What Treatments Work for Ehlers-Danlos Syndrome?
Editor's Note
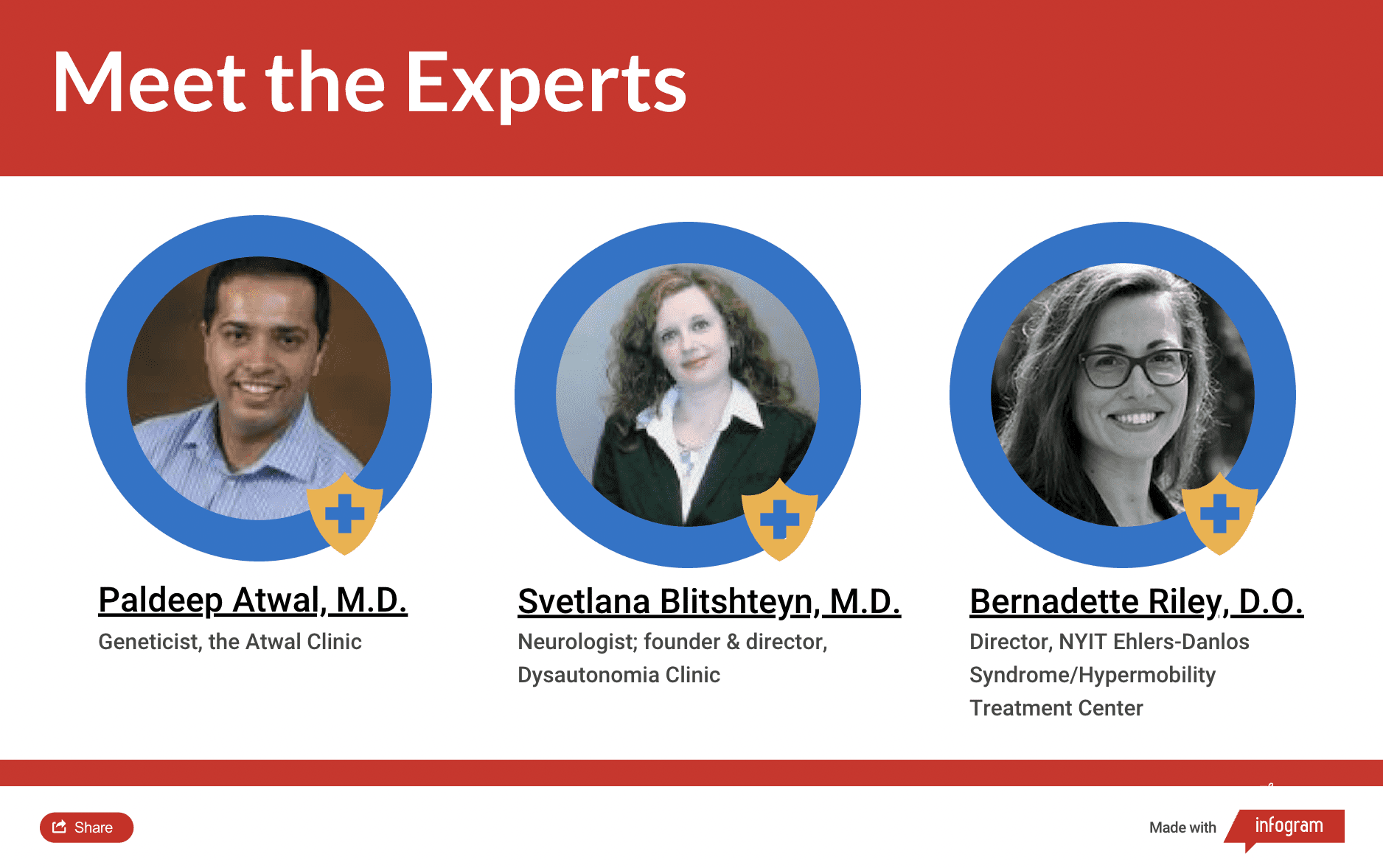
The Mighty’s Condition Guides combine the expertise of both the medical and patient community to help you and your loved ones on your health journeys. For the Ehlers-Danlos syndrome (EDS) guide, we interviewed three medical experts, read numerous studies and surveyed more than 750 people living with EDS. The guides are living documents and will be updated with new information as it becomes available.
What Treatments Work for Ehlers-Danlos Syndrome?
The best treatment for Ehlers-Danlos syndrome (EDS) will depend on your EDS subtype and your individual symptoms. While there is no cure for EDS, using a combination of therapies, medications, exercises and alternative treatment options, you can manage your symptoms. Examples of treatments that have helped others include low-impact exercise, mobility assistance devices, pain management and diet changes.
• What is Ehlers-Danlos Syndrome?
• What Are Common Ehlers-Danlos Syndrome Symptoms?
Learn More About Ehlers-Danlos Syndrome: Overview | Symptoms | Diagnosis | Resources

Medically reviewed by Catherine Karimov, MD, FACMG, FACOG
Treatment Specialists Who Can Help | Common Treatment Options | Considering Joint Surgery | Preventing Worsening Symptoms | Treating Related Conditions | Preparing for Emergencies | Pregnancy and EDS | Living With Ehlers-Danlos Syndrome
Understanding Ehlers-Danlos Syndrome: Treatment Options
Though there is no cure for Ehlers-Danlos syndrome (EDS), you can manage your symptoms through a variety of therapies, medications, exercises and alternative treatment approaches.
To cure EDS, scientists would have to alter the genes responsible for the condition. It’s unlikely there would be one cure for all 13 subtypes since different types affect different genes and work through different mechanisms. Gene editing is still an evolving technology and isn’t ready for study in EDS patients. Researchers and doctors are focusing on effective treatments for the collagen proteins in your body most impacted by EDS. They just haven’t found definitive answers yet.5
In addition to directly treating EDS symptoms, your doctor will identify and treat any co-occurring illnesses such as irritable bowel syndrome (IBS) or gastroparesis so you have the best quality of life possible. In combination with preventative measures and early interventions, it’s possible to reduce the impact EDS on your day-to-day life.

