First, let’s get one thing straight: substance use disorder (SUD) is a disease, not a character flaw or a choice.
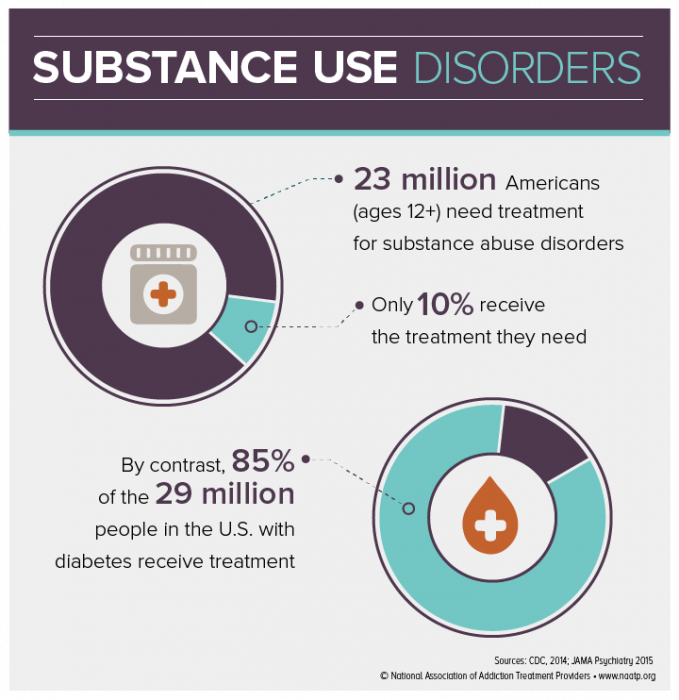
One in 7 Americans, each a unique story, tied together by the common thread of substance use disorder. Yet contrary to popular belief, they’re not broken or willfully choosing this path. This medical condition requires more awareness, compassion, and understanding.
What Is Substance Use Disorder?
We’ve all heard the term “addiction.” Still, when we delve into the medical side, the phrase we often encounter is substance use disorder. SUD is a medical condition characterized by an inability to stop using a substance, despite harmful consequences.
The impairment or distress can manifest in social, occupational, or educational settings. It’s not just “a bad habit”; it’s a complex interplay of psychological, social, and biological factors significantly affecting an individual’s life.
The term “disorder” often raises eyebrows. Someone struggling with SUD may wonder, “Does this mean I’m broken?” Absolutely not. In the medical world, the word helps health care professionals communicate about a set of symptoms that are affecting your well-being.
You have a medical condition that needs management. That’s the lens through which we should view SUD — a medical condition that can be managed and treated.
The Biology of Substance Use Disorder
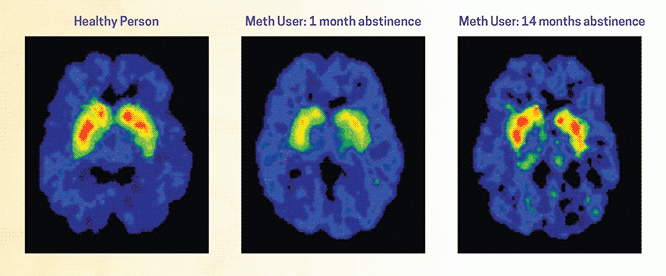
Our brains are wired to seek pleasure and avoid pain — a survival mechanism. The introduction of substances can hijack this “reward system,” making the brain prioritize substance use over other survival behaviors like eating or social bonding. The more often you use, the more your brain becomes accustomed to these heightened neurotransmitters, and the harder it becomes to derive pleasure from other, healthier sources.
The story of SUD starts in the brain, particularly with neurotransmitters like dopamine and serotonin, which are key players in our mood and emotions. When substances like alcohol, opioids, or stimulants enter the system, they can interfere with or enhance the production of these neurotransmitters. The result? A feeling of pleasure or “high.” Over time, the brain adapts and starts to rely on these substances to feel good, a state known as chemical dependency.
As the body becomes more accustomed to the presence of a substance, the initial amount no longer provides the same high. This phenomenon is known as tolerance. A person has to consume more to achieve the desired effect, leading to a vicious cycle. When the substance is unavailable, withdrawal symptoms kick in, ranging from irritability and nausea to severe conditions like hallucinations and seizures. These are physical markers of dependency.
When Do You Have a Substance Use Disorder?
The diagnosis of SUD is based on specific criteria outlined in the “Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition” (DSM-5). Here’s a simplified version:
- Using more than you are meant to, or for a longer time than you planned.
