What Treatments Work for Fibromyalgia?
Editor's Note
The Mighty’s Condition Guides combine the expertise of both the medical and patient community to help you and your loved ones on your health journeys. For the fibromyalgia guide, we interviewed five medical experts, read numerous studies and surveyed 13,997 people diagnosed with the condition. The guides are living documents and will be updated with new information as it becomes available.
Learn More About Fibromyalgia: Overview | Symptoms | Diagnosis | Treatment | Resources | Related Conditions

Medically reviewed by Emma Guymer, MBBS, FRACP
Specialists Who May Be Able to Help | Medication Treatments | Less Effective Treatments | Standard Treatment Options | Functional Medicine Approaches | Treating Other Fibromyalgia Complications
Understanding Fibromyalgia: Treatment Options
Fibromyalgia is a chronic illness that causes chronic pain you might feel all over your body; fatigue; and trouble with cognitive functions like thinking clearly and long-term memory. It’s believed to be caused when your nervous system gets stuck in “alarm” mode.
Because there’s no cure, treating fibromyalgia is better envisioned as a journey instead of a one-size-fits-all treatment plan. You can try many therapies, including medications, graded exercise, cognitive-behavioral therapy (CBT) and functional medicine approaches.
There isn’t one single treatment that helps the majority of all people with fibro — treatment will be individualized to what works for you.12 Keep in mind while there are a lot of treatment options available, they might not work for you. In addition, sometimes treatment won’t completely stop your symptoms, but could help you feel at least a little better.
Finding the right treatment approach might be a long journey while you and your doctors find a plan that reduces your symptoms and addresses comorbid conditions.13

Specialists Who May Be Able to Help
Many doctors, including your primary care physician, may be equipped to find a fibromyalgia treatment plan that works. Sometimes, you might want to call a specialist. Specialist fibro doctors are more familiar with the full range of treatment options and resources for fibromyalgia. Depending on where you live, it may be difficult to find even one of these specialists.
Rheumatologists
Fibromyalgia is officially classified under the rheumatology banner. The American College of Rheumatology (ACR) writes the official criteria used to diagnose fibromyalgia, for example. Rheumatologists also have specialized training in musculoskeletal and autoimmune diseases like rheumatoid arthritis, osteoarthritis, gout and lupus.2
Pain Management Clinics
Not a particular type of doctor per se, but pain management clinics specialize in the challenges of living with a chronic pain condition. There are two types of pain clinics. The first offers comprehensive services that cover everything from medications to physical and occupational therapy, nutrition and psychological strategies to manage your pain. Other pain clinics offer treatments designed to shrink your pain level using injections and nerve blocks.23
Integrative/Functional Medicine Doctors
Integrative or functional medicine doctors often take a whole-body perspective to health. Overseen by the Institute for Functional Medicine, functional medicine doctors combine traditional treatments from the Western world, like medication, with research-backed alternative practices like acupuncture or myofascial release therapy and lifestyle changes.14
Other Health Care Professionals Who Can Help
Other medical professionals could offer additional treatment perspectives. Physical therapists can develop an appropriate graded exercise program to keep your muscles moving but reduce the pain of exercise.

