effects that war has on a solider. Pediatric medical traumatic stress — all of the emotions that children experience during a serious illness, medical procedures or treatment for a life-changing diagnosis — can lead to PTSD.
On the whole, about 4 percent of children under age 18 are exposed to some form of trauma in their lifetime that leads to PTSD. That number jumps to one in six children in the aftermath of a pediatric injury.
2. The same stress affects parents, siblings and caregivers.
Believe it or not, research has shown that parents and siblings are more affected by traumatic stress than the patients themselves within the first two years of a diagnosis.
Facing a child’s life-threatening illness or injury is obviously a traumatic experience for a parent. Seeing your child in pain, feeling uncertain about the future and even navigating treatment and medical terms can cause extreme stress. While a sick or injured child — depending on age — is likely to overcome the symptoms of pediatric medical traumatic stress (PMTS), as he or she grows, parents may feel the effects for longer. In a study of children diagnosed with spina bifida, PMTS symptoms dropped in the first four years of the child’s life and pretty much went away by the time they were in school. But 30 percent of the mothers and 20percent of the fathers still suffered from PMTS.
What is not surprising, but is often overlooked, is a sibling’s reaction to the stress. Many siblings will need more time to process what the illness or injury means to them, which is different from what it means to the ill or injured child and his or her parents. Depending on their age, a child may be confused or upset by their brother or sister’s abrupt new medical needs, or resentful of the attention the sibling is receiving.
3. Pediatric traumatic stress is incredibly common.
Up to 80 percent of children and their families report experiencing traumatic stress following pediatric illness, injury, hospitalization or painful medical procedures. About a third of siblings and fathers have post-traumatic stress symptoms when a child is diagnosed with and treated for cancer, and the same is true for about half of mothers.
The effects of PTSD can — and often do — last longer than the illness and make the coping process more difficult. In up to 20 percent of childhood cancer survivors and 45 percent of their parents and siblings, symptoms persist for years after treatment has ended.
4. The emotions related to PMTS span a wide range. Experiencing one or all of these emotions is completely normal.
Lives change dramatically in the instant a child is injured or diagnosed with illness.
In the short-term following a diagnosis, a child and his or her parents will likely not feel “like themselves.” They might be easily startled or feel jumpy, often called “increased arousal” by medical professionals. Sleep may not come easily and, if it does, may be interrupted. Just as any other person experiencing PTSD, parents and children may repeatedly relive the exact moment of the injury or the doctor’s words when delivering the diagnosis.
Since PMTS and resulting PTSD stem from an immediate and long-lasting perception of life-threat, symptoms of PMTS can strike even after a child is healthy. Feeling your heart jump every time the phone rings or even recoiling at the smell of antiseptic hand wash in the years that follow is not uncommon, since the feeling that your child’s life is being threatened never truly goes away.
One of the highest-occurring long-term symptoms is avoidance, which includes trying to banish any thought of it, and staying away from people or places that serve as reminders of the treatment or injury. In some cases, this may mean going miles out of your way to avoid passing the scene of the injury or the hospital where treatment took place. On the other end of the spectrum, many experience intrusion, or reliving the medical crisis through incessant thoughts and flashbacks.
Parents in particular may find themselves worried about their whole family’s health and safety — not just the child who was sick or injured. Still, 10 years after Ryan’s death, I worry if it’s been a few days since I’ve heard from my daughters, or if my husband’s commute is taking longer than expected. Parents may also feel the fear seep into their own medical care, feeling anxious during their own doctor’s appointment, or avoiding medical tests because of “scanxiety.” The same has definitely been true for me when I was diagnosed with cancer in August, a journey that has brought me right back to the emotions of Ryan’s illness many times.
5. The rate for parents and children suffering from PTSD that stems from pediatric cancer rivals the rate for war veterans afflicted with the same disorder.
Many parents caring for an ill or injured child have a hard time believing they are experiencing PTSD symptoms. Some believe PTSD only happens to people in the military. Others may think that, because it’s their child who is sick or injured, they themselves could not be traumatized.
Nearly 40 percent of parents whose children undergo cancer treatment suffer traumatic stress symptoms. Childhood cancer survivors experience it at a rate of 20 percent. These rates are at least equal to — if not greater than — the rate experienced by U.S. war vets serving since the Vietnam War.
6. Hospitals are not always equipped to deal with pediatric medical traumatic stress.
There are a few reasons for this. For starters, helping children and their families cope with a medical crisis has not always been on the radar for hospitals. Research into pediatric medical traumatic stress is relatively new, and it’s limited. Though it’s hard to believe, the first standards for psychosocial care for children with cancer were only just published in 2016. Standards do not exist yet for any other illnesses or life-changing injuries.
As you may know, many hospitals have social workers and, if they are lucky, child life specialists to help families navigate the ins and outs of a child’s treatment. Unfortunately, extensive caseloads for social workers are often an issue, and many small community hospitals lack child life specialists, so families don’t always get the support they need.
7. PTSD can hit at any time — even years after a child’s illness or injury.
No matter where a child is in his or her treatment or recovery, PSTD symptoms can appear even years later. A child may relive the injury or the day they received the diagnosis. Parents may constantly worry about the health and safety of all of their children, not just the one who was hospitalized. Sleep may not come easy. These symptoms affect some people in the immediate aftermath of their child’s injury or illness, but for others, they may not appear until weeks, months or years later.
8. Leaving the hospital sometimes makes it worse.
It’s counterintuitive, but the day that a child is released from the hospital can trigger stress. While you may feel happy, relieved and excited to have your family all together again, don’t be surprised if you also feel scared, nervous or not ready to be without the hospital staff. It’s helpful to talk to your son or daughter’s doctor or nurse about what you can expect at home and who to call if you need help.
9. There are ways to cope.
Although PMTS is very common, you can improve your outcomes.
It seems to go against every parent’s instinct, but it is absolutely imperative to care for yourself when your child is sick or experiencing the aftermath of a life-changing injury. We talk about “putting your oxygen mask on first” and “not being able to pour from an empty cup.” These are more than just clichés. It was not always easy for me during Ryan’s treatment to take time for myself, but I can see it so clearly now: as your child’s source of strength, you must practice self-care and manage your own stress so that you can be there for your child.
It’s important to honor your emotions, but to also find healthy ways of seeking respite from them for a little while. Deep breaths go a long way in calming the body and mind. You can download an app like Headspace and practice mindfulness when you have a quiet moment. Watching your favorite movie or going for a walk can provide distraction.
People will want to help. Let them. Don’t be shy about putting together a list of needs and reaching out to friends, family and co-workers — it may feel strange to do that, but otherwise, they won’t know how to help you. This could include something as simple as sitting with your child in the hospital so that you can have a break. They could also take your other child or children on an outing, or hit the food store for you.
Depending on your child’s age, there are different ways to monitor their reactions to the stress and help them cope with it. The same goes for their siblings. You may notice regressing into old behaviors or lashing out. A well-behaved child may be getting in trouble at school. The most important thing to do is to acknowledge what is happening, and help the family navigate this time in your lives. Keep the lines of communication open between you and your family. Talk about what you’re feeling — and be prepared for the possibility that not everyone is quite ready to talk about it.
Above all, remember to treat yourself kindly. You are only human. But you are strong. And you are not alone.
Getty image by Wavebreakmedia

