A relapse is not a single event but a process. It signifies a return to substance use after a period of abstinence. Recognizing that relapse is part of a process enables you to identify early signs and take preventive measures.
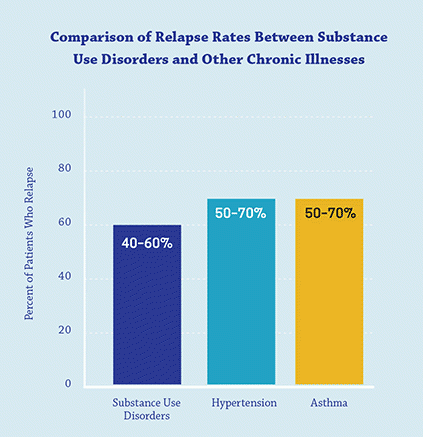
Several studies suggest that the relapse rate for substance abuse ranges from 40-60%, similar to rates for other chronic conditions like diabetes and hypertension. These stats show that relapse is often a part of the chronic nature of substance use disorder (SUD) and is not an isolated failure.
Factors Leading to Relapse
Relapse can feel like a setback that shadows your recovery journey. Why does it happen? What variables seem to conspire against us when we think we’re on a solid path? It’s not a matter of willpower alone. Relapse is often the result of various interacting factors:
- Biological Factors
- Brain chemistry: Extended substance use can alter brain chemistry, making the individual more susceptible to cravings.
- Genetics: Some genetic factors can make certain people more prone to relapse.
- Psychological Factors
- Mental health disorders: Conditions like depression, anxiety, or PTSD can make relapse more likely if not adequately managed.
- Poor coping strategies: Ineffective handling of stressful situations can push an individual toward substance use.
- Social Factors
- Peer pressure: Being around people who use can create a sense of longing and pressure to rejoin.
- Lack of support: An insufficient support system or feeling isolated can lead to relapse.
- Environmental Factors
- Availability: Easy access to substances can heighten the risk of relapse.
- Cues and reminders: Familiar sights, sounds, or smells associated with past use can stir cravings.
Common Triggers For Relapse
Understanding the common triggers often preceding a relapse is crucial to staying empowered and in control of your recovery journey. Awareness is the first line of defense. You can develop strategies to manage these triggers effectively when you recognize them. Here’s a breakdown of some of the most common triggers to watch out for:
- Stress: Personal difficulties, work pressures, and everyday annoyances can spark an intense craving for use.
- Environment: Places or settings where you used to engage in substance use can bring back compelling memories and urges.
- People: Encountering people from your past who are still using can serve as a trigger, as can conversations about substance use.
- Emotional Extremes: Both intensely negative emotions (such as sadness or anger) and extreme positive emotions (like excessive joy or excitement) can trigger relapse.
Stages of Relapse
Relapse is not a singular, isolated event. It is a gradual process that can be broken down into stages:
Emotional Relapse
This initial stage may involve feelings of anxiety, anger, or depression. Individuals might not think of using it, but their emotions set the stage.
Signs: Avoidance behaviors, poor self-care, isolation, not attending support group meetings.
Mental Relapse
The mind starts wrestling with the idea of using. It’s a tug-of-war between wanting to use and wanting to stay sober.
Signs: Reminiscing about past substance use, glamorizing one’s usage days, thinking about places and people associated with past use, and considering relapse as an option.
Physical Relapse
This stage culminates in the actual act of substance use.
Signs: Visiting places where substances are available, contacting dealers or old friends from using days.
Relapse can be an opportunity for growth and adjustment in your treatment plan rather than a point of no return. Remember, every step you take, even the backwards ones, is part of your unique path to a healthier you.
Relapse and Co-Occurring Disorders
When it comes to relapse, understanding the role of co-occurring disorders is crucial. Often referred to as dual diagnosis, this condition involves the simultaneous presence of a substance use disorder and other mental health issues such as anxiety, depression, or bipolar disorder. If you’re dealing with dual diagnosis, you’re not alone, and it’s not a reflection of weakness or lack of willpower. It’s a complex medical situation that requires specialized attention. Let’s delve into why co-occurring disorders make the journey to recovery — and relapse prevention — more complicated, yet not impossible.
The Synergistic Effect
Co-occurring disorders can have a synergistic effect where each disorder exacerbates the other. For example:
- Depression or anxiety: If you’re living with one of these conditions alongside SUD, you may use substances to self-medicate, leading to a vicious cycle of increased substance use and worsening mental symptoms.
