How to Get a Fibromyalgia Diagnosis
Editor's Note
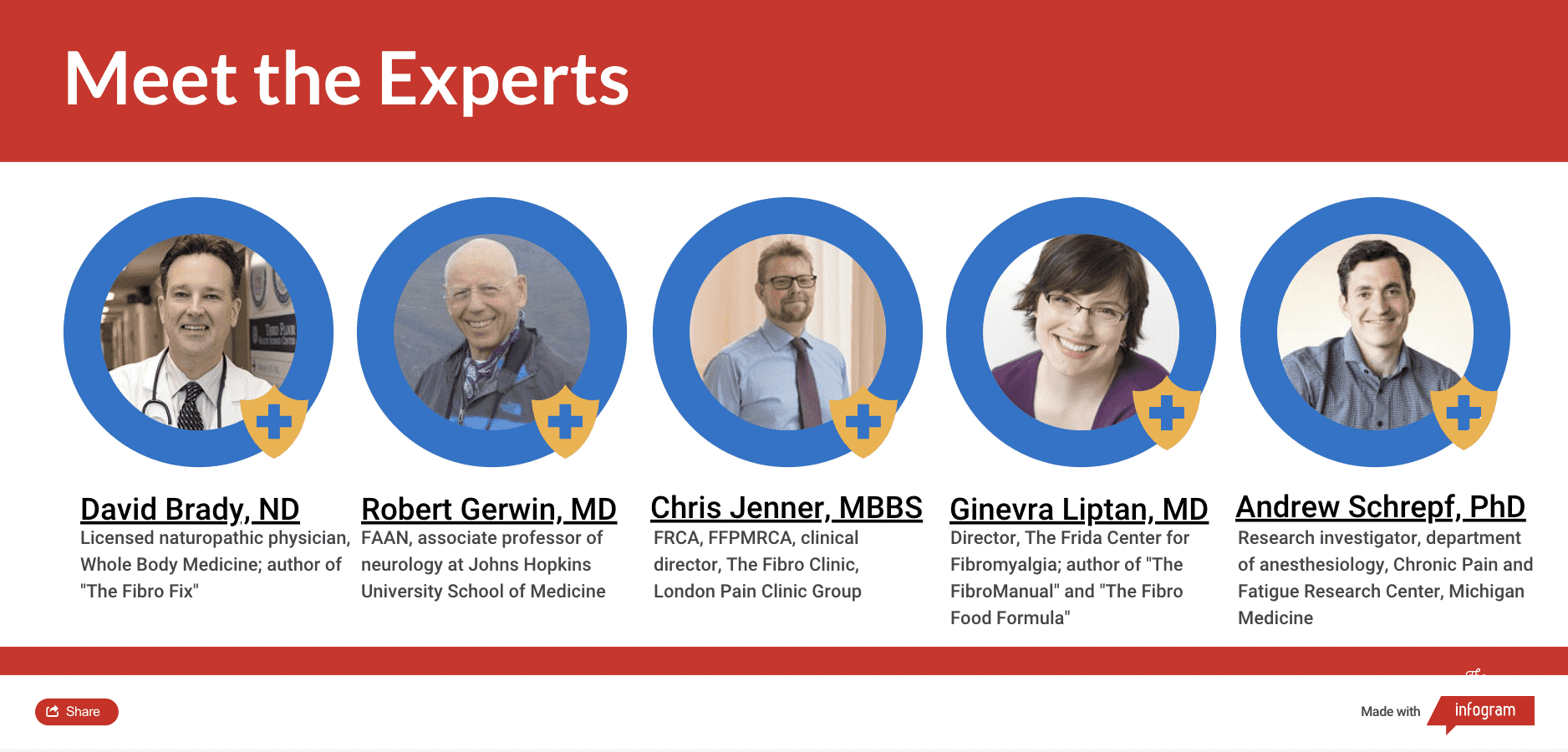
The Mighty’s Condition Guides combine the expertise of both the medical and patient community to help you and your loved ones on your health journeys. For the fibromyalgia guide, we interviewed five medical experts, read numerous studies and surveyed 13,997 people diagnosed with the condition. The guides are a living document and will be updated with new information as it becomes available.
