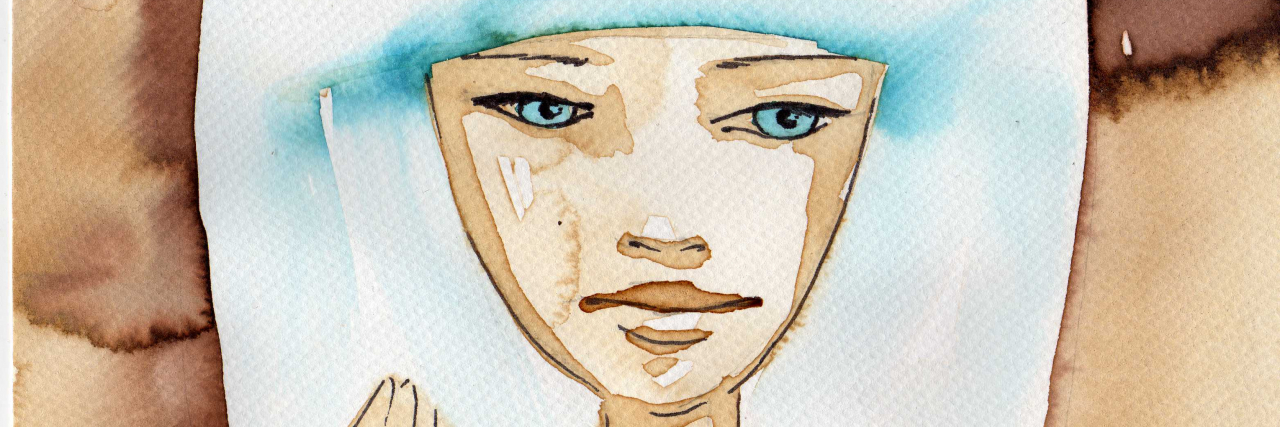
This is my fatigue.
Fatigue is a symptom of many diseases. It significantly impacts my condition, vasculitis (granulomatosis with polyangiitis/Wegener’s and chronic periaortitis). Yet when I search for a definition, it is not easy to find a clear and straightforward medical classification for fatigue. There seems to be material on fatigue within different diseases and chronic fatigue syndrome, but not really a clear definition that fits the crushing impact fatigue has on my life.
So, as I have done before, I would like to share my experience, not because I know better than others, but because I know my situation, and maybe this is repeated in the lives of others. I have found it challenging to explain my fatigue to others. Perhaps writing it down will bring me some clarity and confidence when I speak with my clinical team.
Hopefully, I can improve on my usual description of “I just don’t feel right.”
My fatigue is a mix of physical and mental symptoms. Sometimes it is not easy to split these two areas, but I will try. Often, I feel the physical is easier to describe, less subjective, and more “believable.” I don’t really understand why I think this way, I just know that I do.
My Physical Fatigue Symptoms
Physically, I feel heavy, lacking in energy, and quickly exhausted. My arms and legs feel like they have weights hanging from them. Every action seems to take double the energy it should generally take. Often, I will get cramps in my fingers and toes or restless legs.
I feel tired, but extra sleep doesn’t help me feel better. I can fall asleep watching my favorite television shows; I just do not have the energy to keep my eyes open. My head just wants to flop to the side and rest peacefully.
I feel like I have run a marathon 20 minutes after I have gotten out of bed, and I feel like I want to curl back up and go to sleep. A shower leaves me exhausted and sweating. My head feels too heavy to carry.
My Mental Fatigue Symptoms
I cry a lot; I feel hopeless and think I cannot carry on doing what I am doing. I want to give in and not keep fighting. Everything feels too much to handle; I am irritable and struggle to feel empathy for others. I don’t want to start anything, and I don’t find joy in anything that I do start. A sadness comes over me, a feeling of being useless and not wanting to carry on as I am, worrying whether I will feel like this for the rest of my life.
I cannot think logically.
I don’t learn; I don’t remember that the fatigue lifts a little and that I am coping with everything thrown at me. When the fatigue hits hard, I don’t remember that I have been here before, and I have fought back from it before. It’s like my memory is wiped after each episode. Thankfully, those around me are always there to remind me that this is all part of the illness.
How Do I Describe My Fatigue to Clinicians?
Well, I am not very good at describing it! And maybe that is why clinicians don’t take it as a severe symptom of the illness. I use words like crashed, exhausted, not quite right, and knackered. None of these really do justice to the wide range of symptoms that I experience when the fatigue hits.
Because I cannot say which physical part of me hurts, I find it hard to describe all the little things that build up to me feeling horrible. I don’t want to be a hypochondriac or dramatic. So, a long list of minor issues makes me feel like I am trying to make this into something bigger than it is. But for me, it is big; it is debilitating. It pauses my life and leaves me virtually unable to leave the house at times (except for dog walks).
What Helps Me with Fatigue?
My family helps me. They remind me that it is part of the illness and that I will return to some normality. They help me physically, and they try to give me time to rest and recover. Cuddles from my children make me realize that I must keep positive and “get my fight back” soon. My family helps me both physically and mentally to get through the fatigue. The dogs are the reason for going outside and moving, no matter how tired I am, they need to go out. Sometimes it is a slow 20-minute wander down the street, but it does help.
As predictable as it sounds, eating well helps, a nice homecooked meal does make me feel brighter, and once I eat it, I am less likely to eat the lazy stuff that is not so healthy. My husband will make a superb Sunday lunch or a summer BBQ to try and take the pressure off. He loves volunteering to do the weekend cooking, mainly with a beer in hand. Please don’t get me wrong, I am not saying food is medicine, but having a nutritious meal leaves me in a more positive mood.
Social media helps me sometimes, and sometimes it doesn’t. This seems strange to write when all we hear is that social media damages our mental health, but when you feel low and alone, somebody with the same illness on the end of your computer can make a difference. They can offer support as they understand how you feel and have been in your situation. I am very grateful to the special people I have met on social media platforms; they help me realize that I will be OK, and I hope that I help them in return.
An Unexpected Positive From Long COVID-19
I hate to write about positives and COVID-19 as it has been the cruelest impact on our world and meant we have lost some very special people. But the medical research that will focus on long COVID-19 and how the immune system works could lead to positive developments in auto-immune diseases and the treatment and management of fatigue across all disorders. I dream that the thousands of scientists examining the effects of this pandemic will lead to some tangible breakthroughs for those of us with long-term conditions that present with fatigue in similar ways to COVID-19.
This story originally appeared on Jane’s website.
Getty image by Bruniewska.