Medication Treatments
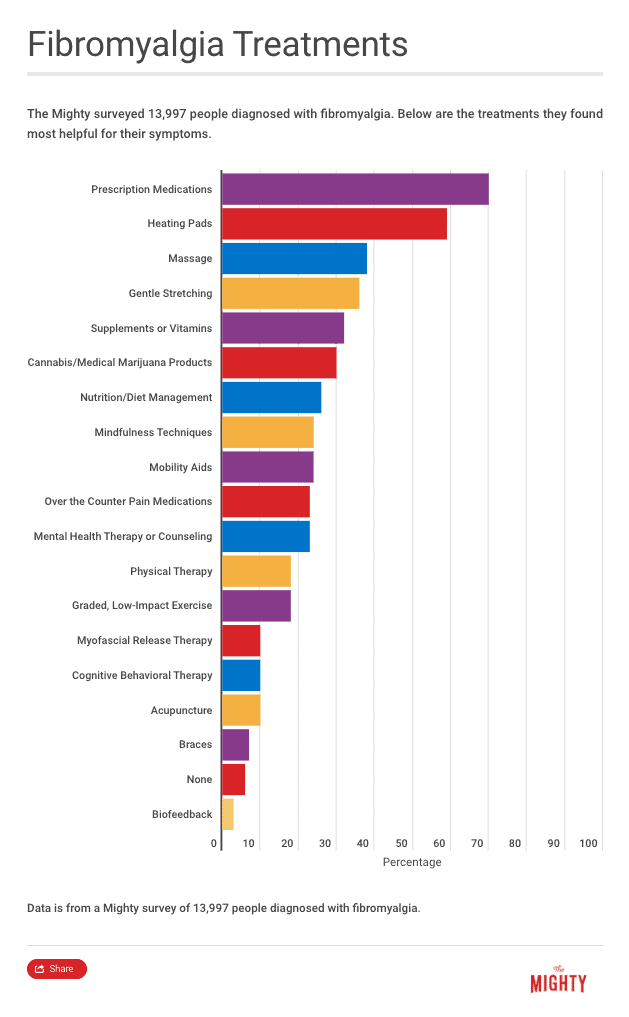
Medications are one avenue of treatment for fibromyalgia that should be used as part of a larger treatment plan that also includes psychological and physical strategies.
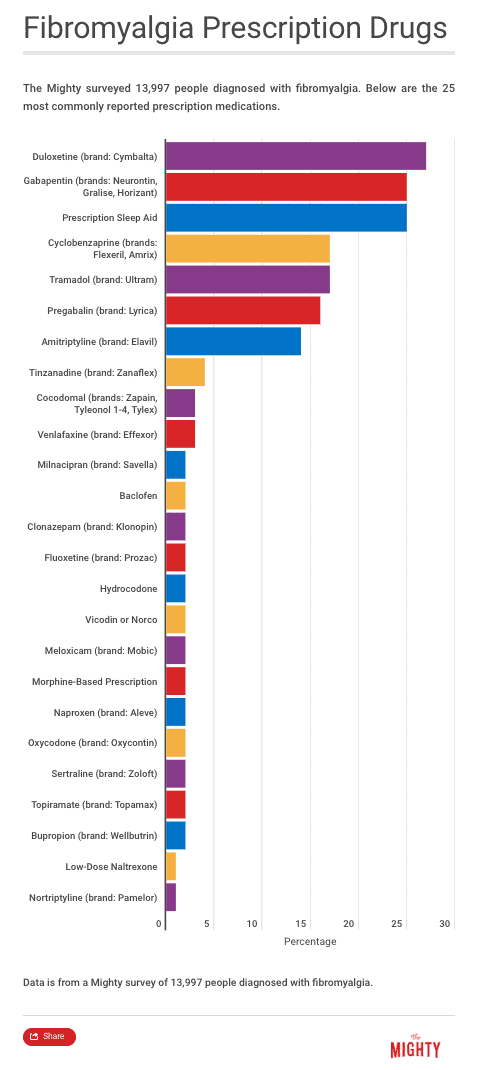
There are three medications officially approved as fibromyalgia treatment options: duloxetine (brand name Cymbalta), pregabalin (brand name Lyrica) and milnacipran (brand name Savella). Your doctor may also try other drugs off-label, meaning they will prescribe a drug that’s FDA-approved to treat conditions with symptoms similar to fibromyalgia. Most fibro-approved prescription medications are only helpful to 30 to 50 percent of patients who use them.12
When designing a medication treatment plan with your doctor, you will likely explore several different methods. If you have a doctor who tells you there’s nothing else you can do after trying only one or two meds, look for another doctors or specialist.14 You may need to try six or more medications to find one that works. Often doctors who don’t specialize in fibromyalgia are unaware of other options to try off-label.13
As with any medication, your doctor should explain what the drug does, how to take it and what it’s for. They should let you know how long until you might feel a difference, as well as what side effects you might experience. You may not need medication for life, but pain-reducing drugs can calm the overactive parts of your nervous system related to fibromyalgia pain.13 Bring up any questions or concerns about your medication with your doctor.