Learn More About Fibromyalgia: Overview | Symptoms | Diagnosis | Treatment | Resources | Related Conditions

Medically reviewed by Nancy Russell, M.D.
Official Diagnostic Guidelines | Why It’s Hard to Get a Fibromyalgia Diagnosis | Conditions That May Be Mistaken For Fibromyalgia | Fibromyalgia Blood and Lab Tests
Understanding Fibromyalgia: Getting a Fibromyalgia Diagnosis
Currently, there is no definitive test to determine whether or not you have fibromyalgia. A clinical diagnosis can be made by a doctor using American College of Rheumatology (ACR) patient surveys that rate your symptoms. The 2010 ACR diagnostic criteria are most often used by doctors, with a 2016 update to the criteria.
There are three qualifications you’ll need to meet to get a fibromyalgia diagnosis:
- A significant rating on both the widespread pain index and symptom severity scale
- Generalized pain in at least four of five regions of your body
- Symptom duration of at least three months23
When making a diagnosis, your doctor will also make sure you do not have another condition that is really the cause of your fibromyalgia symptoms.

Official Diagnostic Guidelines
Set by the ACR, your doctor will want to cover the official guidelines to make your fibromyalgia diagnosis. This will include asking about your symptoms, getting a better idea of the level of pain you feel and how much your symptoms are impacting your life. Your doctor will also make sure your symptoms aren’t caused by a short illness like the flu and rule out other conditions that sometimes look similar to fibromyalgia.
Widespread Pain Index
The first measure used to diagnose fibromyalgia is the widespread pain index (WPI)23. It’s a questionnaire you answer with your doctor. In the past, physicians used a tender point examination to determine your pain level by applying pressure to various muscle areas on your body. A physical examination is no longer required to make a diagnosis of fibromyalgia, though some doctors may still use it. In part, the physical examination wasn’t helpful because everyone has a different level of pain tolerance, even when you’re in more pain than usual.20 Now a series of patient questionnaires, which starts with the WPI, are used to make a diagnosis.
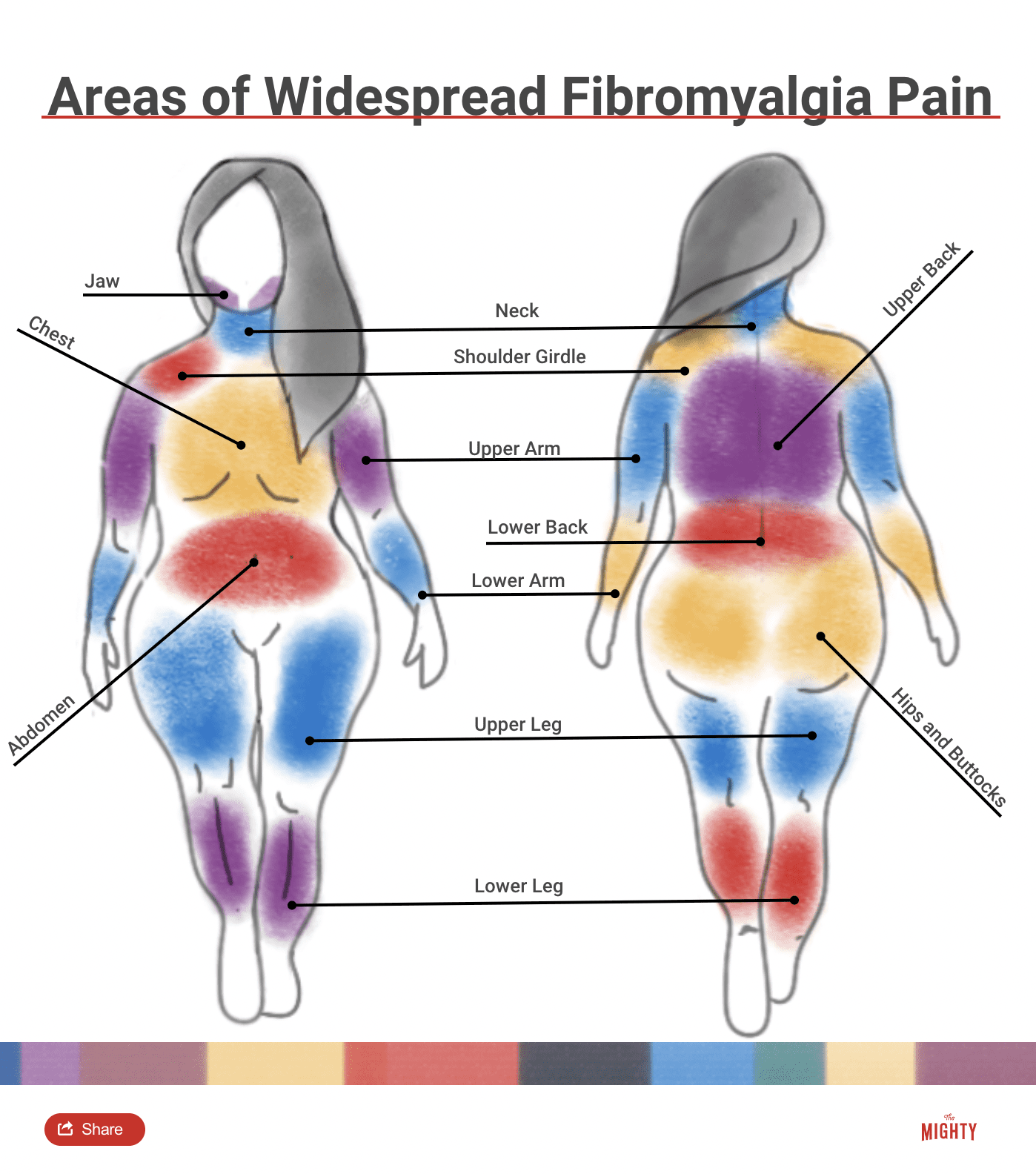
On the WPI, you’ll consider 19 areas of your body where you have experienced pain in the past week, including:
- Left and right shoulder
- Left and right upper arm
- Left and right lower arm
- Left and right hip/buttock
- Left and right upper leg