Treatment Specialists Who Can Help
EDS can impact many systems in your body, so your treatment team will likely need to be diverse. A geneticist might provide a diagnosis and suggest management strategies for your other doctors, while your pain specialist manages your chronic joint pain. A neurologist or cardiologist might be helpful if you have postural orthostatic tachycardia syndrome (POTS) along with EDS. You might be referred to specialists for a second opinion or additional testing while others, like a nutritionist who can give you advice on diets for irritable bowel syndrome (IBS) or a physical therapist to work with you on minimizing daily activities that might injure you.
When you’re searching for a doctor or a specialist, it’s helpful to ask how familiar they are with EDS. You want to see a clinician who understands the disorder and is up to date on the latest treatment options. Depending on where you live, it may be hard to find even one of these specialists. You can try connecting with other EDS patients online who live in your area to see if you can find doctors who can help.
Clinical Geneticist
A clinical geneticist specializes in illnesses inherited and passed through families, including EDS. They are equipped to determine what tests you need to find out what your genes say about the subtype of EDS you have as well as provide additional information for your family about conditions like EDS that are inherited.11 In most cases, you’ll need to see a geneticist (or your doctor will order genetic testing) to get a firm EDS diagnosis and suggested medical management based on your EDS subtype.
Neurologist
Neurologists — most commonly associated with treating brain-related conditions — specialize in your entire nervous system. They can help treat dysautonomic conditions, which occur when your autonomic nervous system doesn’t correctly regulate body functions that are controlled without you having to think about them, like breathing, your heartbeat or blood flow. This might be migraine, neuropathy or postural orthostatic tachycardia syndrome (POTS).6
Pain Management Clinics
EDS can be painful so heading to a dedicated pain management clinic might provide some relief for chronic pain. There are two kinds of pain clinics you may find helpful. Intervention-based pain clinics specialize in pain treatments like injections and nerve blocks. A rehabilitation clinic provides a one-stop-shop for pain management with everything from medication to lifestyle changes and occupational therapy.25 Many pain clinics also offer acupuncture.
Alternative or Holistic Practitioner
Alternative or holistic practitioners typically view EDS symptoms from a whole-body perspective. They use regular practices from the Western world like prescription drugs, but they also use “alternative” practices like acupuncture, mindfulness and lifestyle changes. For conditions like EDS that need a personalized treatment plan, a functional doctor may offer additional treatment choices.18
Orthopedic Doctor
Orthopedic doctors focus their practice entirely on your musculoskeletal system, including bones, muscles and joints. If you live with scoliosis, kyphoscoliosis or joint pain or dislocations, an orthopedic doctor may be able to provide in-depth treatment options to manage pain and increase mobility. They may also provide helpful suggestions to manage joint hypermobility, dislocations and pain.
Ophthalmologist
An ophthalmologist, not to be confused with an optometrist, has the highest level of medical training on conditions that affect your eyes, including care for vision issues that result from EDS.1 Whether it’s vision problems or complications in your cornea as a result of EDS, an ophthalmologist should have the required training to provide effective care.
Cardiologist
If you have cardiovascular EDS symptoms like heart problems or artery complications, a cardiologist can make sure your treatment plan takes those symptoms into account. You may need regular heart and artery monitoring to get ahead of potentially fatal issues like a ruptured artery.6 These doctors are also able to help manage postural orthostatic tachycardia syndrome (POTS).
Gastroenterologist
Gastroenterologists deal with all things gastrointestinal and digestive. Considering having EDS means you’re more likely to have a digestive tract issue, you may be referred to a gastroenterologist.6 They can help address conditions like constipation, irritable bowel syndrome (IBS) and gastroparesis as well as monitor to prevent more serious complications like a ruptured colon.
Physical Therapist
One of the best treatments for joint hypermobility is regular exercise and movement. This is where a physical therapist, a practitioner who focuses on stretching and movement exercises, might come in.14 Be sure to seek out a physical therapist who understands EDS and takes into account joint hypermobility in particular because the regular physical therapy treatments they might try can actually hurt patients with EDS.6
Hematologist
Hematologists specialize in blood and blood-related issues. Because you might bruise easily, which can be severe depending on your EDS subtype, you might be referred to a hematologist to rule out an underlying hematologic disorder.6
Rheumatologist
Rheumatologists have specialized knowledge of musculoskeletal and autoimmune diseases like rheumatoid arthritis, osteoarthritis, gout and lupus.4 If your doctor suspects you have a condition like fibromyalgia or an autoimmune disease, a rheumatologist might be helpful to make an additional diagnosis or rule out these other illnesses. They can also provide additional care if you have EDS symptoms that affect the strength of your bones.
Mental Health Professional
Like other chronic illnesses, living with EDS can take a toll on your mental health and lead to depression, anxiety and other mental illnesses.6 A psychiatrist, who will have an MD or DO license, can treat mental illness by prescribing medications. A psychologist, therapist or counselor can provide support through techniques like cognitive-behavioral therapy (CBT), talk therapy or group therapy to treat mental illness, reduce stress and teach calming techniques that can even reduce your pain levels.