Duloxetine
Duloxetine (brand name Cymbalta) is a serotonin and norepinephrine reuptake inhibitor (SNRI) that’s commonly used to treat depression and anxiety. In 2008, the U.S. Food and Drug Administration (FDA) approved duloxetine for fibromyalgia pain because of its effectiveness and safety.24 Common side effects include dizziness, drowsiness, insomnia and nausea. Like all antidepressants, duloxetine includes a black box warning because it may increase suicidal ideation. Other serious possible side effects include liver damage, abnormal bleeding and severe skin reactions.7
Pregabalin
Pregabalin (brand name Lyrica) was the first drug approved by the FDA to treat fibromyalgia and other nerve pain-related conditions. It’s believed to help calm down your nervous system and reduce your pain and help you sleep better.3 The most common side effects are dizziness and sleepiness, though you may also experience, blurry vision, weight gain, trouble concentrating, swelling in your hands and feet, dry mouth and feeling “high” or euphoric. Pregabalin can increase the risk of suicidal thoughts and may cause serious allergic reactions like any drug.15 However, overall pregabalin is considered a safe medication.3
Milnacipran
Milnacipran (brand name Savella) was the third FDA-approved drug for fibromyalgia. It’s formulated as an SNRI, so it works like an antidepressant and increases neurotransmitters like norepinephrine. Research has shown it can help reduce fibromyalgia pain, fatigue and cognitive issues. Because it works like an antidepressant, it can also be helpful if you have symptoms of depression as well.19 The most common side effects are nausea, headaches, constipation, dizziness, insomnia, hot flush, excessive sweating, vomiting, palpitations and increased heart rate, dry mouth and increased blood pressure. It may also increase your risk of suicidal thinking and other serious complications, though these are rare.1
Gabapentin
Gabapentin (brand name Neurontin) was approved by the FDA in 1993 as a seizure medication. Its use was later expanded for postherpetic neuralgia, the nerve pain caused by shingles. Beyond these two uses, gabapentin is commonly prescribed off-label for fibromyalgia. The drug works by reducing the amount of chemicals nerve cells release that communicate pain. Gabapentin’s most common side effects include feeling dizzy or drowsy. It may also increase your risk for suicidal thoughts and cause a lack of coordination, nausea and vomiting, swelling in your legs and feet, vision problems and tremors.21
Other Prescription Drugs Your Doctor May Try
If you’ve tried the three FDA-approved drugs for fibromyalgia without any relief, consult a specialist about additional medication options. There are about 10 to 15 other medications your doctor may recommend off-label, especially if you don’t respond to the common fibromyalgia drugs.9
These might include:9, 10, 24
- Amitriptyline (brand name Elavil, an older type of tricyclic antidepressant)
- Bupropion (brand name Wellbutrin, an antidepressant)
- Cyclobenzaprine (brand name Flexeril, tricyclic antidepressant also used as a muscle relaxer)
- Fluoxetine (brand name Prozac, an antidepressant)
- Memantine18 (brand name Namenda, used to treat Alzheimer’s disease and dementia)
- Paroxetine (brand name Paxil, an antidepressant)
- Sertraline (brand name Zoloft, an antidepressant)
- Sodium oxybate (brand name Xyrem, used to treat the sleep disorder narcolepsy)
- Tizanidine (brand name Zanaflex, a muscle relaxant)
- Tramadol (brand name Ultram or ConZip, narcotic for pain relief)
- Venlafaxine (brand name Effexor, an antidepressant)
Low-dose naltrexone (brand name Revia), a medication used for those who have an opioid or alcohol dependence, has been shown in studies to help with fibromyalgia symptoms.14
The Future of Fibromyalgia Drug Treatments
Scientists and drug companies are researching other medication-based treatment options to find more options for fibromyalgia treatment in the future. For example, biomedical company EpicGenetics plans on conducting a clinical trial using the generic tuberculosis (TB) vaccine bacillus calmette-guerin (BCG). The vaccine has been used safely for TB since 1921 and now researchers will explore if it has potential for treating fibromyalgia.17 The trial hasn’t been conducted yet and how or if the BCG vaccine will be effective in treating fibromyalgia remains to be seen. Other approaches are likely also on the horizon.