- Left and right lower leg
- Left and right jaw
- Chest
- Abdomen
- Neck
- Upper and lower back
Symptom Severity Score
A fibromyalgia diagnosis is also based on your symptom severity score (SSS)23. There are two parts to the SSS. During the first part, you’ll rate the severity of your pain, fatigue and cognitive difficulties on a scale of 0 to 3 for each symptom. A zero rating means it’s not a problem at all. Level one represents mild or intermittent problems while level two is moderate trouble that disrupts your life and occurs often. Rating a symptom three means it’s severe, constant and greatly affecting your life. After rating each symptom, you’ll add the points together for a score between 0 and 9.
Part two of the SSS records the other symptoms you’ve had in the past week, ranging from constipation or diarrhea to nervousness, dizziness, hives, swelling, dry eyes and hair loss. For each symptom you’ve experienced, check off a box. Once you’re done, count up the total number of boxes you marked. If you didn’t check anything, give yourself a score of 0. If you checked off 1 to 10 checkboxes, you score a 1; 11 to 24 boxes is a score of 2; and more than 25 boxes is a score of 3.
Now add your score from the first part of the SSS (your 0 to 9 score of the severity of pain, fatigue and cognitive trouble) to the score of 0 to 3 from the second part of the SSS on additional symptoms. Your total score, which should be between 0 and 12, is your final SSS score.1
Scoring
Your doctor will look at your WPI and SSS scores side by side. According to the 2016 ACR diagnostic criteria, which are slightly different than the 2010 criteria, you need to meet one of two score combinations to be diagnosed with fibromyalgia. The first is a WPI score of greater than or equal to 7 in combination with an SSS score greater than or equal to 5. You can also be diagnosed with fibromyalgia if you have a WPI score between 4 and 6 and an SSS score greater than or equal to 9.1
Generalized Pain
There are two additional requirements before your doctor can confirm a fibromyalgia diagnosis. First, you must report generalized pain in at least four of five regions in your body. The regions include pain on both sides of your body, both above and below the waist or pain in your neck, spine or back. Jaw, chest and abdominal pain are not considered when evaluating generalized pain.1 This is to assess for widespread pain, which is the defining feature of fibromyalgia. You’ll talk this through with your doctor. It is not based on a physical examination.