Common Treatment Options
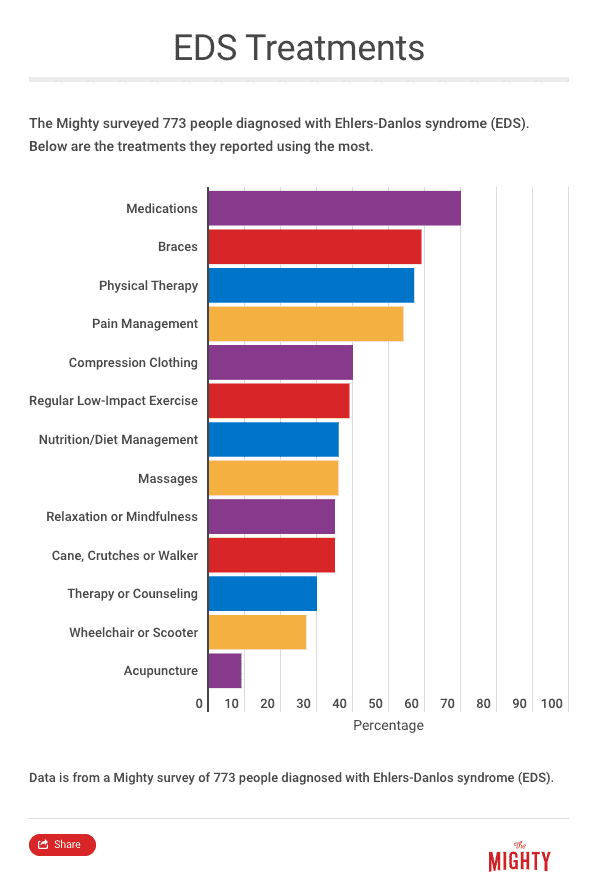
There is a lot of variation in the EDS symptoms you might have, even within just one subtype, let alone across all 13. The best way to find a comprehensive treatment plan is to work with your doctor or team of doctors. What this looks like will depend on your subtype and the severity of your symptoms. For symptoms that are common among many of the EDS subtypes, doctors might especially focus on increasing your muscle strength and healthy joint movement, reducing chronic pain and suggesting lifestyle changes to reduce the impact of your symptoms.
Exercise and Mobility
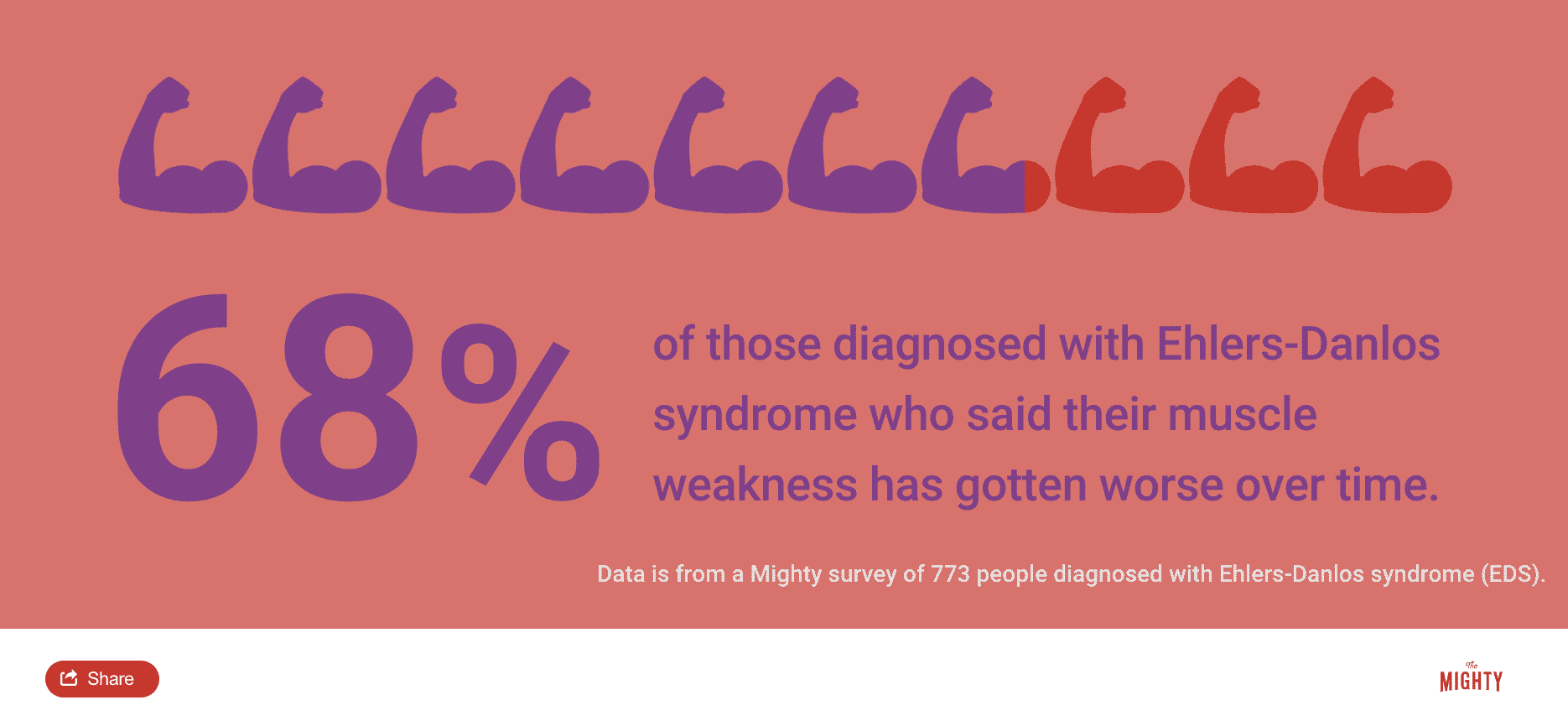
It might sound counterintuitive, but even when you have a lot of joint pain, the best thing you can do is get those joints moving. In short, staying active in some capacity conditions your muscles and makes them more resilient and stronger to support your joints.5 Staying mobile reduces pain, dislocations and even fatigue. Exercise can stop deterioration and deconditioning or a worsening of your condition and improve the overall quality of your life, even if seems too painful to start. Some doctors estimate it’s the best exercise to include in a treatment plan because it helps many aspects of your well-being, not just your joints.5
The exercise you’ll want to start with should be low-impact and gentle. Consider five minutes on the elliptical or gentle stretching every day to get your joints moving, working together and get some coordination going.5 Avoid stop-and-go or repetitive activities like running on pavement, which is hard on your joints and can cause worsening symptoms. Keep in mind it may take time until you notice an improvement. It can take months of muscle toning to reverse deterioration and maybe even longer until exercise reduces your pain levels.