Less Effective Treatments
Because one of your major symptoms of fibromyalgia is likely chronic pain, it seems only natural you might reach for over-the-counter painkillers, be prescribed opioids or try pain injections. These options may help some people, but because fibromyalgia impacts how your nervous system and brain processes pain, there is evidence these methods of pain reduction are less effective.
Over-The-Counter Painkillers
You might have noticed that over-the-counter painkillers like ibuprofen or acetaminophen (brand name Tylenol) don’t usually help. Over-the-counter painkillers belong to a class of drugs called analgesics that reduce a chemical in the brain called prostaglandins, responsible for inflammation and swelling. Essentially these medications raise your pain threshold so you don’t feel as much pain. The chemicals and processes that cause pain and inflammation in fibromyalgia are different, so over-the-counter painkillers are generally not effective.
Opioid Painkillers
A doctor might recommend opioid painkillers like oxycodone (brand name OxyContin) or hydrocodone (brand name Vicodin) to reduce fibromyalgia pain. Fibromyalgia experts typically recommend against using opioids because long-term opioid use increases the risk of addiction.12 In addition, preliminary research shows that opioids aren’t effective for fibromyalgia pain. When you have fibromyalgia, your endogenous opioid system — your natural pain relief system — doesn’t work quite right because your mu opioid receptor system may be impaired. Taking opioid painkillers likely won’t have the desired pain relief effect.22
Pain Injections
In some cases, your pain doctor may consider local steroid or anesthetic, trigger point or botox injections to reduce chronic pain. Most doctors use these treatments with caution and only if they believe they’ll be effective at shrinking your pain level.13 It’s difficult to pinpoint exactly where your pain may be coming from because the area of the body where you feel the pain may not be the source because of how your nervous system processes pain.5

Standard Treatment Options
Medication is only one treatment option for fibromyalgia, and medication alone is rarely enough to manage the condition. It’s best to use medication in combination with other standard treatment options such as movement exercises and cognitive behavioral therapy. Using these other treatment options can support a medication regimen and may be more effective than medication in many cases.12
Exercise and Mobility Programs
When you’re in a lot of pain, the last thing you want to do is move, but low-impact exercise and mobility treatments are crucial in managing fibromyalgia. Exercise is the most effective fibromyalgia treatment, with a 50 percent success rate among patients.2, 12 It should be a part of most fibromyalgia treatment plans.
Exercise here doesn’t usually mean running a marathon but rather taking the body through its full range of motion with light stretching, mobility exercises, strength training and graded exercises.5 Keeping the body moving reduces pain and may prevent worsening pain in the future. Some doctors may even encourage you to set a long-term physical goal. So for example, signing up for a charity walk or bicycle ride depending on your ability as a motivation to make exercise a priority in your treatment plan and provide a sense of accomplishment.13
Water therapy or hydrotherapy — performing physical exercises in a pool — reduce strain and impact on the body while allowing for a full range of movement. Mobility assistance devices, like canes or walkers, can also facilitate movement. Your fibromyalgia doctor or a physical therapist familiar with the condition can determine an exercise program that’s both manageable and helpful for you.
Cognitive Behavioral Therapy
Fibromyalgia isn’t a mental illness, but traditional mental health therapy can help. Cognitive behavioral therapy (CBT) teaches you skills to psychologically deal with chronic pain. A CBT program can help you cope with pain and reframe negative perceptions of having a chronic condition. It focuses on developing your strengths, and over time it has been shown to positively impact about 50 percent of fibromyalgia patients.12
CBT therapy also calms your nervous system over time through strategies to reduce your anxiety, stress and hypervigilance. CBT practices that have a calming effect may include mindfulness practices like deep breathing, guided imagery, meditation or yoga. A calmer nervous system generally means less fibromyalgia pain.5

Functional Medicine Approaches
Because so little is known about the exact cause of fibromyalgia, it calls for a creative treatment approach that combines the best of Western medicine with other evidence-based practices that are often considered “alternative.” This could include various therapies, lifestyle changes and natural supplements your doctor may suggest.
