What Treatments Work for Parkinson's Disease?
Editor's Note
The Mighty’s Condition Guides combine the expertise of both the medical and patient community to help you and your loved ones on your health journeys. For this guide, we interviewed seven medical experts, read numerous studies and surveyed nearly 400 people living with Parkinson’s. The guides are living documents and will be updated with new information as it becomes available.
Other sections of this Condition Guide:
Overview | Symptoms | Diagnosis | Resources
What you’ll find in this section:
Medications | Levodopa Side Effects: Dyskinesia | Other Dopamine Replacement Drugs | Other Drugs Used for Parkinson’s Disease | Using Non-Parkinson’s Drugs to Treat Symptoms | “On” and “Off” Periods | Surgery: Deep Brain Stimulation | Exercise | Other Therapies | Community Recommendations
This section was medically reviewed by Brent Bluett, M.D.
What Treatments Work for Parkinson’s Disease?
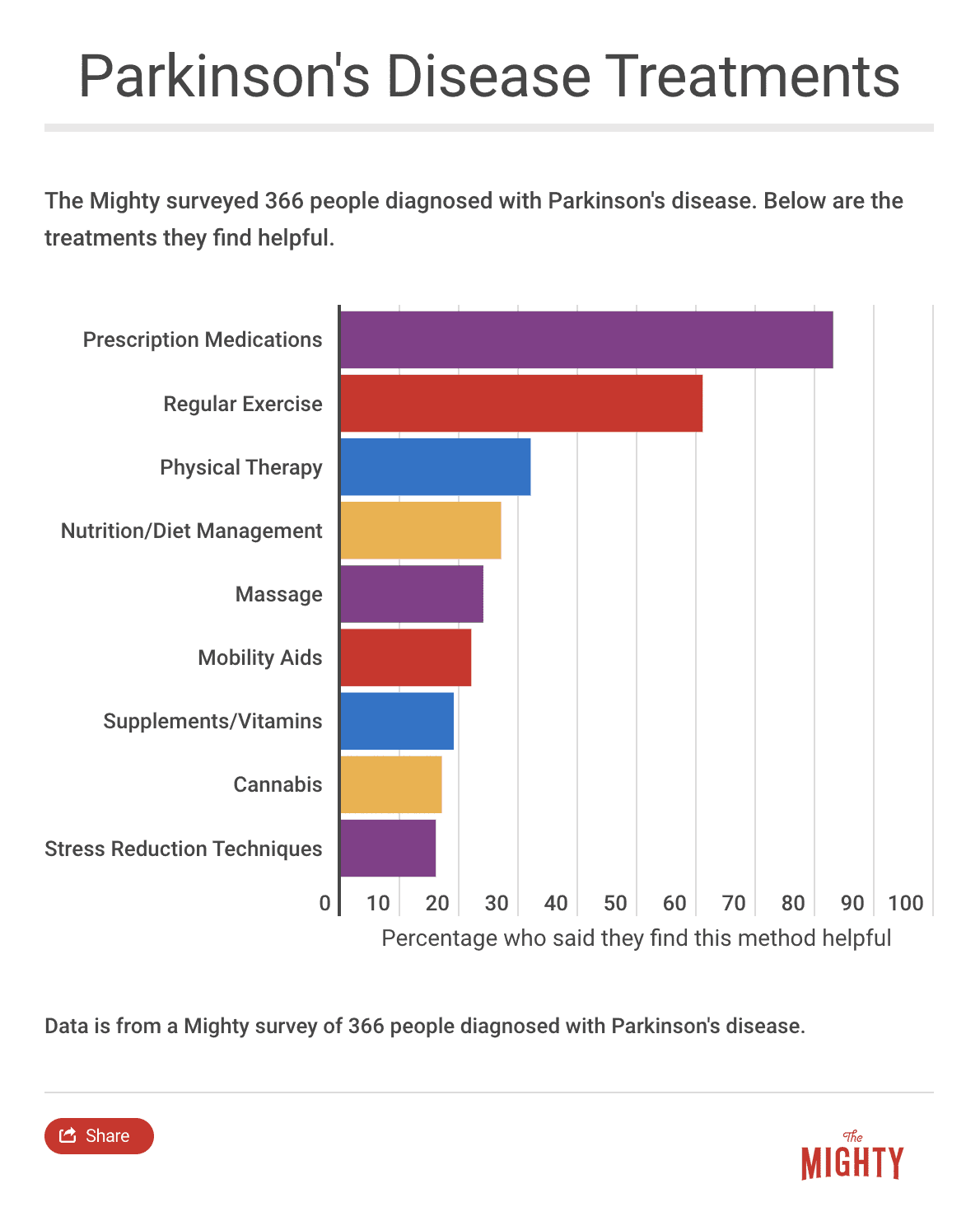
It can be scary to get a diagnosis of Parkinson’s disease, but what many people don’t realize is there are many treatment options, including medications, therapies, surgery and lifestyle changes that can help lessen the impact of your symptoms. There is no one-size-fits-all treatment, and not everyone experiences improvements from treatments. That being said, there are three treatments generally accepted to be the most effective: medication, deep brain stimulation surgery and exercise.
