Monkeypox Myth Busting: Here's What You Need to Know
Editor's Note
The following article contains details about Monkeypox that may be triggering.
This interview took place on August 4, 2022. As scientists are still learning about this virus, this information could have shifted and changed. Please do your due diligence when it comes to information about any viral disease.
On August 5, 2022, the United States government declared monkeypox a public health emergency.
As someone who (sadly) lives on the internet, ever since monkeypox was announced I’ve been seeing different peoples’ thoughts, opinions, and fears when it comes to this disease. Generally speaking, there’s been a lot of good information and threads on the virus; however, there’s also been a lot of fear-based misinformation that, even if well-intentioned, can ultimately cause more harm than good.
It’s for this reason that I connected with Emma Crowley. Emma is a public health professional and rare disease advocate with over a decade of paired experience and advocacy. In addition to public health, Emma has previously worked in human genetics, clinical trials, and global health. Her broad experience has allowed her to speak to physician groups, pharmaceutical companies, and the Food and Drug Administration. She is skilled at breaking down complicated scientific concepts into accessible content.
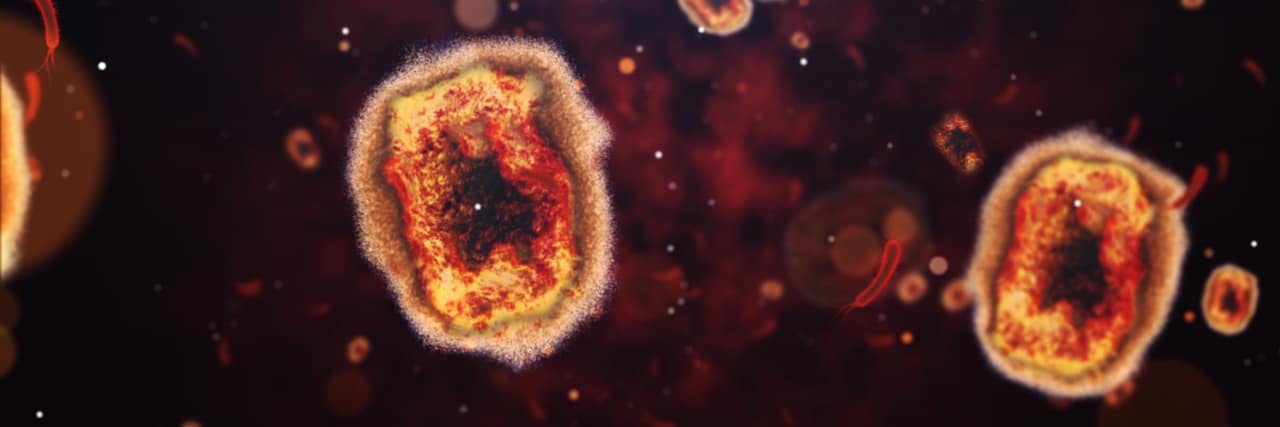
What is Monkeypox?
Emma: Monkeypox is a pustule virus that is related to smallpox and to chickenpox, and what they have in common is those little bumps all over your skin.
Is it new or has it been around?
Emma: Before this outbreak, there were two different clades [of this virus]. One that was found in the Congo is called the Congo Basin clade, and then the other one is called the West African clade.
Traditionally the one found in the Congo was more transmissible and more deadly. The West African one was less transmissible and less deadly. At this point, we believe the virus we’re seeing now is genetically different than those two, but we believe it’s come from or has mutated from the West African one. It’s existed in those regions since the 1970s, and we know that it transmits from animals to humans. It lives in monkeys, of course, but also in rodents, squirrels, moles, and things like that. It’s remained quiet for decades, but in the past 10-15 years there has been some growth.
What are some dangerous misconceptions about monkeypox, outside of it being an LGBTQIA+ predominant STI?
Emma: When it comes to it possibly being a sexually transmitted infection (STI), it can be spread by sexual contact, but it doesn’t mean it’s exclusively an STI. It can live on surfaces, which is called a fomite, but touching a table or trying on clothes at a store likely won’t give it to you. You do need likely close contact — sharing bed linens or cups, but obviously, you’re close with that individual. Sex can be part of that transmission, but it’s not exclusive.
