I wake up, heart racing, cold sweats, head pounding, room spinning. Head to toe it feels like my body is on fire. The paramedic crew greets me and knows I wouldn’t be in an ambulance unless something was truly wrong.
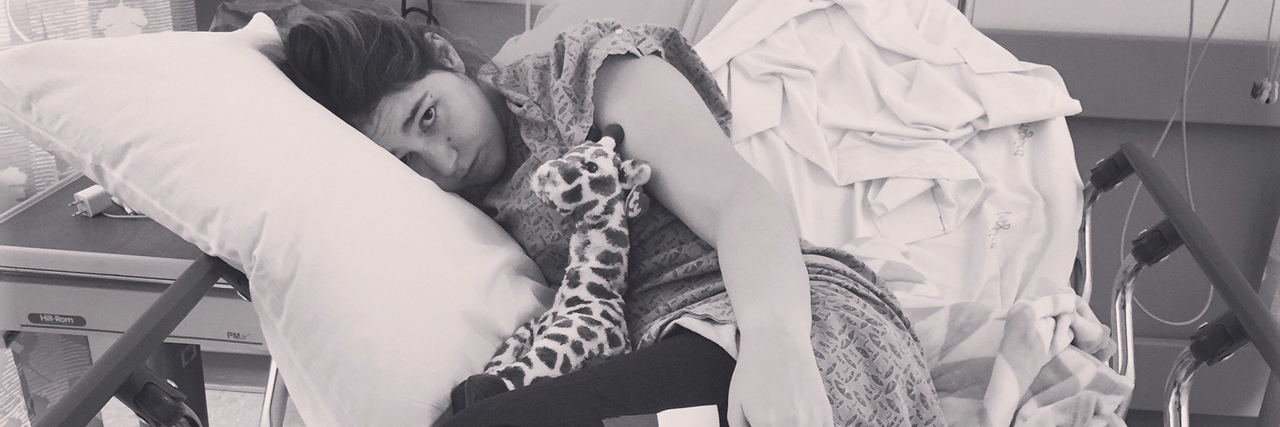
My exceptional coworkers get me to the hospital just in time for them to announce I’m a “code sepsis.” My white blood cell count had escalated over 82,000. A number that should never reach over 10,000. Familiar terms for me in my career, but to my family, I was just sick and no one knew why. I was admitted to the intensive care unit (ICU) for what felt like days. I started having seizures, I became completely paralyzed on the right side of my body. I was losing my vision and hearing. I was terrified. Terrified for my life, terrified for my family and terrified because in my whole career I’ve never seen or heard of anything like this.
Apparently the doctors hadn’t either. I was seen by a neurologist, cardiologist and general medicine. Hospitals are places of business, and its a job for doctors to talk to patients all day. Instead of just going about their regular routine, I wish they would have taken the time to get to know me and my case specifically. I don’t want to feel like a number on a piece of paper that they’re just trying to fix then discharge as fast as they can. Even though that is the game for most hospitals, bed side manner goes a long way. Especially with spoonies who happen to make their appearances to hospitals on the regular. For those who work in a hospital, if you recognize a patient because they were just there a couple weeks ago, don’t say “Hey, weren’t you just here?” Because yes, I was, and now I’m flaring and I’m back again, obviously. Just talk to me like a normal person and ask me how my day is going.
On the third day of my stay in ICU, the infectious disease doctor made an appearance. I will never forget the words of this doctor as he shook his head at me and told me I was faking because he couldn’t find anything wrong with me. This doctor decided to blame his failure in being able to provide a proper diagnosis, on me, the patient. I was weak, exhausted, in pain but I argued. I explained to him my symptoms over and over. I was angry that he discounted my symptoms.
This is something I’ve been guilty of in my career. I’ve heard a patient complaint and discounted it for something less severe, just to find out it really was more serious. Call it karma, but I was infuriated as he stormed out and insisted I needed a psych evaluation. If theres anything I know well, its mental health patients. I work in emergency medical services (EMS) in one of the biggest cities with the highest call volumes a year and a lot of them happen to be mental health related. This was not mental health related. In the span of 24 hours I stopped being able to walk or care for myself and no one knew why.
It took nine months, a lot of money, patience and frustrations to figure out some of my diagnosis. Systemic lupus erythematosus, epilepsy secondary to a misdiagnosed brain tumor, Sick sinus syndrome, super ventricular tachycardia (SVT) and gastroparesis. Everyone, including new members of my care team always say, “Oh my gosh, you’re so young to have all these diagnoses.” I always just nod and go, “Yeah I know. But I rather be diagnosed than undiagnosed and not know why my body is so angry with me.”
Please don’t remind us with chronic illnesses of how sick we are. It’s constantly something were concerned with. If you feel the need to comment, phrases such as, “I hope things are going well for you,” or, “I hope you’re feeling good today,” are better alternatives.
As I look back at the nine months of pure hell I endured trying to get to the bottom of my diagnosis, I want to remind my fellow healthcare providers of a few things. If a patient with a chronic illness has pain, there is a 99.9 percent chance they’re really in pain and it should be dealt with appropriately. Don’t ever doubt someone is having pain just because their diagnosis doesn’t add up to you. Everyone’s symptoms of their chronic illness are different and patients should be treated with respect – regardless of how many times they are seen by a doctor or admitted to a hospital.
Don’t push a patient past their limits. If they’ve had enough physical therapy for the day, tube feedings are not going well or infusions are causing side effects, take a break. Our bodies cant handle a lot thrown at us at once. We move slowly but eventually we will get to the finish line!
As for my spoonie friends, don’t give up, keep fighting. I spent the better part of the last nine months of 2017 in hospitals. Over 60 days in patient, 90 days of physical therapy and three surgeries. You will always be the biggest advocate for your health, so speak up. No one knows what you’re feeling but you. It will be frustrating, exhausting and tears will be shed but better days are ahead of you.