What is Parkinson’s Disease?
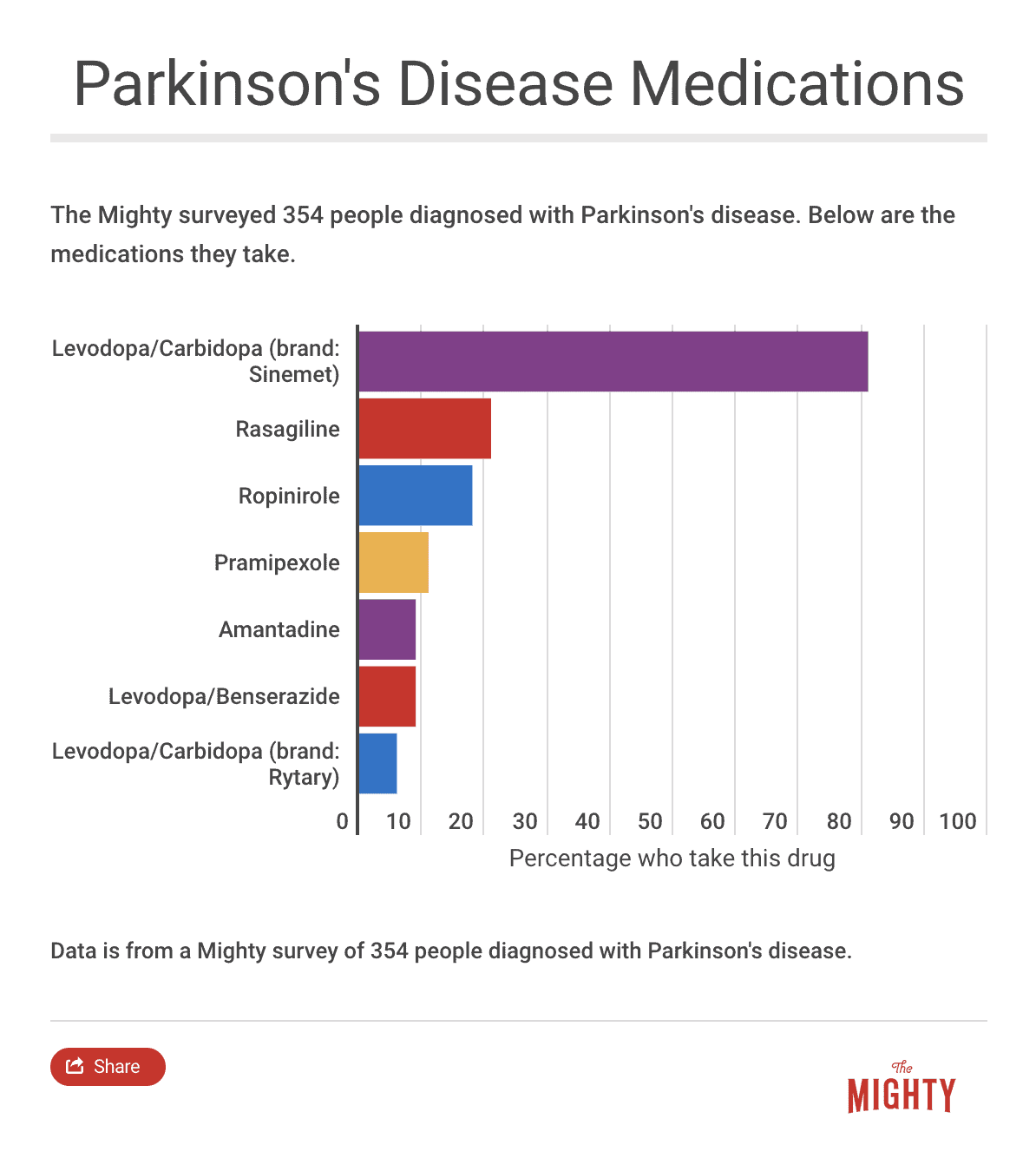
Medication
Your doctor will talk to you about several different medication options, though a few are generally considered more effective than others. It’s important to remember that most Parkinson’s medications only really target movement symptoms, which can be frustrating if you are struggling with non-movement symptoms like fatigue and brain fog. However, when it comes to movement symptoms such as slowness, stiffness, tremor, and difficulty walking, Parkinson’s medications can greatly improve your quality of life.
Levodopa
Levodopa (also called L-DOPA) has been the gold standard treatment for the motor symptoms of Parkinson’s disease since 1967 when a landmark study revealed that gradually increasing the dosage of levodopa given to patients led to dramatic improvements in motor symptoms.28
Levodopa is a drug that is converted to dopamine in the brain, which makes it the closest thing people with Parkinson’s can get to the “real stuff.”13 This means when it’s working, levodopa improves symptoms like rigidity or stiffness, slowness of movement and tremor, though it does not slow down the progression of the disease.
One of the challenges of levodopa is that it is a short-lasting medication because it gets converted into dopamine quickly.1 This means it usually needs to be taken several times per day to maintain its effect. Also, just as levodopa is converted to dopamine in the brain, it is also converted to dopamine in the rest of the body, which can cause its most common side effect, nausea. Levodopa is frequently paired with carbidopa, a drug that prevents levodopa from being converted to dopamine outside the brain and also helps prevent nausea. You will likely see your prescription labeled as “carbidopa-levodopa” indicating the pairing of these two drugs.
Carbidopa-levodopa can be taken in several different ways:
Pill/tablet
Pills or tablets come in two formulations: immediate release (the drug works quickly, for a shorter period of time) and extended-release (the pill releases the drug into your system over a longer period of time). As the disease progresses, you may need to take the pills more frequently in order to maintain the medication’s positive effects and keep you “covered” after doses wear off.
Pill and tablet brand names include:
- Sinemet (immediate-release carbidopa-levodopa)
- Sinemet CR (extended-release carbidopa-levodopa)
- Rytary (extended-release carbidopa-levodopa, a formulation designed specifically to provide longer-lasting benefits)
- Parcopa (extended-release carbidopa-levodopa that dissolves on the tongue, ideal for people with trouble swallowing)
- Lodosyn (carbidopa only — you might take this as a way of extending the effectiveness of your other levodopa/carbidopa medication or to reduce nausea, a common side effect of levodopa).
- Madopar/Prolopa (levodopa-benserazide — benserazide provides the same function as carbidopa but it is not approved for use in the U.S. You may see this as Madopar in the U.K. and Prolopa in Canada.)
Note that in July 2019, drug manufacturer Merck announced that Sinemet CR will no longer be available in the United States. If you want to take Sinemet CR, you will have to switch to a generic version.
