Hereditary angioedema (HAE) is a rare genetic disorder that causes sudden, recurring episodes of severe swelling in different parts of the body. These swelling attacks — called “angioedema” — can affect the skin, gastrointestinal tract, and even the airways, sometimes becoming life-threatening if the throat or tongue is involved.
Although it’s uncommon, HAE can be deeply disruptive. People who live with it often face unpredictable symptoms that interfere with daily life, from pain and fatigue to anxiety about when the next attack will strike.
Understanding the Basics
Hereditary angioedema is “hereditary” because it’s passed down through families — caused by changes (mutations) in the SERPING1 gene or, more rarely, the F12 gene. These genes are responsible for producing a protein called C1 inhibitor (C1-INH), which helps regulate inflammation and fluid movement within blood vessels.
In most people with HAE, this protein is either missing, not working properly, or present in too low amounts. Without enough functioning C1 inhibitor, the body loses control over a system that normally helps balance fluid levels. As a result, small blood vessels can leak fluid into nearby tissues, leading to episodes of swelling that are often painful and dramatic.
Unlike allergic swelling (such as hives), HAE attacks are not caused by histamine, which means they don’t respond to common allergy medications like antihistamines, corticosteroids, or epinephrine. This can make the condition especially frightening or confusing until a proper diagnosis is made.
Types of Hereditary Angioedema
Doctors classify HAE into three main types based on the specific genetic and biochemical causes.
-
Type I HAE – This is the most common form, accounting for about 85% of cases. People with type I HAE have low levels of C1 inhibitor.
-
Type II HAE – In this type, C1 inhibitor levels are normal or even elevated, but the protein doesn’t function properly. It’s like having the right amount of workers — but they’re not doing their jobs effectively.
-
Type III (or HAE with normal C1-INH) – This is the rarest form and often linked to mutations in the F12 gene. C1 inhibitor levels and function appear normal, but the person still experiences HAE symptoms. It’s seen more frequently in women and may be influenced by hormonal factors, such as estrogen.
Each type causes similar symptoms, but identifying which kind someone has helps guide treatment decisions.
Symptoms and What They Feel Like
HAE attacks can happen anywhere in the body, but they most commonly affect:
-
Skin: Swelling often occurs in the hands, feet, face, or genitals. It’s usually not itchy, but it can be tight, painful, and disfiguring.
-
Abdomen: When swelling happens in the digestive tract, it can cause intense cramping, nausea, vomiting, and diarrhea — symptoms often mistaken for appendicitis or other gastrointestinal issues.
-
Airways: The most dangerous attacks involve the tongue, throat, or larynx (voice box). Swelling in these areas can block breathing and require emergency medical care.
An attack can develop slowly over several hours, peak within 12–36 hours, and then fade over the next two to five days. Some people experience warning signs before an episode, like tingling, fatigue, irritability, or a non-itchy rash.
The frequency of attacks varies widely. Some people have only a few per year, while others have multiple episodes each month. Common triggers include:
-
Physical trauma (even mild injury or dental work)
-
Emotional stress
-
Hormonal changes, such as menstruation or pregnancy
-
Infections
-
Certain medications, especially ACE inhibitors (used for blood pressure) and estrogen-containing birth control pills
How HAE Differs From Other Forms of Angioedema
Many people first encounter angioedema as part of an allergic reaction. However, HAE has distinct differences:
| Feature | Allergic Angioedema | Hereditary Angioedema |
|---|---|---|
| Cause | Triggered by allergens (food, insect stings, etc.) | Genetic mutation affecting C1 inhibitor |
| Response to Antihistamines/Steroids | Usually improves | Typically no effect |
| Onset | Minutes to hours | Hours to days |
| Accompanied by Hives? | Often | Rarely |
| Family History | Usually absent | Often present |
Because HAE attacks don’t respond to typical allergy medications, misdiagnosis is common — sometimes for years. Awareness among doctors and patients has improved, but early recognition remains a key challenge.