Symptom Duration
The final criterion for fibromyalgia is the length of time you’ve had symptoms. Because the feeling of fibro pain can be similar to the aches and pains of the flu or other viruses, you must experience symptoms consistently for at least three months before a diagnosis can be made. This helps your doctor rule out other temporary conditions with similar symptoms.12
Why It’s Hard to Get a Fibromyalgia Diagnosis
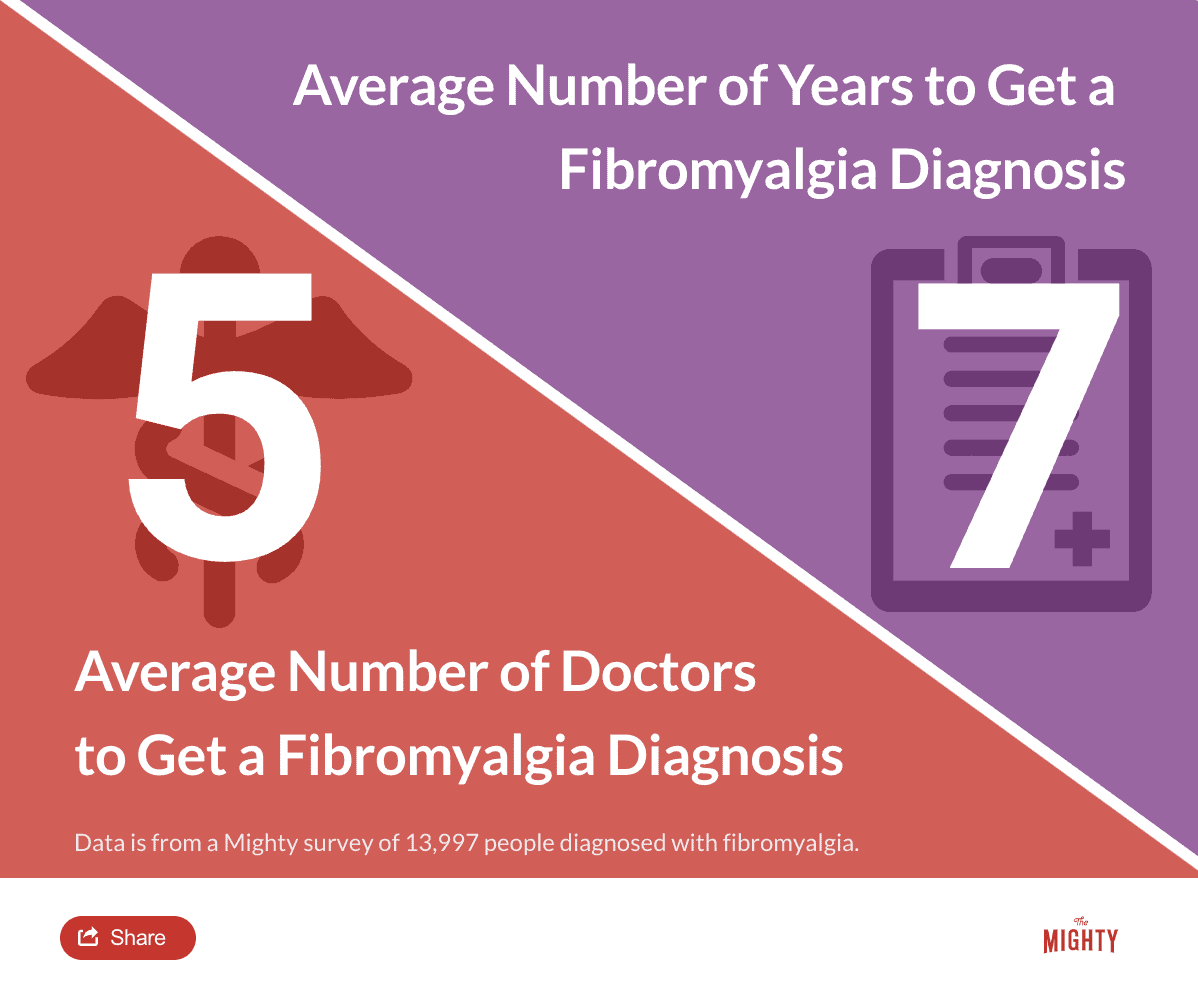
Fibromyalgia is a complicated disorder, and because it’s still not well understood, it can be hard to get a diagnosis. Over the years, fibromyalgia has caused controversy, with many doctors debating whether it was a “real” illness or not. Because fibromyalgia affects more females than males and the majority of the medical and research community identify as men, part of the stigma is due to gender bias.6 It’s also at times been considered a “wastebasket” diagnosis for chronic complaints doctors couldn’t understand. Research has lagged behind other illnesses because of the controversy, which makes diagnosis tricky even in recent years.16
While attitudes are changing, there are still doctors who do not consider the diagnosis valid or who have not caught up with the latest research. It’s estimated that it takes at least five years for someone with fibromyalgia to get the correct diagnosis, sometimes much longer.19 Other studies have shown that doctors often misdiagnose fibromyalgia, sometimes over-diagnosing.13 One study found that doctors got it wrong 66 percent of the time.10
Conditions That May Be Mistaken For Fibromyalgia
It’s challenging to diagnose fibromyalgia because its symptoms overlap with conditions that need to be either diagnosed or ruled out. In the past, a fibro diagnosis was often made by ruling out other conditions before deciding on fibromyalgia once the doctor ran out of other options.6 It’s important to correctly diagnose both fibromyalgia and other conditions that look like fibro to make sure your treatment plan will be helpful.
Below are some conditions your doctor may rule out when making a diagnosis.
Chronic Fatigue Syndrome
