What You Should Know Before You Stop Taking Antidepressants
Editor's Note
Please see a doctor before starting or stopping a medication.
In the antidepressant world, you may not be told — not even by your psychiatrist — about medication side effects, how long you’ll have to take antidepressants, what they are supposed to do or how they work. But if there’s one warning about psychiatric drug use we have probably all heard, it’s, “Don’t stop taking your medication without first talking to your doctor.”
Warnings like this might make you feel as though you shouldn’t question your medications or the need to take them. Or it brings up fear that stopping your antidepressants will have cataclysmic ramifications you’ll never come back from. Even if you’ve been feeling great for months or years after an episode of mental illness, doctors rarely suggest you should stop taking them. It’s not surprising about 22 percent of patients don’t consult with their doctors before stopping medication.
But why? And what happens if you do want to stop taking your antidepressants?
What We Know About Antidepressants
First, a little background. In the 1950s, mental illness was treated with two classes of medications — monoamine oxidase inhibitors (MAOIs) and tricyclic antidepressants (TCAs). By 1987, the first selective serotonin reuptake inhibitor (SSRI), fluoxetine (brand name Prozac), was approved. A second generation of antidepressants called serotonin-norepinephrine reuptake inhibitors (SNRI) came along in the 2000s. SSRIs remain the most popular class of antidepressants.
Though it’s still a bit of a mystery how antidepressants work, the current consensus is they increase the amount of “feel good” neurotransmitters in your brain like serotonin, dopamine or norepinephrine. SSRIs, for example, block the brain’s ability to reabsorb (reuptake) serotonin. This leaves more of the “happy” chemicals between neurons, which, over time, are thought to make you feel better. Most antidepressants take up to four weeks to kick in.
Reasons You Might Want to Stop Your Meds
If you’re one of nearly 13 percent of the U.S. population over age 12 taking antidepressants, there are many reasons you may want to stop. Perhaps they were meant to be a short-term solution and you don’t want to be on them for the rest of your life. Maybe you want to try maintaining your mental health with lifestyle changes like diet and exercise instead. If you’re prescribed several meds, they add up financially month after month. Even if you have insurance, drugs aren’t always affordable.
Antidepressants are also notorious for mild to major side effects. One recent study that asked why people wanted to quit their meds found 74 percent were concerned about long-term risks or side effects. From weight gain or loss to nausea, constipation, fatigue, insomnia, anxiety, risk of seizures and increased risk for suicidal thoughts, side effects can be serious and debilitating. A constant stream of new (and sometimes conflicting) studies warn of other potential health risks.
“I realize antidepressants work for a lot of people and they are a great tool in giving someone a slight helping hand,” Mighty contributor Ben Smallwood wrote in his piece, “Taking Antidepressants Made My Depression Worse.” “But in my case, it was a massive push towards a very dark path.”
Antidepressants also have a black box warning because they may increase the risk of suicide, especially in young adults. As mood improves with medication, those with suicidal thoughts be at higher risk of attempting suicide because they have more energy to make an attempt.
One review of the issue concluded it’s safe to prescribe antidepressants when patients are closely monitored, especially early in the course of drug treatment. Another expert argued the danger of these medications, saying that significantly more suicides are related to antidepressant use than the FDA reports. If you’re experiencing suicidal thoughts, reach out to your doctor immediately, call or text the National Suicide Prevention Lifeline or call 911.

Long-Term Psychiatric Drug Use
You might also consider quitting antidepressants because of concerns about long-term use. Given how little data is available, some claim meds can damage the body’s nervous system if taken too long. But this doesn’t hold up with experts. “In the central nervous system there are 80 billion neurons and about a trillion synapses,” psychiatrist John J. Miller, MD, told The Mighty. “There’s several hundred neurotransmitters and lots of different circuits, so I don’t know what that means. It’s just a vague, general statement.”
Stuart Seidman, MD, a psychiatrist at West End Medical Associates in New York, told The Mighty long-term nervous system damage doesn’t seem to be an issue. He said this kind of serious damage “could only be true if the effect were rare or if it took decades to develop; otherwise, we’d know.”
“I’ve had patients on [Zoloft] for 27 years, who, before they were on it, had severe obsessive-compulsive disorder or a severe episode of depression and couldn’t function,” Miller, who has 30 years of clinical experience, added. “We tried to take them off it several times and they’d get worse so they’d go back on it. I have not seen any of them have irreversible long-term side effects.”