- PTSD: Substance use can be a form of escapism from traumatic memories, but often worsens the symptoms of PTSD over time.
The Challenge in Diagnosis and Treatment
Treating one disorder without addressing the other often leads to incomplete recovery and a higher risk of relapse. One disease can often mask the symptoms of the other, making accurate diagnosis and appropriate treatment more difficult. When both conditions are not treated concurrently, the untreated condition can become a significant factor for relapse.
Importance of Integrated Treatment
The most effective approach is an integrated one that treats the SUD and the co-occurring mental health disorder. This could involve medication-assisted treatment, cognitive-behavioral therapy, and targeted treatments for the co-occurring condition.
Special Considerations in Relapse Prevention
1. Medication adherence: Skipping medications for mental health issues can destabilize your emotional well-being and increase the likelihood of using substances as a quick fix.
2. Healthy coping mechanisms: It’s essential to cultivate healthy ways to cope with stress or emotional pain if you have a dual diagnosis.
3. Regular monitoring: More frequent check-ins with health care providers can help to adjust treatment plans as needed, thereby reducing the risk of relapse.
The Role of Support
In addition to medical and therapeutic interventions, support from loved ones, community resources, and peer groups can make a significant difference.
The road to recovery feels much less lonely when you know people are rooting for you.
Ongoing Care and Management
Long-term management often involves ongoing therapy, medication, and lifestyle modifications.
Recovery isn’t a sprint. It’s a marathon with ups and downs, and ongoing care equips you for that long haul.
Understanding the relationship between SUDs and co-occurring mental health disorders is like putting together a jigsaw puzzle. Each piece provides a small part of the bigger picture. And while the journey may be challenging, it’s important to remember that understanding this complex relationship is the first step toward tailored treatment and long-term recovery. You don’t have to figure it all out on your own. With the right team and resources, you can navigate this complex terrain and come out stronger on the other side.
Steps for Preventing Relapse
Achieving sobriety is a monumental step, but maintaining it is ongoing. It’s not simply about avoiding substances but building a fulfilling, meaningful life where substances no longer have a place. That might seem daunting, but the good news is you don’t have to do it alone.
Staying Connected With Recovery Communities
- Regular meetings: Whether a 12-step program or a secular support group, consistent engagement keeps you accountable and provides emotional support.
- Online groups: Can’t attend in person? Various online forums and social media groups are designed for people in recovery.
- Mentorship: Connecting with someone who has been in recovery for a longer period can provide invaluable insights and emotional support.
Holistic Approaches to Recovery
Mindfulness and Meditation: These practices have been shown to reduce stress and increase self-awareness, key factors in preventing relapse.
Nutrition and Exercise: A healthy body can significantly impact your mental state, reducing the appeal of substances.
- Alternative therapies: Some find acupuncture, yoga, or art therapy helpful in maintaining a balanced life.
Lifestyle Changes
- Routine: A structured daily routine can reduce the emotional highs and lows that might trigger substance use.
- Occupation and purpose: Engaging in meaningful work or volunteering can provide a sense of purpose, a crucial element in sustained recovery.
- Leisure activities: Picking up new hobbies can divert your attention and offer a sense of achievement, reducing cravings.
Developing Coping Skills
- Stress management: Learn techniques like deep breathing or progressive muscle relaxation to manage stress effectively.
- Emotional regulation: Developing the skills to manage your emotional states can significantly lessen the need to rely on substances for mood alteration.
- Problem-solving skills: Instead of viewing challenges as insurmountable, acquiring problem-solving skills helps you approach them as hurdles that can be crossed.
Identifying and Managing Triggers
- Awareness: The first step in managing triggers is identifying them.
- Plan of action: Have a contingency plan for encountering a known trigger. This could be calling a friend, engaging in a physical activity, or even removing yourself from the situation.
- Ongoing assessment: Your triggers may change as you progress in your recovery. Continual self-assessment helps you adapt your coping strategies accordingly.
The recovery journey is just that — a journey, not a destination. It will have its ups and downs, but with a well-rounded approach to relapse prevention, you’re not just surviving but thriving. And remember, every step you take to fortify your life in recovery is a step away from relapse. You’ve got this!
Getty image by Cavan Images