Addressing Chronic Pain
EDS is more than just flexible joints — it can be very painful and debilitating. Pain could come from your joints and dislocations or even headaches, which about a third of people with EDS experience.10 Therefore, your treatment plan may need to include pain management through medication, physical-based therapies and even psychological methods like meditation or cognitive behavioral therapy. A comprehensive pain management program will tackle pain from various angles, even working to address your fatigue, which is a major factor in chronic pain.
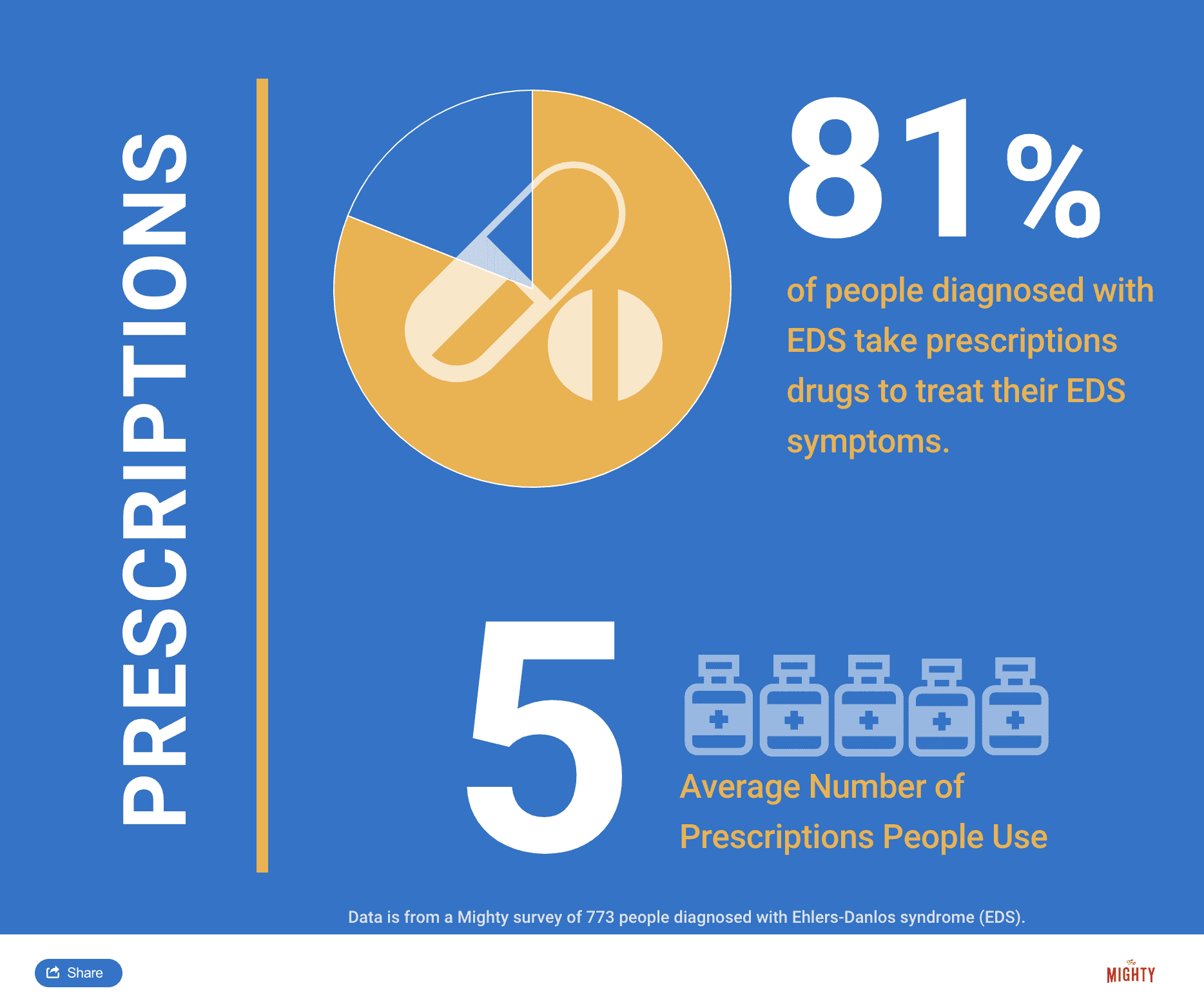
Medication is one component of chronic pain management. Your doctor may choose a number of different drugs. Some medications, like ibuprofen and opioids, may not be recommended if they cause worsening pain or dependency. The goal with pain management is to become more functional and then decrease pain medication needs with other therapies. You’ll also want to be careful with nerve pain medications because when you have hypermobile Ehlers-Danlos syndrome (hEDS), they can actually make your symptoms worse if not coupled with physical therapy and strategies to prevent further damage. Nerve pain medications are designed to blunt your pain response. Some people have found medications for muscle contractions helpful to reduce both pain and fatigue.