Infusion
The infusion method of taking your medication provides carbidopa-levodopa in a gel formulation that is infused through a PEG-J tube in your intestine, delivered through a pump continuously over 16 hours a day. This requires surgery to create a small hole, called a stoma, in your stomach. Then, a tube is placed through the hole that connects your intestine to a pouch outside your body, which contains a pump and a “cassette” of a gel formulation of levodopa-carbidopa. This surgery is a common, routine procedure that takes about 30 to 45 minutes, and should require a recovery time of a few days.29
The infusion pump is programmed to release gel continuously from the time you wake up until the time you go to sleep. You will need to change the cassette once or twice a day.15 This procedure is typically used when Parkinson’s disease has progressed, and you require more frequent doses of oral carbidopa-levodopa.36 With an infusion, you get a continuous supply of carbidopa-levodopa delivered directly to your gut, bypassing the difficulties associated with frequently taking pills. The brand name of this formulation is Duopa.
Inhaled Powder
An inhaled powder formulation of levodopa is ingested using an inhaler-like tool. It was designed to be taken as needed when your other medication wears off and you begin to experience an “off” period when your symptoms are worse.20 You might try this formulation if you are having more off periods and want immediate relief when you feel the symptoms come on — it is designed to work within about 30 minutes.18 The brand name is Inbrija.

Levodopa Side Effects: Dyskinesia
One side effect of levodopa is dyskinesia: uncontrolled, involuntary muscle movement. One way to describe dyskinesia is feeling like you’re a puppet being controlled to move at triple speed.9 The movement can range from small twitches to more disruptive flailing and wriggling of your limbs and body parts.
As Parkinson’s progresses and the amount of internal dopamine your body produces decreases, you become more dependent on the levodopa you’re getting from your medication (i.e. levodopa/carbidopa).13 When your body is not producing enough dopamine and the medication has worn off, you may have difficulty moving, “freezing” (this is when you are unable to take a step forward despite having the intention to do so), slowness of movement, and rigidity or stiffness. To treat these symptoms, you may require more doses of levodopa, which can then result in excessive movements, aka dyskinesia.31
To help you experience less dyskinesia, your doctor might tinker with the dosage of levodopa you’re already taking, perhaps advising you to take it less frequently or at a different dose than you were before. You also might be prescribed the medication amantadine (brand names: Symmetrel, Osmolex, Gocovri), which was originally used as an antiviral drug but in recent years has been used to treat dyskinesia in Parkinson’s.25 Amantadine is usually used in addition to carbidopa-levodopa to reduce medication-induced dyskinesia.
Another option to reduce dyskinesia is to take a dopamine-replacement drug besides levodopa, called a dopamine agonist, which is less likely to cause dyskinesia — in fact, this is the main advantage to dopamine agonists and a major reason why they were developed in the first place.25 However, dopamine agonists are generally considered less effective than levodopa and are more likely to cause other side effects including psychosis, the formation of extra and potentially harmful body tissue in your lungs, or an irregular heartbeat.25
On the other hand, you might decide you’re OK with some mild dyskinesia symptoms and opt not to treat it at all. Some people find that the benefits they get from levodopa outweigh the downsides of dyskinesia, and would rather keep their drug regimen the same.25 That’s a decision you can make with your doctor.
Should You Wait to Start Taking Levodopa?
There is a common misconception levodopa is dangerous and you should wait to start taking it as long as possible, it only works for a few years, or it will make your Parkinson’s disease progress faster. However, these concerns are a myth if it is managed appropriately.35
Levodopa has been used since the 1960s and there is no evidence that it is harmful to the brain. In fact, levodopa may have a slight protective effect.25 Medical professionals are more focused on helping your brain stay as normal as possible for as long as possible, rather than under-treating for the theoretical benefit of taking fewer medications. In addition, levodopa can make you more mobile so you can exercise more, which is another important (and effective) treatment strategy.

Other Dopamine Replacement Drugs
Although levodopa is the gold standard and generally accepted to be the most effective treatment for Parkinson’s, there are a few other options. Since we know that long-term levodopa use can lead to the movement issues of dyskinesia, you might want to try another medication first37 (for example, if you are diagnosed with early-onset Parkinson’s, you could take levodopa for a long time). Some dopamine replacement drugs can also help levodopa work better.