Alternative Therapies for Pain Reduction
You can try a variety of available pain reduction techniques and therapies to manage chronic fibromyalgia pain. This could mean applying heat or ice to painful areas of your body. You may choose to see a chiropractor or therapeutic massage therapist who specializes in fibromyalgia to reduce pain. Acupressure or acupuncture, which are designed to reduce pain and promote wellness, may also provide relief.
Myofascial Release Therapy
Myofascial Release Therapy was developed by a physical therapist to address fascia, a system of connective tissue in your body tied into your autonomic nervous system.14 Applying gentle, sustained pressure to the fascia slowly rehydrates these tissues to improve movement and reduce pain. Licensed practitioners know that where you feel fibromyalgia pain may come from another area in the body, and they work to apply pressure to those areas and loosen them up so you feel better.
Relaxation Techniques
Not only are relaxation techniques good for your psyche — and the stress of dealing with a chronic illness — they have a calming effect on your nervous system’s fight-or-flight response, which may provide some symptom relief. Try activities like meditation, relaxation exercises, yoga, breathing techniques and even aromatherapy. Biofeedback, a therapy where sensors are attached to your body as a way to gain more control over your body’s automatic responses to stress, may also be worth looking into.11
Natural Supplements
A wide variety of natural supplements on the market are advertised for fibromyalgia or chronic pain but consult with your doctor before trying any of these. Some supplements are useless, and others prevent your prescription medications from working or cause dangerous interactions.
One natural product your doctor might recommend is 5-hydroxytryptophan (5HTP).5 This chemical occurs naturally in your body and is a precursor to serotonin. Supplementing 5HTP may help your body naturally increase its serotonin production, which might reduce fibromyalgia symptoms. You also have a significant amount of serotonin in your gut, so increasing your overall serotonin levels improves common fibro complications like irritable bowel syndrome (IBS).5
Though there aren’t as many (or sometimes any studies) showing their effectiveness, some doctors might recommend alternative supplements to help your symptoms. This could include somnolin, which can help you sleep better.5 Ashwagandha, also referred to as Indian ginseng, may reduce stress, pain and fatigue, according to at least one study.5, 6 Chamomile may calm the nervous system without the “zombie” effect of some traditional medications.5, 16
An increase in inositol — aka vitamin B8 — also has some research showing it can help with depression or anxiety, and therefore maybe also fibromyalgia symptoms.5,20 Check with your doctor about additional options for managing your condition and before starting a supplement because sometimes they can interact with your other medications.
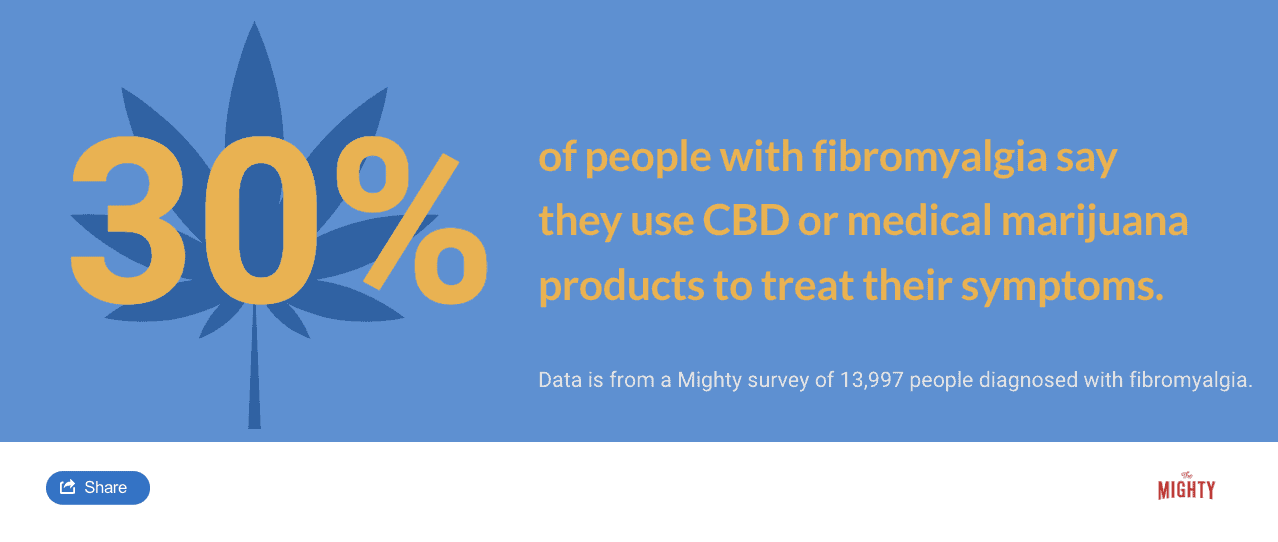
CBD Products
Cannabidiol (CBD) — a part of the cannabis plant that will not get you high — may benefit many painful conditions, including fibromyalgia.4 Your body actually produces cannabinoids on its own. Though more research is needed, it’s believed that CBD interacts with your cannabinoid receptors or encourages the body to make more of its own cannabinoids.