Osteopathic Manipulative Treatment
Practiced by doctors of osteopathic medicine (DO), osteopathic manipulative techniques are similar to what a chiropractor might do by manipulating your muscles or joints to reduce pain, but a DO has more training and is a medical doctor.3 The therapeutic treatment takes into account your whole body and may be a helpful therapy to try.23
Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) and biofeedback (a type of mind-body therapy that helps you learn how to control some of your body’s responses) address chronic pain through psychological techniques. A CBT approach helps you cope with chronic pain and reframe what it means to live with a chronic condition. It focuses on developing your strengths and reducing stress and tension, which has been shown to be a major cause in the headaches that can sometimes accompany EDS.10
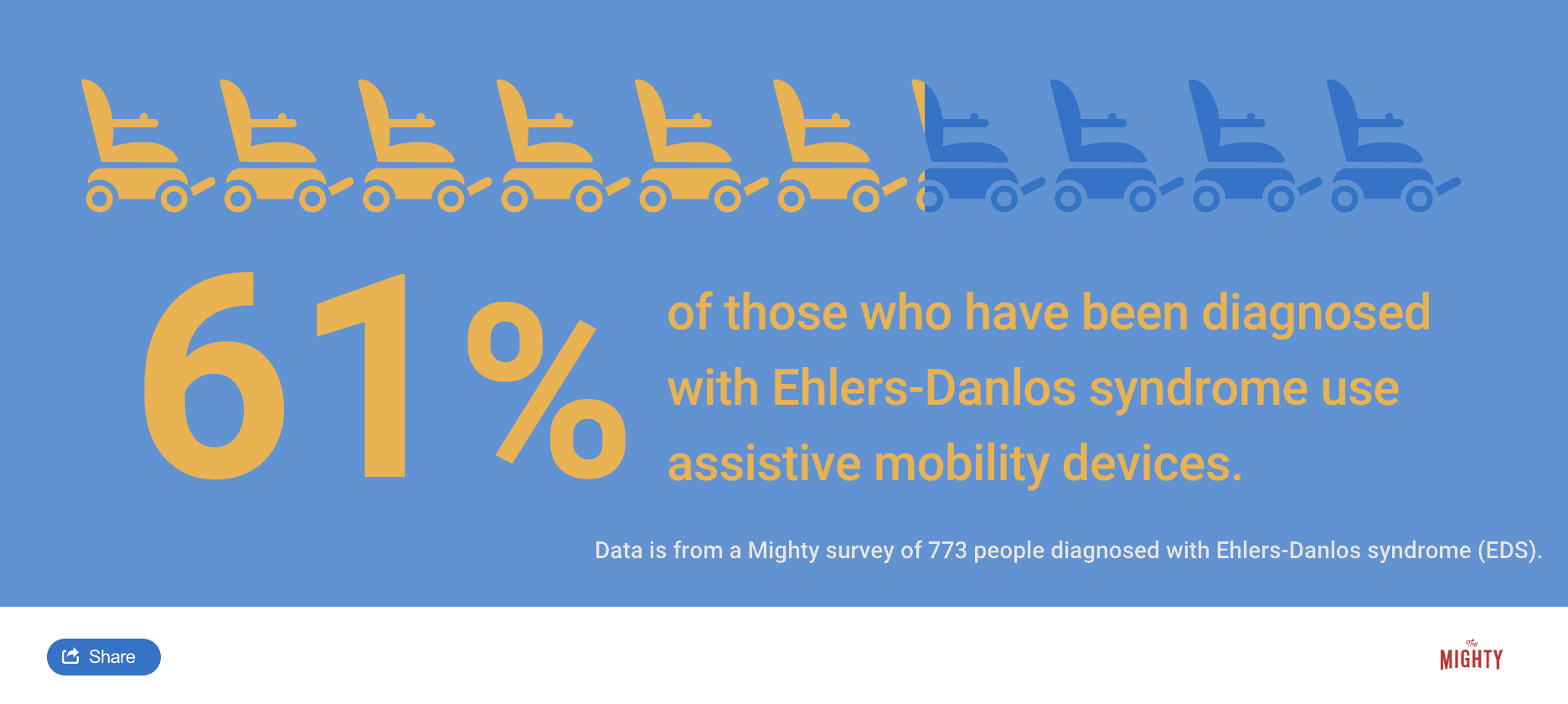
Mobility Assistance and Other Aids
To help stabilize your joints, a variety of mobility aids can make a big difference. Splints and braces might add stability to your joints so you can get on with everyday tasks.23 These can be custom designed to fit any part of your body. Wheelchairs, walkers and canes assist with mobility as needed. Compression clothing increases circulation and keeps joints in place while supportive shoe brands reduce the impact of uneven pavement and promote ankle stability.26 A variety of other aids, like pillows, athletic tape and cooling and heating products also provide a little extra comfort.
Alternative Medicine Approaches
Alternative medicine approaches to pain reduction and general wellness combine Western medical approaches and treatments still considered “alternative” that many have found beneficial with EDS. Some approaches that have helped people include:
- Apply heating or cooling pads to painful areas of your body to reduce pain
- Therapeutic massage, acupressure or acupuncture might provide relief, though check with your doctor to make sure these practices won’t have an adverse effect and find practitioners who understand EDS to prevent issues
- Practices like meditation, relaxation exercises, breathing techniques and aromatherapy may provide tension relief throughout your body
Often times natural supplements or vitamins might be recommended for your symptoms but consult with your doctor before giving them a try. When they’re combined with prescription meds, even though they’re over-the-counter supplements, they can counteract or intensify how your prescribed drugs work. Cannabidiol (CBD) — a cannabis product that will not cause a high — is an emerging alternative treatment for pain. Talk to your doctor first here too as it’s not an FDA-approved treatment for EDS. A doctor can help determine what will be right for your symptoms.
It’s worth noting that some influencers in the health space may advocate for eating or drinking collagen supplements.21 There may be a few small studies highlighting the benefits of consuming collagen in this way.22 However, the science backing this up is preliminary at best and researchers haven’t looked at the long-term risks or benefits. There’s also no regulation or oversight of the companies producing these collagen products, so it’s unlikely they will be beneficial and could even be harmful.
Diet and Nutrition
Making changes to your diet helps some people with EDS, especially for those who have food allergies or sensitivities. There isn’t one recommended diet when you have EDS, so talk to your doctor to come up with a plan that works for you.
Related:
- 32 ‘Hacks’ That Can Make Life With Ehlers-Danlos Syndrome Easier
- 20 Products People With Ehlers-Danlos Syndrome Swear By
- 23 Shoe Brands People With Ehlers-Danlos Syndrome Recommend

Considering Joint Surgery
You may need surgery for a variety of EDS symptoms like ruptured arteries or colon complications that should be considered carefully with your treatment team. However, depending on the degree of your hypermobility, dislocations or subluxations, your doctor may suggest a joint-related surgery. For example, surgeons can firm up or stabilize your joints through a process called arthrodesis by fusing together nearby joints or adding a metal structure to the area. This is a controversial practice in the EDS community, and most specialists believe it should be used only as a last resort.16
Surgery may correct some of your joint issues but inadvertently cause other problems because of the fragility of the connective tissue throughout your body. Your doctors and surgeons need to take into account your EDS at every step of the process. Though surgery may be on your joint, if you have mitral valve prolapse, sometimes called a “floppy heart valve,” surgery can increase your risk of infection in that area.