Scientists are still looking into if there is a bodily fluid transfer that makes it more transmissible in the men who have sex with men, or MSM, community. But it does seem unusual that a majority of cases have been men who have sex with men when according to statistics, we should be seeing more women and children exposed. It could be because of superspreader events, Or, ever since the HIV/AIDS epidemic, the MSM community has really developed close ties to their local health departments and have really close health relationships with people that they have sex with. So it could just be that they were the ones who brought it to our attention first.
“… The isolation period is long: about three to four weeks. You are contagious until your lesions drop; they kinda scab over and drop and are replaced with new skin. You are contagious until that new skin has formed.
Are people already protected against contracting it in regards to prior smallpox vaccinations?
Because it’s in the pox virus family, the smallpox vaccine is protective. I do believe that the CDC is still recommending people who are high risk in the gay community, in the MSM community to get a vaccine anyway, but it’s very interesting when you look at the data because you can see that as smallpox vaccines decline — which, in the United States, we stopped vaccinating for smallpox in 1973 and we declared officially eradicated from the world in 1980 — monkeypox has increased because there’s an unvaccinated population. This has allowed the virus to spread.
Also, the mortality rate for the African clades is about 1-10%, but we’re seeing very few deaths for how many cases there are. It’s not always presenting the same way as those pustules. People are also getting rashes, or they may look like a bunch of little pimples and bumps instead of the traditional pox that you think of. It’s also making it difficult for doctors to feel comfortable with diagnosing, so the word from the CDC is if you see something just test it, which is probably the right thing to do at this point.
What are the best preventative measures when it comes to Monkeypox, or what can we do to ease our anxiety when it comes to the disease?
It’s kind of unfortunate, but it’s really important for at-risk communities to decrease their sexual partners. This isn’t just for transmission, but it also buys time for public health officials to vaccinate as many people as possible.
The vaccines that people are using are called Jynneos. It comes from a company called Bavarian Nordic and they produce it in Copenhagen, and it was really only approved for people with the monkeypox virus, or if you were on assignment for a specific job in an African nation that sees it more often. Part of the difficulty is that we’ve never needed this many, but what’s important is that it’s safe for individuals who are HIV positive. So it doesn’t pose a big risk, there are very few side effects, and it’s a great safe vaccine. You do need two doses, and if you are exposed, it is recommended that you get vaccinated within four days. If you do, you may be able to stop the onset of illness, and if you stop the onset, you stop the transmission.
There is still some research going on to see if you can spread [the virus] asymptomatically, but that’s still being researched.
The ACAM2000 was left over from our old-school smallpox vaccine. It was developed for smallpox and we just happened to have a bunch on hand in case there was biological terrorism, but the rate of people having adverse reactions was relatively high, like a couple per thousand, and it’s a live virus that has the ability to replicate, whereas Jynneos does not. So you’re exposing yourself to a tiny amount of the live virus, which for those who are immunocompromised (such as those who are HIV positive) isn’t safe.
Hopefully, that’ll just be a backup. It looks like the federal government is working to procure as many doses as possible and will be implementing the Defense Production Act to engage other pharmaceutical companies to support them in their production, so hopefully, we get ahead of it but it’s unfortunate how widespread it got so quickly.
There have been some people reporting that their doctors don’t know what to do once they’ve contracted the disease. Do you have any advice on what to do or where to go if you suspect you’ve contracted monkeypox?
Doctors are still learning about this. We’re all learning in real-time, but I would recommend people contact their local health departments. We can make sure to get you in contact with the resources that you need and ensure that you have some funding so you can stay home and isolate, yourself because the isolation period is long: about three to four weeks. You are contagious until your lesions drop; they kinda scab over and drop and are replaced with new skin. You are contagious until that new skin has formed.
It’s important that we stay properly informed about Monkeypox so we know how to both protect ourselves and our community. Make sure you stay up to date with the latest news from the CDC as they help advise the country through this public health crisis. You’re not alone, and together we’re going to get through this.
Getty image by kontekbrothers