Getting a Diagnosis
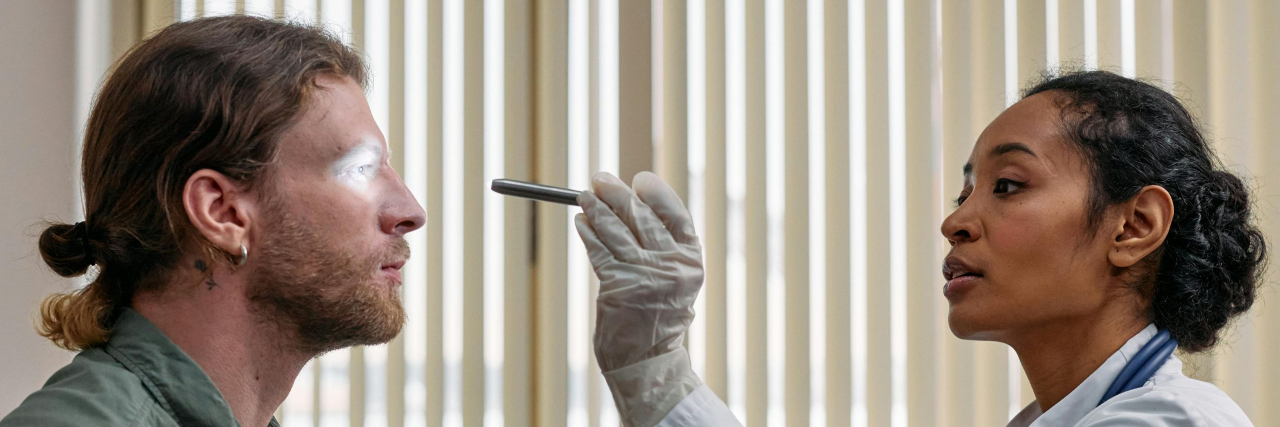
If HAE is suspected, a doctor (often an allergist or immunologist) will perform blood tests to measure both the level and function of C1 inhibitor and complement component 4 (C4), a related protein that’s typically low during and between attacks.
A genetic test may also confirm the diagnosis and identify the exact mutation. Since HAE runs in families, once one person is diagnosed, relatives are often tested as well — even if they don’t yet have symptoms.
Treatment Options
While there’s no cure for hereditary angioedema yet, there are several effective treatments that can both prevent and manage attacks. Treatment generally falls into two categories: on-demand (acute) and preventive (prophylactic).
1. On-Demand (Acute) Treatments
These are used to stop swelling once an attack begins. They work best when taken early. Options include:
-
C1 inhibitor replacement therapy (Berinert®, Ruconest®) – Provides the missing or malfunctioning protein directly.
-
Kallikrein inhibitors (ecallantide, icatibant) – Block a chemical pathway that leads to swelling.
-
Fresh frozen plasma – In emergency settings where other medications aren’t available, plasma can temporarily restore C1 inhibitor levels.
2. Preventive Treatments
These reduce the frequency or severity of attacks. Preventive options include:
-
C1 inhibitor infusions given regularly (e.g., Cinryze® or Haegarda®).
-
Kallikrein inhibitors like lanadelumab (Takhzyro®) or berotralstat (Orladeyo®), taken by injection or orally.
-
Hormone management – For people whose attacks are linked to hormonal changes, adjusting medications like birth control may help.
Emergency plans are essential for anyone with HAE, especially since throat swelling can escalate quickly. Many patients carry their medication with them and teach family or coworkers how to administer it if needed.
Living With Hereditary Angioedema
Because HAE is unpredictable, it can take a toll not just physically, but emotionally. Many people describe the constant fear of an attack as one of the most complex parts of the condition. Swelling in visible areas, such as the face, can be distressing, while abdominal and airway attacks can make it difficult to work, travel, or make plans.
Support from healthcare providers, mental health professionals, and patient communities can make a big difference. Organizations like the US Hereditary Angioedema Association (HAEA) provide education, resources, and connections with others who understand the condition firsthand.
Lifestyle management can also help:
-
Keep a symptom diary to track potential triggers and attack patterns.
-
Manage stress through mindfulness, therapy, or gentle exercise.
-
Avoid medications known to worsen symptoms, like ACE inhibitors or estrogen-based therapies.
-
Stay prepared with access to on-demand treatment, especially during travel or stressful events.
Outlook and Hope for the Future
Advancements in HAE treatment have transformed what living with the condition looks like. A few decades ago, people often faced frequent, debilitating attacks and limited options. Today, targeted medications can help many patients prevent or quickly control swelling episodes.
Ongoing research is exploring gene therapies and next-generation drugs that could one day correct the underlying cause, rather than just treating symptoms. For people living with hereditary angioedema — and their families — that progress represents real hope.
The Bottom Line
Hereditary angioedema is a rare but serious condition caused by a genetic defect in the body’s ability to regulate swelling. While it can be unpredictable and sometimes dangerous, understanding the condition and accessing the right treatments can make a tremendous difference.
If you or someone you know experiences unexplained swelling — especially without hives and unresponsive to allergy medicine — talk to a doctor familiar with rare immunologic conditions. Early diagnosis saves lives and opens the door to treatments that allow people with HAE to live full, safe, and empowered lives.