Chronic fatigue syndrome (CFS) causes fatigue that reduces your ability to participate in everyday activities, sleep trouble, cognitive difficulties like trouble thinking or memory problems and pain. CFS has the same symptoms of fibromyalgia, except fatigue is usually the primary symptom and symptoms must last at least six months. CFS can’t be diagnosed by a definitive test, so doctors must make a judgment call based on your symptoms. You can have both fibro and CFS.8
Hypothyroidism
Your doctor may check you for hypothyroidism, which has many symptoms in common with fibro. Hypothyroidism, which happens when your thyroid gland isn’t producing enough hormones, slows your body down.15 You may feel tired, forgetful, depressed or have digestive issues like constipation. You might experience other symptoms, some of which also mimic fibromyalgia. A doctor can order a series of blood tests to rule out hypothyroidism, which would likely include the tests TSH, T-4, T-3 and a thyroid antibodies test.
Autoimmune Diseases
Autoimmune disease, including rheumatoid arthritis and lupus, have an overlap in symptoms with fibromyalgia. Autoimmune diseases cause your immune system to attack healthy cells in your body, which leads to chronic pain and other symptoms. The pain you feel with an autoimmune disorder is in your joints, not your muscle tissue like fibromyalgia. An autoimmune diagnosis can typically be determined using blood tests.16 An estimated 10 to 20 percent of people with rheumatic disease have also been diagnosed with fibromyalgia.
Lyme disease
Lyme disease (Borrelia burgdorferi) is a bacterial disease that’s passed to humans through tick bites. Lyme disease symptoms can include: pain in the body’s tissues and joints, dizziness, nerve pain, short-term memory problems and inflammation in the brain or spinal cord.18 You can be tested for Lyme disease, but the first basic test used — enzyme-linked immunosorbent assay (ELISA) — is inaccurate nearly 50 percent of the time. A second test, the Western blot, is a common follow-up, and your doctor may recommend trying more sensitive testing from private labs such as iGenex to definitely rule out Lyme disease.17 It is common for those with Lyme disease to have fibromyalgia as a secondary diagnosis.
