Are Chronic Illness and Trauma Related? Here's What You Need to Know.
If you’ve been diagnosed with a chronic illness and experienced trauma, you may have some uneasy feelings about the connection between the two. After all, some doctors who don’t really understand tricky conditions like fibromyalgia or myalgic encephalomyelitis (ME/CFS), for example, might be quick to tell you your symptoms are “all in your head” or due to a mental health condition.
While living with a chronic illness can be traumatic, research shows the reverse may be true as well. Trauma, especially if it happens when you’re younger, can trigger chronic illness. It’s not that simple of course — trauma isn’t the only factor that determines whether or not you get a chronic illness and it’s not associated with all conditions. And it’s worth mentioning, just because you have a chronic illness does not mean you experienced trauma.
It’s important to talk about how trauma may impact chronic illness because knowing the connection can improve your treatment options and encourage doctors to look at your health from a holistic, mind-body perspective. In addition, some researchers hope early intervention and prevention of trauma may reduce the number of people who develop chronic illness in the future.
Connecting Trauma and Chronic Illness
The connection between chronic illness and trauma is complex because both affect your body and your mind. When you experience trauma like physical or sexual abuse, a major accident or military combat, the impact isn’t just “all in your head. Trauma affects your mental health and your nervous system, this is especially true if you develop post-traumatic stress disorder (PTSD).
Trauma-related symptoms like hypervigilance keep your nervous system perpetually locked in an overactive state. As part of your fight-or-flight response to trauma (perceived danger), your nervous system preps your body for action (or inaction in the case of the freeze response). This includes changes to how your immune system is working, which can lead to higher inflammation in your body. Researchers hypothesize inflammation may be a key connection to chronic illness.
According to Karestan C. Koenen, Ph.D., a researcher and professor of psychiatric epidemiology at Harvard University, it’s possible mental and chronic illness in some cases can be connected through inflammation. Higher inflammation levels may be a factor in what causes some mental illnesses, including PTSD and depression. Higher levels of inflammation have also been connected with certain chronic illnesses, best studied so far in heart disease and type 2 diabetes.
Other theories implicate the stress hormone cortisol, which rises during a traumatic or stressful event. When your cortisol levels are out of whack thanks to the lasting impact of trauma or PTSD, your body goes ahead and creates more cortisol. Too much cortisol reduces your immune system’s effectiveness and makes you susceptible to infection. If your system stays stuck in trauma mode, eventually you won’t release enough cortisol and that leads to unnecessary inflammation. Either scenario may make you more susceptible to developing chronic illness.
What Is Epigenetics?
Experiencing trauma alone isn’t usually enough to cause chronic illness, which is where epigenetics comes in. Your risk of getting a chronic illness is often a combination of a predisposition for a condition in your genes and then a trigger from the environment that “switches on” and activates the illness. This is referred to as epigenetics. You can also think of it like a gun — genetics loads the bullet and the environment pulls the trigger.
In the context of chronic illness, there are a variety of environmental factors that may contribute to your risk of developing a condition. Common triggers include experiencing trauma, having an infection or smoking. For many illnesses, traumatic stress that happens when you’re a child or adolescent makes you especially susceptible to developing a chronic condition. An epigenetic risk for a condition can also be inherited and passed down to you by a relative, like a parent, who experienced trauma before you were born.
While trauma can sometimes be the primary trigger of your chronic illness, it can also cause secondary triggers that increase your risk of having a condition. With changed cortisol levels, for example, having too much cortisol weakens your immune system and you’re more likely to get an infection. Research shows some chronic illnesses may be triggered by a significant infection such as the Epstein-Barr virus or Lyme disease.
Sometimes the trigger may be linked to how you cope with trauma. “We know that developing PTSD is associated with changing certain health behaviors … that can then be a risk for chronic disease,” Koenen told The Mighty. She pointed out trauma and PTSD can lead to behaviors that are known chronic illness triggers, like smoking, as well as increased drug or alcohol use, getting less exercise, diet changes or weight gain.
Can Trauma Cause Your Chronic Illness?
Trauma, toxic stress and PTSD have now been directly linked to several types of chronic illnesses, including heart disease, type 2 diabetes, autoimmune disorders like rheumatoid arthritis and lupus, chronic pain, digestive conditions like irritable bowel syndrome (IBS), and fibromyalgia. Other chronic illnesses, like multiple sclerosis, may be impacted by some of the secondary effects of trauma, like smoking or infection risk.
“We find that PTSD, but also depression, are associated with a lot of different chronic diseases. So it doesn’t seem to be that they affect just one system,” Koenen, who first wondered about the connection between chronic and mental illness while working with veterans, said. “What’s really striking is that these mental health conditions really do seem to adversely affect the physical health over the life course, especially as one ages.”
Fibromyalgia, a condition that causes chronic pain, fatigue and thinking and memory issues, is strongly linked with trauma. Partly this may be because fibromyalgia is best understood as a hyperactive nervous system disorder — your fibro symptoms and trauma responses are caused by a similar type of overactive process in your autonomic nervous system, which controls automatic body functions like your heart rate.