Many find CBD products relieve pain and have other healing properties.14 CBD from hemp is legal in most U.S. states now, even if recreational marijuana is not. It’s not FDA-approved for fibromyalgia use, and there is still no convincing scientific evidence that its use benefits fibromyalgia symptoms. It did, however, receive approval to treat epilepsy in 2018, so its acceptance as a viable medical treatment is expanding in other areas.4
Diet Changes
Making lifestyle changes to your diet helps some people with fibromyalgia. These changes could include reducing your dairy intake, avoiding inflammatory foods and consuming more protein to boost your energy. Your doctor and several self-help resources suggest diets that might work, which will be different for everyone with fibromyalgia.
Related: Here are some ways people describe what it’s like living with fibromyalgia.
- “23 Truths People With Fibromyalgia Wish Others Understood“
- “25 ‘Habits’ of People With Fibromyalgia“

Treating Other Fibromyalgia Complications
Fibromyalgia is way more than chronic pain and two of the most challenging parts of living with the condition are fatigue and mental health issues. In addition to managing your pain, finding a treatment that might help clear out some of your brain fog and taking care of any body function issues like constipation and diarrhea, make sure your doctor takes into account these other complications of fibromyalgia.
Fatigue
Fatigue is a major component of fibromyalgia, making it important to work on getting restorative sleep. Addressing sleep issues has a preventative and protective function in addition to helping you function better. Because your sympathetic nervous system stays in high-alert mode, you rarely get to a place of deep, restorative sleep with fibromyalgia. This leads to that constant fatigue, and it can make any brain fog or memory problems you’re experiencing worse. You might consider a sleep disorder specialist to learn insight into your sleep issues and address other comorbid sleep disorders like sleep apnea. Regular sleep medications likely won’t be helpful because they don’t impact your deep sleep needs.
Go back to basics with your sleep hygiene to set yourself up for sleep success.13 Avoid caffeine and alcohol in the hours before you go to sleep. Reduce your screen time and shut down the bright electronics before bed. Turn off stimulating movies and videos games before going to bed. Take a bath or engage in other soothing practices right before bedtime to calm down. Make sure your sleep space is comfortable and inviting, from the feel of the sheets on your body to the temperature in the room. Stick with a sleep schedule so your body gets used to a routine. All of these simple techniques can be helpful.
Mental Health
Fibromyalgia is not a mental health condition, but when you live with fibromyalgia it’s common to have a comorbid mental illness. People with fibromyalgia are three times as likely to be diagnosed with depression.8 Anxiety disorders and post-traumatic stress disorder (PTSD) are also common. Mental health symptoms sometimes overlap with fibromyalgia symptoms, so talk to your doctor or mental health professional. In addition to CBT practices for pain management, consider adjunct mental health therapy to address mental illness and build your emotional support system.