Anemia
Anemia is a blood disorder that occurs when your body doesn’t make enough healthy red blood cells, called hemoglobin. As a result, your body lacks oxygen. Though there are several types of anemia like sickle cell anemia, hemolytic anemia and aplastic anemia, most cases are caused by an iron deficiency. If you have an autoimmune disease, thyroid condition or inflammatory bowel disease (IBD) — Crohn’s disease or ulcerative colitis — you’re more likely to also have anemia. Symptoms include weakness, shortness of breath and headaches, among others. Anemia is diagnosed by a blood test.4
Mitochondrial Disease
Mitochondrial disease is a genetic chronic illness that affects the part of cells that produce energy — small organelles called mitochondria. Mitochondrial disease symptoms may include muscle pain and weakness, cognitive difficulties, gastrointestinal problems and seizures. The disease is progressive and has no cure or reliable test, though some specialists sometimes use blood DNA testing or muscle biopsies.2
Other Conditions to Consider
Other conditions your doctor may want to check when you have fibromyalgia symptoms can often be ruled out or diagnosed via blood or other lab tests. Your doctor might investigate migraine, endometriosis and other chronic pain conditions that are associated with a central nervous system pain processing disorder.12 Depending on your symptoms, your doctor may want to screen for cancer. It’s possible to have more than one diagnosis, fibromyalgia included.
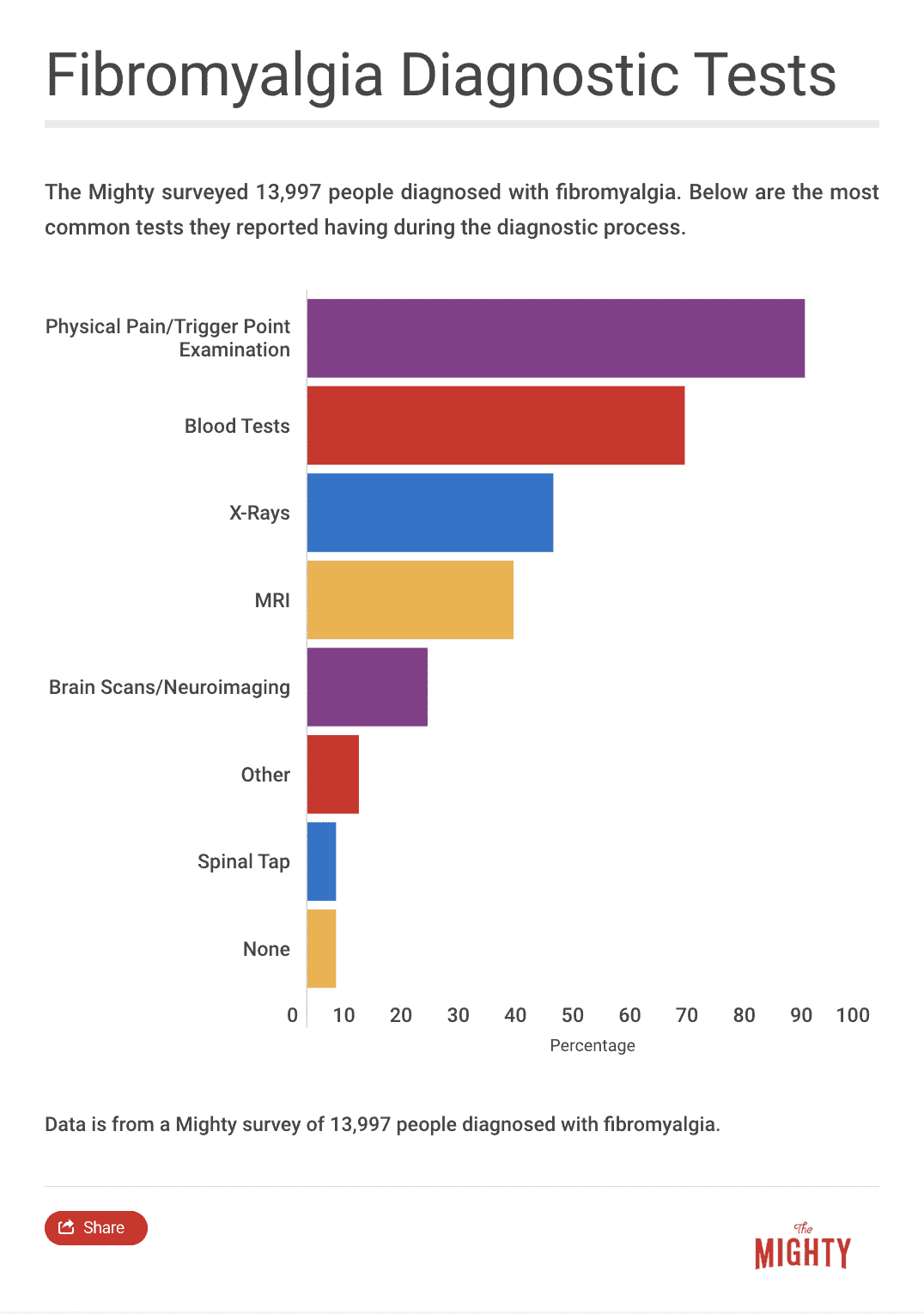

Fibromyalgia Blood and Lab Tests
There isn’t a way to definitively diagnose fibromyalgia yet, but experts estimate in the next five to 10 years, doctors will have a yes-or-no test to diagnose fibromyalgia.16 Several blood and lab tests are currently under review that show promise for the future.
FM/a Blood Test
Developed by biomedical company EpicGenetics in 2012, the FM/a blood test may confirm a fibromyalgia diagnosis.21, 5 It’s a regular blood test scored on a scale of 0 to 100. If you score 50 or higher, the company says it confirms your diagnosis with 99-percent accuracy. Your doctor must fill out an authorization form if you want to take the test.11
Testing is available in the U.S. and several international countries. Most insurance companies will cover the test, including Medicare. While the test is promising, its accuracy hasn’t been verified by independent research outside of EpicGenetics. Many fibromyalgia specialists don’t use it.
IsolateFibromyalgia Blood Test
The IsolateFibromyalgia test is another blood test that may be able to diagnose fibromyalgia.22, 7 By submitting blood from a regular test to IQuity Labs, the maker of IsolateFibromyalgia, you can get a yes or no diagnosis in less than a week. The company claims a more than 90-percent accuracy rate.