- Trying but failing to cut down or control how much you use.
- Spending a significant amount of time and effort obtaining, using, or recovering from the substance.
- Experiencing withdrawal symptoms or needing to use more of the substance to achieve the desired effect (tolerance).
Types of Substance Use Disorders
When we talk about substances, we’re referring to a broad range of items that can impact your mental, emotional, or physical state. SUD is classified into several types based on the specific substance involved. Each type has its unique symptoms, challenges, and treatment approaches. Here’s a quick rundown:
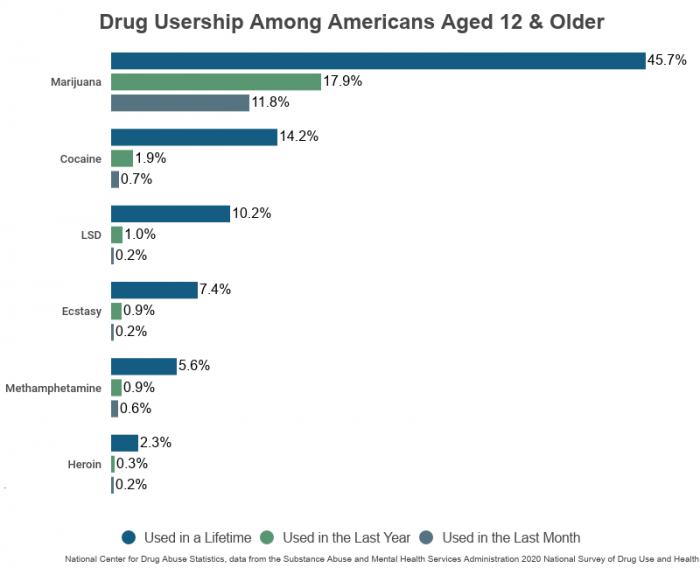
- Alcohol use disorder (AUD): Chronic misuse of alcohol, ranging from binge drinking to alcoholism. Impacts liver, cardiovascular health, and cognition.
- Opioid use disorder: Involves prescription opioids like morphine, oxycodone, or illegal opioids like heroin that have a high risk for addiction and overdose.
- Benzodiazepine use disorder: Includes medications such as Valium and Xanax, often prescribed for anxiety or insomnia. It can lead to dependence and withdrawal symptoms.
- Stimulant use disorder: Pertains to medications like adderall and ritalin or illegal stimulants like cocaine and methamphetamine. There is a high risk for misuse and severe health consequences.
- Tobacco use disorder: Involves using tobacco products like cigarettes, cigars, and chewing tobacco. It is highly addictive and leads to lung and heart diseases.
- Cannabis use disorder: Chronic misuse of cannabis products like marijuana. It can result in cognitive impairment and increased risk of psychosis in predisposed people.
- Hallucinogen use disorder: Includes substances like LSD, peyote, and magic mushrooms. It is less common but can have significant psychological effects.
- Inhalant use disorder: Involves inhaling volatile substances like glue, aerosol sprays, or solvents. It is dangerous and can lead to sudden death.
- Sedative, hypnotic, or anxiolytic use disorder: Involves the misuse of medications often prescribed for sleep disorders or anxiety, including some benzodiazepines and barbiturates.
- Polysubstance use disorder: Concurrent use of multiple substances complicates diagnosis and treatment.
- Caffeine use disorder: While generally considered to be of lower risk compared to other substances, excessive caffeine consumption can lead to insomnia, heart palpitations, and digestive issues.
- Club drug use disorder: Involves substances commonly used in nightlife settings, like MDMA (“ecstasy”), GHB, and ketamine. These can lead to various health risks, including severe dehydration and cognitive impairments.
- Phencyclidine (PCP) use disorder: This disorder is related to using PCP or similarly acting arylcyclohexylamines. It can cause hallucinations, impaired motor coordination, and severe agitation.
- Anabolic steroid use disorder: Concerns the misuse of anabolic-androgenic steroids often used for muscle building. It can cause hormonal imbalances, aggressive behavior, and increased risk of heart disease.
- Over-the-Counter medication use disorder: Some over-the-counter (OTC) medications, such as cough syrup containing dextromethorphan, can be misused and lead to dependence.
- Novel psychoactive substances use disorder: This term refers to various “designer drugs” chemically engineered to mimic established illegal drugs. Because these are often new and poorly understood, they can be especially risky.
- Co-occurring disorders (dual diagnosis): Involves the simultaneous presence of a substance use disorder and another mental health condition like depression, anxiety, or bipolar disorder. This complicates treatment and requires an integrated approach.