Dopamine Agonists
A dopamine agonist drug directly stimulates your dopamine receptors in your brain, similar to how “real” dopamine would. In order to carry out its functions in the body, dopamine must first attach to “receptor” proteins in the brain, which help signal other cells on how to behave. While dopamine agonists don’t turn into dopamine the way levodopa does, they stimulate dopamine receptors without binding to them and ultimately have similar effects in the brain. You can use an agonist instead of levodopa (most frequently recommended for younger patients), or in combination with levodopa. You might also use an agonist if avoiding dyskinesia is a priority for you.
Brand name dopamine agonists include Mirapex (pramipexole), Requip (ropinirole), Neupro (rotigotine — this is a skin patch), and Apokyn (apomorphine — an extremely fast-acting drug delivered through an injection if your other medication wears off suddenly, leaving you immobile).
It’s important to note that agonists can cause serious side effects.6 One side effect is impulse control disorders, such as problems with gambling, obsession with sex or shopping. Other possible side effects include hallucinations and excessive daytime sleepiness. Quitting an agonist suddenly can also bring on withdrawal symptoms.
MAO-B Inhibitors
MAO-B inhibitors disrupt the activity of a molecule that breaks down dopamine in the brain, which allows dopamine to function for a longer period of time.32 You could take an MAO-B inhibitor alone while the disease is mild, or alongside levodopa medication to help it last longer.
Brand name MAO-B inhibitors include Azilect (rasagiline), Eldepryl (selegiline), Zelapar (selegiline) and Xadago (safinamide). Potential side effects include nausea, dry mouth, dizziness, confusion and insomnia. You can’t take the brand name extended release levodopa-carbidopa drug Rytary and a MAO-B inhibitor within two weeks of each other because this can cause high blood pressure.
COM-T Inhibitors
Like MAO-B inhibitors, COM-T inhibitors prevent dopamine from being broken down (COM-T inhibitors just act on a different molecule than MAO-B inhibitors). This allows more levodopa to be available for conversion into dopamine, thereby increasing the amount of time it’s effective.5 Unlike MAO-B inhibitors, COM-T inhibitors can only be used with levodopa, not alone. Since both MAO-B and COM-T inhibitors work similarly, you shouldn’t take them both at the same time.
Brand name COM-T inhibitors include Comtan (entacapone), Stalevo (levodopa/carbidopa and entacapone) and Tasmar (tolcapone). Side effects include orange discoloration of urine, nausea, drowsiness, diarrhea and dyskinesia.
Other Drugs Used for Parkinson’s Disease
While most Parkinson’s medications are based around increasing the amount of dopamine available to your brain, there are a few other medications that work differently. Parkinson’s disease can cause a unique assortment of symptoms, and for this reason, the following medications are used on a case-by-case basis. Depending on your symptoms, your doctor might feel like there is a place for these drugs in your treatment.
Anticholinergics
Anticholinergic drugs are used to treat conditions that involve contraction and relaxation of your muscles. They work by inhibiting acetylcholine, a neurotransmitter in your central nervous system that helps regulate movement.Before levodopa was introduced, anticholinergics were the primary treatment for Parkinson’s disease, but today are used only sparingly, primarily for younger people. It most effectively treats tremor and dystonia — abnormal, involuntary muscle contractions.19 Anticholinergics are typically avoided in older patients because they can worsen cognition. Brand names include Cogentin (benztropine) and Artane (trihexyphenidyl HCL). Possible side effects include nausea, dry mouth, memory problems and vision changes.
