5 Mental Health Takeaways From a Psychologist Who Specializes in IBD Patients
I had the pleasure of sitting down with inflammatory bowel disease (IBD) experts and patient advocates in honor of World IBD Day to discuss a topic I am most passionate about — the integration of a mind and body approach into IBD care. While there is much to be grateful for with respect to medical advances in the management of IBD over the last decade, with respect to medical advances in the management of IBD over the last decade, the prevalence of comorbid mental health disorders has remained high and stagnant — suggesting that simply screening our IBD patients for anxiety and depression is insufficient and usually too late. We must empower patients and providers to have an open dialogue about the unpleasant aspects of day-to-day management of IBD, remembering that the majority of disease care takes place outside of the doctor’s office!
The goal of IBD therapy and monitoring is to prevent bowel wall damage, avoid surgery and minimize complications. We must think similarly about mental health — a proactive approach that targets and monitors the emotional aspects of living with a chronic condition, with the parallel goal of preventing the onset of mental health disorders and associated disability. I am confident we as a community can do this by building resilience and reducing stigma.
Below are some key takeaways from my conversation with The Mighty. To watch the entire conversation, head here.
1. Mental health and IBD are deeply entangled.
I go so far as to think of anxiety and depression as extra-intestinal manifestations of Crohn’s and colitis, particularly because we have so much data on inflammation and depression, the microbiome and mental health, and of course, the brain and the gut. There’s just no reason to separate mental and physical health when it comes to IBD.
Depression and anxiety are psychological disorders, but there’s a range of symptoms of those disorders that patients have well before they become clinically diagnosed with depression or anxiety — and they may never. Not being able to talk about your mood or your fatigue or your difficulty making decisions, your fear of not finding a bathroom in time… those are all precursors to the onset of depression and anxiety. When we don’t ask about those things, that’s when the disease becomes more and more disabling.
2. Symptoms of anxiety and depression are common in patients living with IBD.
Recently, a large meta-analysis from the U.K., found that the prevalence of depression in IBD patients was just about 25% — so one in four people actually met criteria for depression according to a self-report questionnaire. One in three, so 30%, met criteria for anxiety using that same sort of rigorous approach to self-report.
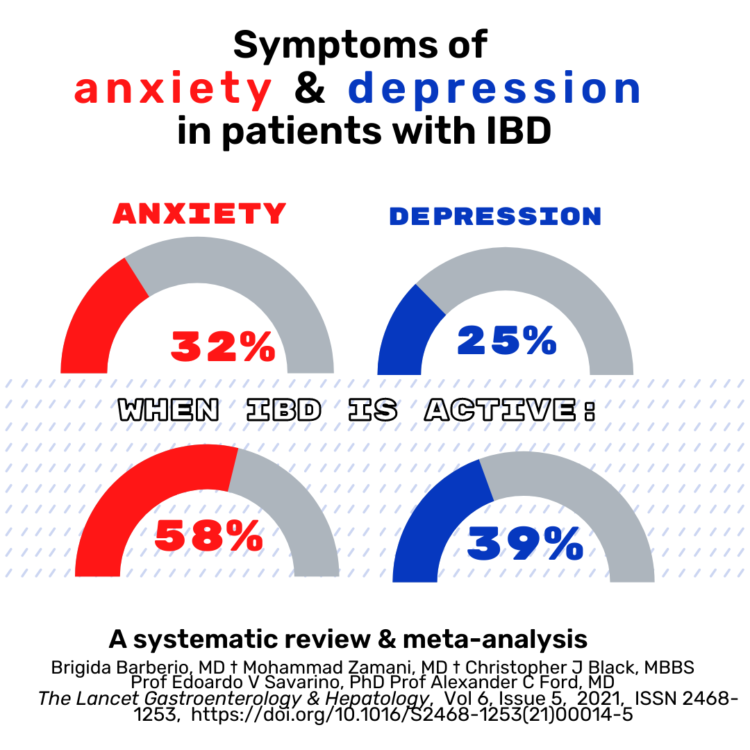
When you look at the data during disease flares, anxiety skyrocketed. And that makes sense, who’s not anxious when their disease is active? The rates of depression also rise when the disease is active. So again, we can’t disentangle this brain-gut connection because the inflammation and the psychological symptoms overlap and co-occur and really can’t be separated.
3. Policymakers need to see comorbidities as a societal issue to solve.
It’s also a healthcare cost problem. IBD patients who have comorbid depression or anxiety actually cost the health system five times more than an IBD patient who does not have that comorbidity. This is an urgent issue, if payers and policymakers could really hear this — that not integrating mental health into IBD care is not just a problem for the individual patient, it’s a societal problem.
4. It’s on both the doctor and patient to make sure mental health is addressed.
I so believe that physicians need to be asking about mental health — that needs to be just part of our practice culture. Obviously, some of it starts with getting the physicians to always have that door open to bring it up.
There’s a lot of catastrophizing that happens on both the patient’s and the provider’s side around these conversations. The patients often are afraid to ask because they don’t want to be perceived as a burden to their doctor; they’re afraid of making their doctor uncomfortable. I think on the flip side doctors are often afraid they’re going to get in over their head, you hear about “opening Pandora’s box,” or there are just system barriers to the amount of time you have to discuss these things.
5. Setting up an additional appointment with your gastroenterologist can be a gamechanger.
I often tell patients if you really want to bring up an issue and you’re worried about burdening your doctor (or surprising your doctor, because that tends to be the biggest concern), set up an extra visit to talk specifically about your fatigue, your urgency, your incontinence, your fertility concerns… there’s a lot you can do to advocate for yourself in those conversations so that you feel empowered to talk about it.
What’s been most helpful in managing your mental and/or physical health?
Answer here. You can also join our private Women+ With IBD group to make your own post, meet others going through similar journeys, or simply check it out!
Getty image by Yukari Mishima.