- Behavioral addictions: While not always classified as substance use disorders, behavioral addictions like gambling, food, or internet addiction often share similar neural pathways and can co-occur with SUDs.
- Other (or unknown) substance use disorder: The DSM-5 also allows diagnosing SUDs related to unknown or unspecified substances, which may not fall into existing categories but still cause significant impairment or distress.
These various types of SUDs require tailored treatment approaches, considering their unique challenges and health risks. Knowing the specific type can make all the difference in finding the most effective route to recovery.
Risk Factors and Causes of Substance Use Disorders
Some people are more susceptible to SUD than others. Genetics can play a role. Specific gene mutations may make some people more prone to addictive behaviors. However, genetics is just one piece of the puzzle, often interacting with environmental and psychological factors contributing to SUD.
Understanding the risk factors and causes of substance use disorders can be empowering.
Environmental Factors
- Family environment: Growing up in a household where substance use is normalized can increase the risk of developing SUD.
- Peer pressure and social networks: Being surrounded by friends or social circles that engage in substance use can influence behavior.
- Accessibility: Easy access to substances, whether through prescription medications at home or drugs sold on the street, plays a significant role.
- Socioeconomic status: Financial stress and lower socioeconomic conditions can make people more susceptible to SUD as a coping mechanism.
- Cultural influences: Social attitudes and cultural beliefs about substance use can also be determining factors.
Genetic Factors
- Family history: Genetics can predispose people to addictive behaviors. A family history of SUD raises the risk factor.
- Biological makeup: How an individual’s body metabolizes a substance can influence the likelihood of dependence.
- Genetic mutations: Specific gene mutations may make some people more susceptible to SUDs.
- Age of first use: Genetic factors can interact with environmental factors like age at first use to influence the risk of developing SUD.
Psychological Factors
- Mental health conditions: Conditions like depression, anxiety, and PTSD are often co-occurring disorders with SUD.
- Stress and coping mechanisms: The inability to cope with stress in healthy ways can lead to substance use as a form of self-medication.
- Personality traits: Traits like impulsivity or high sensation-seeking can make an individual more prone to experimenting with substances, thus increasing the risk of SUD.
- Trauma: Past or ongoing traumatic experiences can contribute to the use of substances as a coping strategy.
Recognizing that these risk factors do not exist in isolation is essential. They interact in complex ways, often amplifying each other. For instance, someone with a genetic predisposition may be more vulnerable if they’re also in a high-stress environment.
Understanding these various risk factors is not about laying blame. It’s about gaining insights that can inform prevention and treatment efforts.
Consequences of Substance Use Disorders
Life with a substance use disorder can feel isolating and overwhelming. However, understanding the full scope of its impact is a step toward reclaiming your life or aiding someone you love.
Health Risks
- Physical deterioration: Long-term substance use can lead to various health issues, including liver damage, respiratory problems, cardiovascular disease, stroke, and multiple forms of cancer.
- Overdose risk: Many substances, especially opioids and certain prescription medications, carry a high risk of overdose, which can be fatal.
- Immune system: Chronic use can weaken the immune system, making one more susceptible to infections.
- Nutritional and metabolic imbalance: Substance use can interfere with nutrient absorption and metabolism, leading to malnutrition and weight loss.
- Cognitive decline: Long-term use of certain substances can result in memory loss, concentration problems, and diminished cognitive abilities.
Socioeconomic Implications
- Employment: SUD often impacts job performance and career prospects, leading to unemployment and financial instability.
- Legal consequences: Substance use can result in legal issues, ranging from DUIs to more severe criminal charges, leading to incarceration.
- Family dynamics: SUD can strain family relationships, potentially resulting in separation or divorce and impacting the emotional well-being of children.
- Homelessness: In extreme cases, substance use disorders can contribute to homelessness.
Emotional and Psychological Damage
- Mental health: Substance use often co-occurs with mental health disorders like depression, anxiety, and PTSD, either as a cause or an exacerbating factor.
- Self-esteem and identity: Chronic substance use can erode self-esteem and contribute to a sense of lost identity, making recovery more challenging.
- Social isolation: As the disorder progresses, people may withdraw from social activities and relationships, leading to feelings of isolation and loneliness.
- Emotional numbness: Substance use can serve as a way to numb emotional pain, but it also suppresses the ability to feel pleasure, leading to an emotional flatline over time.
While this might seem like a grim list, understanding the whole picture is crucial for the next steps toward recovery. The consequences of SUD are interconnected, forming a tapestry that impacts nearly every aspect of life.
Getty image by LeszekCzerwonka