Injections into your muscles may cause extra bleeding and resulting surgical scars may heal poorly or slowly because of skin fragility. Even transferring you on the operating table can cause a problem if your surgical team doesn’t know your joints easily dislocate. In general, the risk of complications when you have EDS following surgery is higher than average, so plan carefully with your doctor before, during and after surgery if it’s the right option for you.

Preventing Worsening Symptoms
Part of living with EDS is taking precautionary measures to prevent worsening symptoms. This will be different for everyone depending on your subtype, and it’s something you’ll want to address with your doctor. One aspect might be continued monitoring based on your symptoms. If you’re at risk for cardiac or vascular complications, you may check in with your cardiologist frequently.
When your EDS symptoms include joint hypermobility and full and partial dislocations, your doctor might want you to avoid certain activities to prevent harm, such as:
- Pay closer attention to your surroundings to avoid injury by tripping over a wonky sidewalk23
- Protect loose joints with braces, splints or compression clothing where appropriate
- Avoid activity with a higher chance of joint problems like heavy lifting, intense running on hard pavement
- Get used to limiting your joint range of motion to prevent them from popping out of place5, 6

Treating Related Conditions
Many people find they have other conditions at the same time as EDS. In addition to directly addressing your EDS symptoms, it’s important to target other health concerns. This will improve the quality of your life, prevent additional complication and ensure you’re taking care of your whole body.
Digestive Problems
Experts estimate that about 75 percent of people with hypermobile Ehlers-Danlos syndrome (hEDS) experience digestive issues at some point in their lives.24 Irritable bowel syndrome, which can cause abdominal pain, constipation, diarrhea or nausea can be addressed with diet changes, regular exercise and in some cases medication.
Gastroparesis is another digestive complication common among those with EDS. It messes with the normal cycle of your digestive process, delaying digested food from leaving your stomach because of damage to your vagus nerve.2 As a result, you may experience heartburn, nausea, bloating and in extreme cases malnutrition. Gastroparesis doesn’t have a cure, but it can be managed with medications and to a lesser extent diet.
Dysautonomia
Dysautonomia is a blanket term for when your autonomic nervous system, which controls automatic bodily functions like your heart or digestive system, goes astray. You may have a more specific type of dysautonomia like postural orthostatic tachycardia syndrome (POTS), but many of the symptoms are similar.
Symptoms of dysautonomia may include6:
- Fatigue
- Dizziness
- Exercise intolerance
- Head rushes
- Racing heartbeat
Dysautonomia is treated a number of ways. You may be prescribed medications like beta blockers to reduce your heart rate, among others. Increase your water and salt intake because the extra sodium chloride boosts the amount of blood cells your body produces, which in turn increases your blood pressure. Try different positions for daily activities such as sleeping with your head slightly above the rest of the body by changing the angle of your bed to reduce symptoms.12 Compression garments like stockings or abdominal binders may also help.6
Small Fiber Neuropathy
Small fiber neuropathy is a painful condition that originates in your peripheral nervous system. It can manifest as numbness, tingling, burning, itching and decreased sensation in your hands, feet or face.6 In addition, it can cause pain “attacks” or show up as a generalized pain all over your body, making things that aren’t usually painful abnormally painful. You may experience digestive problems, heart palpitations or even, like with dysautonomia, a sudden drop in your blood pressure that leads to dizziness and fainting.23
At least 30 percent of patients with EDS also have small fiber neuropathy and it’s tricky to treat.6 Doctors often prescribe medications like antidepressants or anticonvulsants. Alternative pain relief therapies like acupuncture and massage have been recommended, but talk to your doctor to ensure that’s safe to do with your EDS symptoms. Cooling and heating treatments might be beneficial as well as comfortable clothing.17
Mast Cell Activation Syndrome
Mast cell activation syndrome may have an overlap with EDS.19, 23 Mast cells, a kind of blood cell in your body’s tissues that release immune-regulating chemicals like histamine, don’t work right when you have mast cell activation syndrome. Symptoms may include allergic-like reactions such as itching or a rash, but the condition can impact many systems in your body.
There isn’t a specific test for mast cell activation syndrome, and the symptoms can overlap some symptoms of EDS. However, there are a number of clinical symptoms and laboratory test data your doctor can use to support or rule out a mast cell activation syndrome diagnosis by looking at measures such as a validated urinary or serum marker of mast cell activation (MCA), transient increase in serum total tryptase level, an increase in other mast cell-derived mediators, such as histamine, and others.
Avoiding triggers — allergens found in food and poisonous animals like bees and some medications, sudden temperature changes or strong smells — sometimes prevents an attack. Your doctor can recommend safe drugs to take and it’s usually best to keep an epinephrine pen (Epi-Pen) on-hand if you have severe attacks.20
Mental Health
Living with EDS can impact your mental health on a variety of levels, and you have an increased risk for developing a mental illness along with EDS.8 It’s frustrating living with an often invisible illness that requires accommodations outsiders may question and this can lead to an anxiety disorder, obsessive-compulsive disorder (OCD) or depression.6, 9, 23 It’s easy to become very anxious about your present or your future when you have a chronic illness.6 For this reason, add a mental health professional to your treatment team, whether that’s a cognitive-behavioral therapist, talk therapist or even a psychiatrist if you need medication.
Other Related Conditions
EDS occurs with other chronic illnesses, and it’s important to treat as many of these as possible. Other common comorbid conditions you may have include:
- Autoimmune disorders like lupus or rheumatoid arthritis
- Fibromyalgia
- Hypermobility spectrum disorders
- Chronic fatigue syndrome
- Other sleep disorders
- Celiac disease
- Allergies
- Heavy menstrual bleeding
Preparing for Emergencies
It’s a good idea for anyone, but especially with EDS, plan for emergencies. Ensure emergency responders are aware of hypermobile joints and fragile skin and other connective tissue by keeping a wallet-sized card with you at all times. You may even consider a medical bracelet. If you have an EDS subtype that impacts your heart or vascular system, may cause a rupture in your arteries or colon or lead to a collapsed lung, it’s critical to write out an emergency plan. Get your information on file with local emergency rooms just in case, including a list of your treatment team’s contact information.7 Share all this vital information with loved ones and emergency contacts in the event you’re not able to advocate for your own needs.