Other classes of mental health drugs, like antipsychotics or lithium, do have potential long-term consequences. Antipsychotics can result in a movement disorder called tardive dyskinesia, while lithium can reduce the function of the thyroid gland or cause kidney disease. Miller said close monitoring can catch these symptoms early to prevent further harm. If you feel uncomfortable with the medication you are taking, ask your doctor to explain the potential long- and short-term side effects so you can make an informed decision about your treatment.
There’s also concern that antidepressants are addictive. Addiction means you develop a tolerance to a substance and need higher and higher doses to get the same result. Research indicates this is not the case with antidepressants. A drug may eventually stop working and require a dose increase or medication change, but that’s not because you’re addicted. It’s just a feature of some antidepressant drugs. Other classes of mental health meds — benzodiazepines like the anti-anxiety medication Alprazolam (brand name Xanax), for example — can be addicting.

4 Things You Should Know Before Stopping Your Medication
Psychiatric medications work differently for everyone because of our unique biological makeup and individual environmental triggers. Which drugs work for you may be useless to someone else. You may have side effects and your best friend on the same medication may not. Accordingly, whether or not to stop taking antidepressants is a decision that only you — with input from a doctor you trust — can make.
1. There’s a Risk of Mental Illness Relapse
One major risk of stopping your medications is a risk of relapse. Some doctors consider the danger of a mental health relapse a greater concern over any hypothetical negative impacts of using antidepressants for years. Mental illnesses like depression or bipolar disorder are prone to recur. Medication may be the best option to prevent future episodes and maintain a higher quality of life.
“Once a person has a second episode, that person will almost always have recurrent episodes,” Seidman told The Mighty. In the case of a condition like bipolar disorder, a manic episode that’s left untreated may turn into a psychotic break. Those with untreated depression or bipolar disorder have a higher risk of suicide.
“It’s a generalization but it really holds true for all the major mental illnesses like schizophrenia, recurrent unipolar major depression [and] bipolar depression,” Miller told The Mighty. “[The] more episodes a person has over the course of their life and the longer they go untreated, the greater the risk they have for future episodes and the harder those future episodes will be to treat.”
2. You May Experience Withdrawal Symptoms
When you stop taking your medication, you may experience withdrawal, or discontinuation, symptoms. These could include “flu-like symptoms, insomnia, nausea, imbalance, sensory disturbances, and hyperarousal,” said Johnny Williamson, MD, a psychiatrist and medical director at Timberline Knolls in Illinois.
You may also experience “headaches, dizziness, fatigue, electric shock type symptoms (sometimes referred to as zingers) and irritability.” Usually, any withdrawal symptoms start within a few days of lowering the dose of your antidepressants and last one to two weeks. Most symptoms are mild, though that’s not always the case.

It’s also important to know that discontinuation symptoms can look like a relapse of your mental illness. However, these warning signs could be the direct result of medication leaving your system. It’s important to keep an eye on this and check in with your doctor. Mighty contributor Emma Wilson experienced similar symptoms when she stopped her meds, in addition to physical ones, which she wrote about in her piece, “The Part of Taking Antidepressants Doctors Can’t Prepare You For“:
For me, the symptoms of withdrawal vary greatly and seem to fluctuate within a fairly quick time period. From nausea and digestive problems, to headaches, dizziness, sore feet, ulcers and teeth grinding in my sleep, the physical symptoms can feel quite bizarre. The mental blips are arguably the hardest, particularly panic, sudden low mood or anxiety attacks. Sometimes it can feel like I’m going loopy and slightly mad (oh, the irony).
3. You Should Do It With the Support of a Medical Professional
Before stopping psychotropic medications, talk to your doctor first. You’ll want to discuss your reasons for discontinuing medication, how the process might work and the potential effects of withdrawal. A doctor — or even a pharmacist — can help decide how fast (or slow) you should go while lowering doses to minimize any potentially dangerous consequences, including side effects or interactions with other drugs you’re taking.
Be aware that not every doctor will be helpful. A 2017 study of 250 U.S. patients who attempted to stop taking up to two psychiatric drugs found that only 45 percent of participants thought their doctor was helpful at the time. Psychiatrists aren’t always great about explaining what medications they’re giving you and why in the first place. If your doctor isn’t willing to work with you, you have every right to find a new one.