Learn More About Fibromyalgia: Overview | Symptoms | Diagnosis | Treatment | Resources | Related Conditions

Sources
- Allergan. (2016). Medication Guide: Savella. Retrieved from https://www.savella.com/SavellaMedicationGuide.pdf
- Bhana, S. (2017). Fibromyalgia. Retrieved from https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Fibromyalgia
- Boomershine, C. (2010). Pregabalin for the management of fibromyalgia syndrome. Journal of Pain Research, 81. doi:10.2147/jpr.s7884
- Borgelt, L. M., Franson, K. L., Nussbaum, A. M., & Wang, G. S. (2013). The Pharmacologic and Clinical Effects of Medical Cannabis. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy,33 (2), 195-209. doi:10.1002/phar.1187
- Brady, D. (2018). Fibromyalgia [Telephone interview].
- Chandrasekhar, K., Kapoor, J., & Anishetty, S. (2012). A prospective, randomized double-blind, placebo-controlled study of safety and efficacy of a high-concentration full-spectrum extract of ashwagandha root in reducing stress and anxiety in adults. Indian journal of psychological medicine, 34(3), 255-62.
- Eli Lilly and Company. (2016). Medication Guide: Cymbalta. Retrieved from http://pi.lilly.com/us/Cymbalta-Medguide.pdf
- Fibromyalgia | Arthritis | CDC. (2017). Retrieved from https://www.cdc.gov/arthritis/basics/fibromyalgia.htm
- Fibromyalgia Information Foundation. (n.d.). Commonly Used Drugs. Retrieved from http://myalgia.com/Treatment/Drugs%20.htm
- Forte, M. L., Butler, M., Andrade, K. E., Vincent, A., Schousboe, J. T., & Kane, R. L. (2015). Treatments for Fibromyalgia in Adult Subgroups. Comparative Effectiveness Reviews, 148. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK274474/
- Frank, D. L., Khorshid, L., Kiffer, J. F., Moravec, C. S., & McKee, M. G. (2010). Biofeedback in medicine: Who, when, why and how? Mental Health in Family Medicine,7(2), 85-91.
- Gerwin, R. D. (2018). Fibromyalgia [Telephone interview].
- Jenner, C. (2018). Fibromyalgia [Telephone interview].
- Liptan, G. (2018). Fibromyalgia [Telephone interview].
- Lyrica. (n.d.). Retrieved from https://www.lyrica.com/
- Mahjoub, F., Salari, R., Noras, M. R., & Yousefi, M. (2017). Are Traditional Remedies Useful in Management of Fibromyalgia and Chronic Fatigue Syndrome? A Review Study. Journal of evidence-based complementary & alternative medicine, 22(4), 1011-1016.
- Migdol, E. (2018). A Clinical Trial Is About to Begin Testing a New Fibromyalgia Treatment. Retrieved from https://themighty.com/2018/09/fibromyalgia-clinical-trial-bcg-epicgenetics-bruce-gillis/
- Olivan-Blázquez, B., Herrera-Mercadal, P., Puebla-Guedea, M., Pérez-Yus, M., Andrés, E., Fayed, N., . . . Garcia-Campayo, J. (2014). Efficacy of memantine in the treatment of fibromyalgia: A double-blind, randomised, controlled trial with 6-month follow-up. Pain, 155(12), 2517-2525. doi:10.1016/j.pain.2014.09.004
- Ormseth, M. J., Eyler, A. E., Hammonds, C. L., & Boomershine, C. S. (2010). Milnacipran for the management of fibromyalgia syndrome. Journal of pain research, 3, 15-24.
- Palatnik, A., Frolov, K., Fux, M., & Benjamin, J. (2001). Double-Blind, Controlled, Crossover Trial of Inositol Versus Fluvoxamine for the Treatment of Panic Disorder. Journal of Clinical Psychopharmacology, 21(3), 335-339. doi:10.1097/00004714-200106000-00014
- Pfizer. (2017). NEURONTIN® (gabapentin) Medication Guide. Retrieved from https://www.pfizermedicalinformation.com/en-us/neurontin/medguide
- Schrepf, A. (2018). Fibromyalgia [Telephone interview].
- Wait, M. (2018). Is a Pain Clinic Right for You? Retrieved from https://www.arthritis.org/living-with-arthritis/pain-management/chronic-pain/pain-clinic.php
- Wright, C. L., Mist, S. D., Ross, R. L., & Jones, K. D. (2010). Duloxetine for the treatment of fibromyalgia. Expert review of clinical immunology, 6(5), 745-56.