Pregnancy and EDS
Just because you have EDS doesn’t mean you can’t have a successful pregnancy.13 If you’re considering getting pregnant, talk to your doctor, because women with EDS may be at higher risk for certain obstetric complications like premature labor and premature rupture of membranes.6 Sometimes your EDS symptoms may include connective tissue fragility in your uterus, cervix or vagina, and your joints may dislocate during the birthing process.
Take special precautions if you have the vascular subtype of EDS and see a maternal-fetal specialist who has managed others with your condition. Pregnancy complications like ruptured arteries have led to death in 5 percent of pregnant people with EDS. Opting to have a C-section can reduce your risk.7 You’ll want to address all of these potential complications prior to getting pregnant and keep in mind that labor and delivery can trigger new or additional symptoms.7

Living With Ehlers-Danlos Syndrome
Like the condition itself, living with EDS will vary depending on your subtype, your symptoms and the other conditions you have in addition to EDS. For most subtypes of EDS, you can expect a normal lifespan and a good prognosis.5, 6 For those with vascular Ehlers-Danlos syndrome (vEDS) it is associated with a high risk for a reduced lifespan, with the average age of death about 50 years old.7 Early death is most commonly associated with an artery tear or ruptured artery. For males under the age of 20, there’s a high risk of sudden death due to a vascular rupture caused by a sports-related injury.7
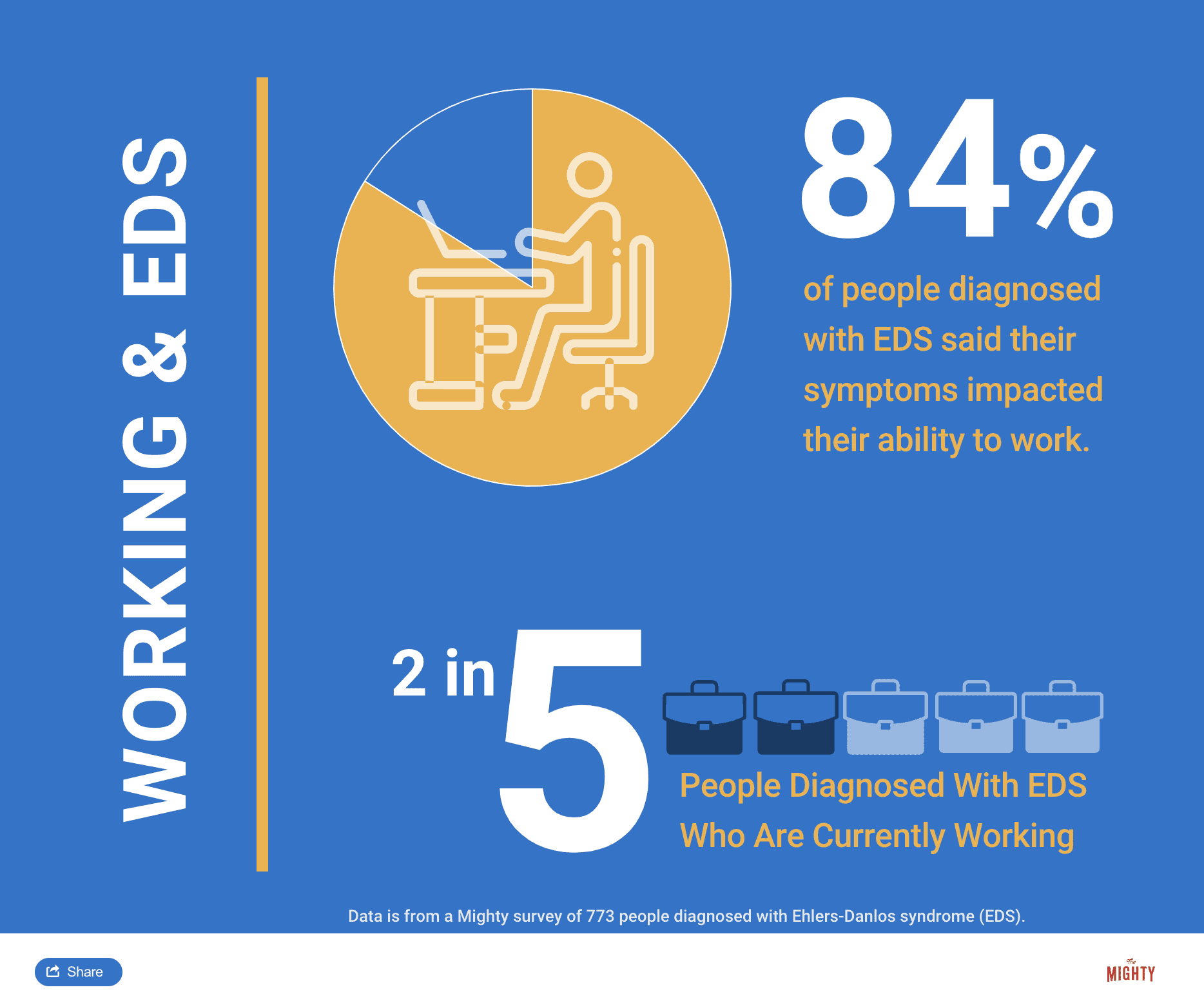
When you’re able to get a good degree of joint conditioning and treat your other symptoms with medication, therapies and lifestyle changes, you’re more likely to have a better outcome.6 However, even when you work hard on protective measures to reduce the impact of your symptoms, know that you’re not alone if EDS makes it difficult or impossible to attend school or work.6
EDS can be variable throughout your life. For example, maybe you have some pain and loose joints when you’re first diagnosed. Then in your early 20s, you might develop dizziness and fatigue and then maybe when you have children that can set off more pain and gastroparesis.6 Things can add up and you can have new symptoms or new conditions that develop alongside EDS over time. It’s a variable condition. You’ll have some good days and some bad days. Times when you’re not able to walk without assistance and others when you won’t feel many symptoms at all. The condition will be different for everyone.