Your doctor must request the test directly from IQuity Labs. It’s only been on the market since 2018, so it’s likely not covered by your insurance nor is it available in New York.3 IQuity Labs won’t completely reveal the research they say proves the IsolateFibromyalgia tests work, so there is no verification from independent researchers.
Ohio State University Blood Test (In Development)
Another blood test is under development by researchers at Ohio State University.14 In a preliminary test, researchers were able to determine who had fibromyalgia compared to lupus, rheumatoid arthritis and osteoarthritis. While the researchers are optimistic they will be able to develop a blood test for fibromyalgia within five years, they first want to replicate the results of their initial work by doing studies with more participants and zeroing in on exactly what’s different about patterns in the blood of people with fibromyalgia.14
Spinal Tap
You may have had a spinal tap to rule out other conditions, but in the future it could confirm a fibromyalgia diagnosis. If you have fibromyalgia, doctors tend to see low levels of the neurotransmitter serotonin, which is a chemical that makes you feel better. They also found high levels of the neuropeptide substance P, which contributes to how much pain you feel in your spinal fluid.6 Using a spinal tap to diagnose fibromyalgia has only been looked at in studies and not tested for clinical practice. Researchers would need to determine if they can tell the difference between serotonin and substance P levels in fibromyalgia versus migraine and other conditions first. A spinal tap is a possible diagnostic tool, but it needs more research first.16
Learn More About Fibromyalgia: Overview | Symptoms | Diagnosis | Treatment | Resources | Related Conditions

Sources
- 2016 Revisions to the 2010/2011 Fibromyalgia Diagnostic Criteria. (2016). Retrieved from https://acrabstracts.org/abstract/2016-revisions-to-the-20102011-fibromyalgia-diagnostic-criteria/
- About Mitochondrial Disease – Mito FAQ. (n.d.). Retrieved from http://www.mitoaction.org/mito-faq
- Accurately Identify Fibromyalgia Early. (n.d.). Retrieved from https://www.iquitylabs.com/providers/fibromyalgia/
- American Society of Hematology. (2018, January 08). Retrieved from http://www.hematology.org/Patients/Anemia/
- Behm, F. G., Gavin, I. M., Karpenko, O., Lindgren, V., Gaitonde, S., Gashkoff, P. A., & Gillis, B. S. (2012). Unique immunologic patterns in fibromyalgia. BMC Clinical Pathology,12(1). doi:10.1186/1472-6890-12-25
- Brady, D. (2018). Fibromyalgia [Telephone interview].