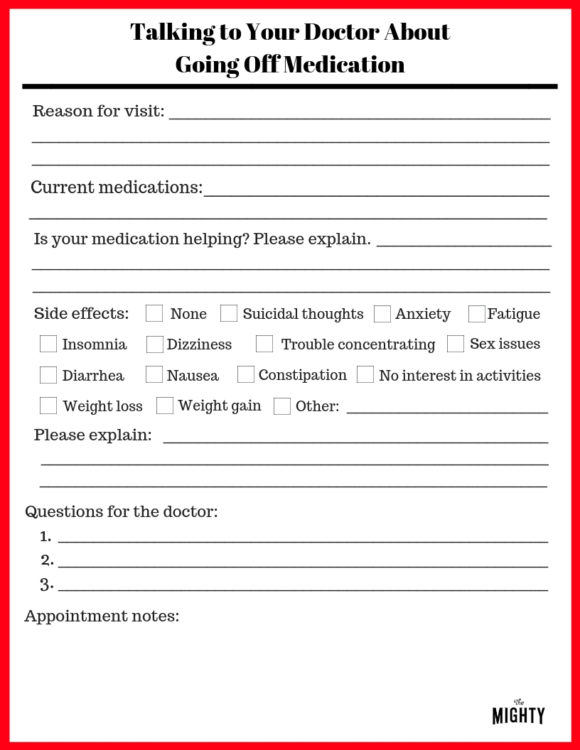 (Click here to download a PDF version of the form and here to download a PDF you can complete digitally.)
(Click here to download a PDF version of the form and here to download a PDF you can complete digitally.)
Come to your appointment prepared and be specific. If your doctor asks if a medication is helping, instead of responding with, “Maybe a little,” try giving examples. “I only missed two days of work because of depression this month instead of five.” Do your own research and be assertive to get your questions answered. “The more informed my patient is, the easier my job is,” Miller told The Mighty. “There are always risks to the benefits [of medication] and that’s why it should be an ongoing collaboration between the patient and the prescriber.”
4. You Need to Go Slowly and Taper Off
Clinicians usually suggest waiting at least six months to a year after your mental illness symptoms have subsided before considering quitting your meds. From there, you’ll work with your doctor to create a plan to taper your medications slowly over time, which could mean weeks, months or even a year or more. Slow tapering has two major benefits. First, it reduces the discontinuation symptoms you’re likely to experience.
“Some medicines, the longer you’re on them and the higher the dose, the slower you have to taper off them to minimize withdrawal symptoms,” Miller told The Mighty. “Some of the withdrawal effects are not dangerous but they’re very, very scary. Other withdrawal effects can be really dangerous. If someone’s on say Klonopin for a year at 4 mg and they stopped it cold turkey, two weeks later they could have a seizure while they’re driving.”
A gradual taper schedule also reduces the risk of a mental health relapse. A Harvard Medical School study found that out of 400 participants, those who stopped their antidepressants in seven days or less were more likely to experience a mood or anxiety disorder relapse within the following year. Miller advised you’ll want to “make changes slowly so that your brain will hardly notice.”
How to Create a Taper Schedule
A major consideration of a successful taper schedule is how long an antidepressant stays in your body. This is determined by a drug’s half-life, the amount of time it takes for half the medication to leave your body. For example, the half-life of sertraline (brand name Zoloft) is approximately 26 hours. After that amount of time, half the drug will be out of your system. In another 26 hours, another half will be out, and in just over five days — after five half-lives —sertraline will be almost completely out of your system.
The longer the half-life of a medication the fewer discontinuation symptoms most people experience. For medications with a shorter half-life, it can take longer to get off them safely even at lower doses. Your doctor should take this into consideration. Everybody responds to withdrawal differently, and your doctor can adjust your taper accordingly. Write out a tapering schedule with your psychiatrist that reduces your medication dosage by a small amount every two to six weeks, or longer depending on what’s best for you. Keep a copy of the schedule handy so you can easily track your progress.
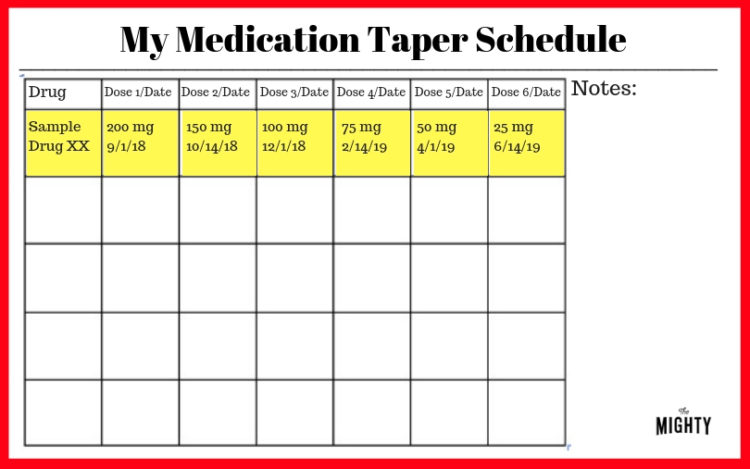 (Click here to download a PDF version of the form and here to download a PDF you can complete digitally.)