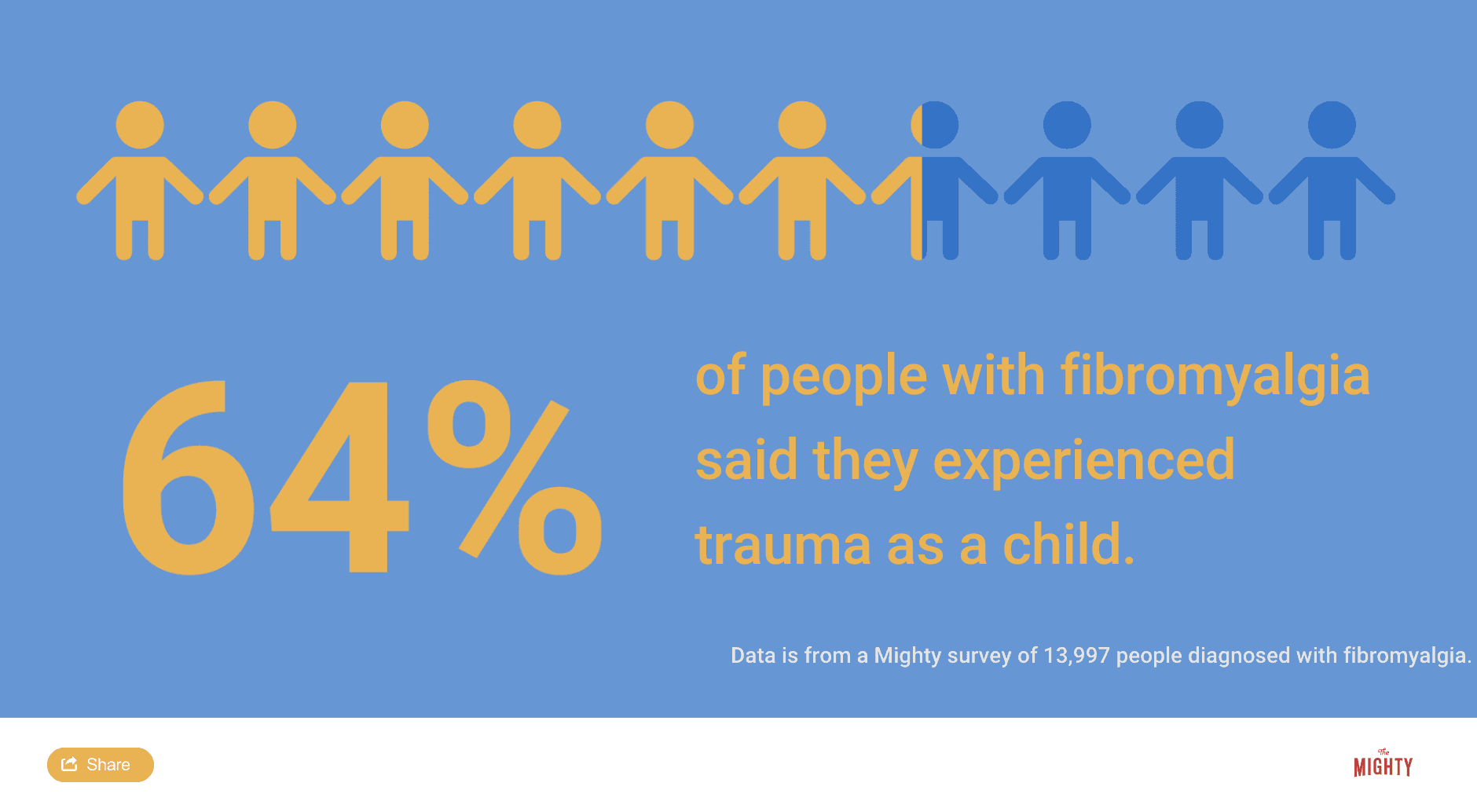
In the case of fibromyalgia, research shows women who experience trauma, like abuse, military combat or a car accident that causes whiplash, in their early teen years are most likely to develop fibromyalgia. But it’s not just women. According to Ginerva Lipton, M.D., almost half of men with military combat-related PTSD met the diagnostic criteria for fibromyalgia. Another study found 80% of military combat veterans with PTSD also experienced chronic pain. In a Mighty survey of nearly 14,000 people diagnosed with fibromyalgia, 64% reported experiencing trauma as a child.
What This Means for Health Care (and You)
If you live with chronic illness, it can be helpful to know how trauma may have your diagnosis, but it might not seem like there’s much you can do about it now. A couple of studies have shown treating PTSD symptoms may improve your overall physical health too. Koenen said this is one area of research she’s hoping to dig into to see how treating trauma might impact chronic illness.
“If we treat mental health better, we treat PTSD better, and depression, and we treated them effectively, would we reduce the reduce the risk of these chronic diseases?” Koenen asked. “The big question is about reversibility. … If you treat PTSD effectively, would it remove this extra risk of these chronic diseases? Or do you have to treat it within a certain time? Do you have to treat it within the first year or anytime will it increase, improve the outcome?”
Doctors also need to recognize it’s important to integrate physical and mental health when addressing your chronic illness. Complementary and alternative medicine practices take a mind-body approach to health, Koenen said, which is one reason why these treatment options are growing in popularity among chronic illness patients. Though chronic illness is not a mental health condition or “all in your head,” your doctor should consider the impact of past trauma or toxic stress on your current symptoms to make sure you’re exploring all available treatment options.
“Very little in our health system integrates mental health and physical health,” Koenen said, adding:
Despite this, I think the evidence is pretty overwhelming that the two are related. But as a patient, you’re stuck with all your specialists who generally don’t talk to each other. And so that just speaks to the whole way we structure health care and the fact that we treat the brain as if it’s separate from the rest of the body and the way the system’s set up. … Improving [the health care] system would probably improve outcomes, and in the long run, cost less money.
If you want to know more about living with chronic illness and PTSD or trauma, check out these other stories from The Mighty community:
Header image via StudioM1/Getty Images