Learn More About Ehlers-Danlos Syndrome: Overview | Symptoms | Diagnosis | Resources

Sources
- American Academy of Ophthalmology. (2015, August 14). What Are the Differences Between Ophthalmologists, Optometrists, and Opticians? Retrieved from http://www.djo.harvard.edu/site.php?url=/patients/pi/439
- American Diabetes Association. (2017). Gastroparesis. Retrieved from http://www.diabetes.org/living-with-diabetes/complications/gastroparesis.html
- American Osteopathic Association. (n.d.). OMT: Osteopathic Manipulative Treatment. Retrieved from https://osteopathic.org/what-is-osteopathic-medicine/osteopathic-manipulative-treatment/
- Amigues, I. (2019). Fibromyalgia. Retrieved from https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Fibromyalgia
- Atwal, P. (2018). Ehlers-Danlos Syndrome [Telephone interview].
- Blitshteyn, S. (2018). Ehlers-Danlos Syndrome [Telephone interview].
- Byers, P.H., Belmont, J., Black, J., De Backer, J., Frank, M., … Wheeldon, N. 2017. Diagnosis, natural history, and management in vascular Ehlers–Danlos syndrome. American Journal of Medical Genetics Part C (Seminars in Medical Genetics) 175C:40–47. Retrieved from: https://www.ehlers-danlos.com/pdf/2017-FINAL-AJMG-PDFs/Byers_et_al-2017-American_Journal_of_Medical_Genetics_Part_C-_Seminars_in_Medical_Genetics.pdf
- Cederlöf, M., Larsson, H., Lichtenstein, P., Almqvist, C., Serlachius, E., & Ludvigsson, J. F. (2016). Nationwide population-based cohort study of psychiatric disorders in individuals with Ehlers–Danlos syndrome or hypermobility syndrome and their siblings. BMC Psychiatry, 16(1). Retrieved from https://doi.org/10.1186/s12888-016-0922-6
- Chaplin, A. (2018). Ehlers-Danlos Syndrome [Telephone interview].
- Chopra, P., Tinkle, B., Homonet, C., Brock, I., Gompel, A., Bulbena, A., & Francomano, C. (2017). Pain Management in the Ehlers–Danlos Syndromes. American Journal of Medical Genetics Part C (Seminars in Medical Genetics), 175C, 212-219. Retrieved from https://www.ehlers-danlos.com/pdf/2017-FINAL-AJMG-PDFs/Chopra_et_al-2017-American_Journal_of_Medical_Genetics_Part_C-_Seminars_in_Medical_Genetics.pdf
- Clinical Genetics Society. (n.d.). What Is Clinical Genetics? Retrieved from http://www.clingensoc.org/what-is-clinical-genetics/
- Dysautonomia International. (2012). Lifestyle Adaptations for POTS. Retrieved from http://www.dysautonomiainternational.org/page.php?ID=44
- Fitz-Desorgher, R. (2017). Pregnancy, birth, feeding and hypermobile Ehlers-Danlos syndrome / hypermobility spectrum disorders. Retrieved from https://www.ehlers-danlos.org/information/pregnancy-birth-feeding-and-hypermobile-ehlers-danlos-syndrome-hypermobility-spectrum-disorders/
- Gardner, K. (2011). Role of a Physical Therapist. Retrieved from http://www.apta.org/PTCareers/RoleofaPT/
- Genetics Home Reference. (2012). Small fiber neuropathy. Retrieved from https://ghr.nlm.nih.gov/condition/small-fiber-neuropathy
- Hashemi-Nejad, A., & Vanhegan, I. (2016). Orthopaedic surgery in hypermobile Ehlers-Danlos syndrome and hypermobility spectrum disorders. Retrieved from https://www.ehlers-danlos.org/information/orthopaedic-surgery-in-hypermobile-ehlers-danlos-syndrome-and-hypermobility-spectrum-disorders/
- Hovaguimian, A., & Gibbons, C. H. (2011). Diagnosis and Treatment of Pain in Small Fiber Neuropathy. Current Pain and Headache Reports, 15(3), 193-200. Retrieved from https://doi.org/10.1007/s11916-011-0181-7
- Liptan, g. (2018). Fibromyalgia [Telephone interview].
- Mast Cell Action. (n.d.). About MCAS. Retrieved from https://www.mastcellaction.org/about-mcas
- Mastocytosis Society. (n.d.). Treatments for Mast Cell Diseases. Retrieved from https://tmsforacure.org/treatments-2/
- McRae, M. (2018, May 16). Eating Collagen Is Becoming a Health Fad, And We Can Only Sit Back And Sigh. Retrieved from https://www.sciencealert.com/science-behind-collagen-supplement-market-increase
- Proksch, E., Segger, D., Degwert, J., Schunck, M., Zague, V., & Oesser, S. (2014). Oral Supplementation of Specific Collagen Peptides Has Beneficial Effects on Human Skin Physiology: A Double-Blind, Placebo-Controlled Study. Skin Pharmacology and Physiology, 27(1), 47-55. doi:10.1159/000351376
- Riley, B. (2018). Ehlers-Danlos Syndrome [Telephone interview].
- Tinkle, B., Castori, M., Berglund, B., Cohen, H., Grahame, R., Kazkaz, H., & Levy, H. (2017). Hypermobile Ehlers-Danlos syndrome (a.k.a. Ehlers-Danlos syndrome Type III and Ehlers-Danlos syndrome hypermobility type): Clinical description and natural history. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 175C, 48-69. Retrieved from https://doi.org/10.1002/ajmg.c.31538
- Wait, M. (2018, July 27). Is a Pain Clinic Right for You? Retrieved from https://www.arthritis.org/living-with-arthritis/pain-management/chronic-pain/pain-clinic.php
- Wyant, P. (2017, September 13). 20 Products People With Ehlers-Danlos Syndrome Swear By. Retrieved from https://themighty.com/2017/09/ehlers-danlos-products-pain-relief/