(Click here to download a PDF version of the form and here to download a PDF you can complete digitally.)
Some clinicians might try prescribing a medication with a longer half-life, like fluoxetine (brand name Prozac), as a stop gap to minimize uncomfortable symptoms. A liquid-based drug formulation may also be an option, especially for tiny doses. Your doctor should prescribe the appropriate pill size or drug formulation for each dose reduction. Also, confirm that it’s OK to cut antidepressant pills as needed.
What to Do If You Take More Than One Medication
Stopping one or more medications when you’re on several is tricker. Each medication has a different metabolism speed in the body. When one medication dose changes, that may affect the others you’re taking, even if they are for another condition such as a chronic illness. Williamson explained it like this: “If you reduce drug A that increases the metabolism of drug B, the amount of drug B available in the blood may increase.” Or, as one medication changes, another may decrease and no longer be effective.
Coordinate with all your doctors if you were prescribed other medications from someone other than your psychiatrist to monitor drug interactions. Be mindful of substances like alcohol, tobacco, marijuana and other drugs, which can have a big impact on the effectiveness of your prescriptions meds. The same goes for any natural supplements. Be upfront with your doctor so that you can work together to minimize your risk. You may be able to taper off multiple drugs at the same time, depending on which medication you take and your doctor. Miller, for example, likes to reduce medications one at a time.
“I will review each of the medicines they’re on, the role they’re playing, the side effects from the drug, the possible withdrawal effects and then once we decide on which drug makes sense as the first to pull away, create a plan to do it moderately,” Miller said. “The patient should make that choice based on the purposes of each of the drugs and what they can expect as those drugs get pulled away.”
Often times those in treatment for mental illness end up taking four or more medications to manage their symptoms. In general, this isn’t ideal, and it’s a good idea to ask your doctor if you can simplify your prescriptions. “I inherit patients that come in from other places and they might be on six or seven drugs,” Miller said. “The first goal is let’s try and get you down to four over the next year and then see where you’re at and then let’s try to simplify it more….As a psychiatrist, my goal is the lowest dose and fewer medications.”
How to Reduce Withdrawal Symptoms
In addition to working with your doctor on a taper schedule, you can take control of the process by adding additional supports. To help naturally boost your brain health while stopping an antidepressant, get regular exercise, follow a consistent sleep schedule and eat a nutritious diet.
Studies have shown that working with a counselor during the antidepressant discontinuation process leads to a better outcome. A therapist can help you monitor mental health fluctuations, support positive lifestyle changes, work on skills to prevent relapse and address any underlying causes of mental illness such as trauma. Friends or family can also be on the lookout for health or mood changes that may signal an issue and support you through the process.
After You’re Off Your Meds
Once you’ve completed your taper schedule, schedule a follow-up appointment with your doctor about a month later. You’ll have an opportunity to check in, talk about any lingering symptoms you’re still experiencing and lay out a plan if you run into any issues in the future.
Continue to monitor your mood and any behavioral changes that might signify a mental health relapse and require a visit to the doctor. Finding a creative way to track your mental health can make this fun. You can also enlist a loved one (and your therapist) to nudge you if they notice something might be off.
Alternatives to Stopping Medication
You may have tried to stop taking antidepressants and found it wasn’t the right decision. There is absolutely nothing wrong with that, and many people do really well on medications long-term. Any decision that keeps you healthy is a good one.
And this is why I use #medication as part of the plan to address my #anxiety and #mentalhealth. Antidepressants, for me, are the metaphorical oil on the railroad switch. I still have to steer the train, but they make it easier to apply the training I give myself in therapy.
— Sarah Curtis-Tilton (@sarahbearct) September 7, 2018
If you’re still unhappy with your antidepressants, several other alternatives might be worth trying. Reducing the dose of meds you’re on or switching to a different medication might clear up unwanted side effects, for instance. Every person’s chemistry is unique, so what works for you may not work for someone else. Talk to your doctor about options to address your concerns about antidepressants.
Staying Mentally Healthy
You may decide to take care of your mental health with long-term psychotropic drug maintenance, reducing medication dosages or the number of drugs you’re taking, changing meds or successfully quitting antidepressant use altogether. No matter what route you choose, even if it’s stopping your meds altogether, the goal is the same — mental health
“Upon successful discontinuation of antidepressant medications, it is expected that people return to their pre-depressive state of functioning,” Williamson told The Mighty. “Ideally, there are no remnant discontinuation symptoms, mood and anxiety are stable, and the person feels that they function free of such symptoms.”
Header Getty Image via Alina Traut.