- Cerdá-Olmedo, G., Mena-Durán, A. V., Monsalve, V., & Oltra, E. (2015). Identification of a MicroRNA Signature for the Diagnosis of Fibromyalgia. Plos One,10(3). doi:10.1371/journal.pone.0121903
- Diagnosis of ME/CFS | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) | CDC. (2018). Retrieved from https://www.cdc.gov/me-cfs/symptoms-diagnosis/diagnosis.html
- N/A
- Fitzcharles, M., & Boulos, P. (2003). Inaccuracy in the diagnosis of fibromyalgia syndrome: Analysis of referrals. Rheumatology,42(2), 263-267. doi:10.1093/rheumatology/keg075
- FM/a. (n.d.). Retrieved from http://fmtest.com/
- Gerwin, R. D. (2018). Fibromyalgia [Telephone interview].
- Gittins, R., Howard, M., Ghodke, A., Ives, T. J., & Chelminski, P. (2017). The Accuracy of a Fibromyalgia Diagnosis in General Practice. Pain Medicine,19(3), 491-498. doi:10.1093/pm/pnx155
- Hackshaw, K. V., Aykas, D. P., Sigurdson, G. T., Plans, M., Madiai, F., Yu, L., . . . Rodriguez-Saona, L. (2018). Metabolic fingerprinting for diagnosis of fibromyalgia and other rheumatologic disorders. Journal of Biological Chemistry, 294(7), 2555-2568. doi:10.1074/jbc.ra118.005816
- Hypothyroidism. (n.d.). Retrieved from https://www.thyroid.org/hypothyroidism/
- Liptan, G. (2018). Fibromyalgia [Telephone interview].
- Lyme Disease Tests – learn about the lyme tests available. (n.d.). Retrieved from https://www.lymedisease.org/lyme-disease-test/
- Lyme Disease | Lyme Disease | CDC. (2018). Retrieved from https://www.cdc.gov/lyme/index.html
- National Fibromyalgia & Chronic Pain Association (NFMCPA). (n.d.). Retrieved from https://www.fmcpaware.org/
- Schrepf, A. (2018). Fibromyalgia [Telephone interview].
- Wallace, D. J., Gavin, I. M., Karpenko, O., Barkhordar, F., & Gillis, B. S. (2014). Cytokine and chemokine profiles in fibromyalgia, rheumatoid arthritis and systemic lupus erythematosus: A potentially useful tool in differential diagnosis. Rheumatology International,35(6), 991-996. doi:10.1007/s00296-014-3172-2
- What is RNA? (n.d.). Retrieved from https://www.rnasociety.org/about/what-is-rna/
- Wolfe, F., Clauw, D. J., Fitzcharles, M., Goldenberg, D. L., Katz, R. S., Mease, P., . . . Yunus, M. B. (2010). The American College of Rheumatology Preliminary Diagnostic Criteria for Fibromyalgia and Measurement of Symptom Severity. Arthritis Care & Research,62(5), 600-610. doi:10.1002/acr.20140