Pimavanserin (Brand Name Nuplazid)
One possible symptom of Parkinson’s is hallucinations and delusions, typically occurring later in the disease progression. Pimavanserin (brand name Nuplazid) was developed specifically to reduce the number of hallucinations and delusions you experience. Possible side effects include swelling in your legs and arms, feeling confused, and an increased risk of death if you also have dementia-related psychosis.2
Rivastigmine (Brand Name Exelon)
Rivastigmine (brand name Exelon) was developed to treat dementia caused by Alzheimer’s or Parkinson’s disease. It may also help to reduce the frequency of hallucinations. It works by increasing the amount of acetylcholine in the brain by preventing its breakdown. It comes in a pill, liquid solution and a skin patch. Possible side effects include nausea, tiredness, stomach problems, depression and difficulty sleeping.11
Droxidopa (Brand Name Northera)
One common symptom of Parkinson’s is orthostatic hypotension, which means that your blood pressure drops when you stand up, causing you to feel dizzy, lightheaded or like you’re about to blackout when you stand. Droxidopa (brand name Northera) was developed to treat sudden blood pressure drops after standing due to Parkinson’s. Possible side effects of this drug include high blood pressure while lying down, narrowed or blocked arteries in your heart, irregular heartbeat and headache.26
Using Non-Parkinson’s Drugs to Treat Symptoms
As you may have noticed, most Parkinson’s drugs primarily treat motor symptoms. That means your non-motor symptoms like fatigue, sleep issues and constipation likely won’t be helped by specific Parkinson’s drugs. However, you can still take drugs that aren’t designed specifically for Parkinson’s disease to treat these symptoms. For example, you might try an anti-anxiety medication or a sleep medication to treat insomnia. Your doctor should be familiar with which drugs could interact with other Parkinson’s medications you’re taking, and which ones are safe to use.25<
CBD and Parkinson’s
Now that cannabis is gradually becoming more mainstream (and legal, at least in many places at the state level — click here to find out if cannabis is legal in your state), you may be curious to see if CBD will help treat any of your symptoms. Because medical cannabis as a treatment is so new and still experimental, there isn’t a lot of research about how effective it is for Parkinson’s symptoms. There are currently no federally-approved cannabis treatments for Parkinson’s.
There are a few small studies, however, that researched cannabis and Parkinson’s. One found that CBD (without THC, a part of cannabis that doesn’t cause psychoactive effects) helped decrease symptoms of Parkinson’s-induced psychosis.38 Another small study found that CBD along with THC (the part of the cannabis plant that does cause psychoactive effects) helped decrease pain associated with Parkinson’s, along with tremor and slowness.21 There is also a study that found CBD improves quality of life but not motor symptoms7
Because research is so limited and mixed, you should consult with your doctor before trying any CBD or cannabis products. Cannabis can react with certain medications, so it’s important to exercise caution.

“On” and “Off” Periods With Parkinson’s
As your Parkinson’s progresses over the years, you will probably start to notice even though you’re still taking your carbidopa-levodopa regularly, you experience periods where it’s working effectively (aka “on”) and then periods where the medication seems to not be working (aka “off”). When you’re “on,” you should feel like you can move more normally, with less tremor, stiffness and/or slowness. And then when you’re “off,” all those stiff, rigid, slow movements and your tremor return, almost as if your medications have decided to stop working. Frustratingly, it can be hard to predict exactly how long your “on” and “off” periods will last.
“Off” periods are a result of the disease progressing and becoming harder to control through medication. When you first start medication, it’s common to go through a “honeymoon period” of several years, where it’s working well and you can hardly tell you have Parkinson’s.23 Then, as the condition progresses, your body produces less dopamine, making you more dependent on your dopamine-replacement medication. Over time this leads to more and more instances where the medication is supposed to kick in, or supposed to last for several hours, but is less effective.31
To manage these “off” periods, your doctor will first make sure you are taking your medication as prescribed — it’s important to follow your medication schedule since it can take time for the effects to fully kick in. You can make things worse by changing the times and dosages without a doctor’s approval.25 Then, your doctor can start tinkering with your medication, perhaps having you take your levodopa more frequently, or adding a MAO-B inhibitor, COM-T inhibitor or dopamine agonist to try and smooth out the fluctuations of levodopa in your system.31 However, if you’re trying these strategies and still not able to control or manage your motor symptoms, that’s when it may be time to talk about levodopa-carbidopa intestinal gel (discussed earlier) or deep brain stimulation surgery.
This whole process, from when you start taking medication to when you start considering surgery, can take 10 years or more.31 Another option some experts suggest is to go for surgery earlier in your disease progression, like within the first three to five years, to potentially avoid having to deal with medication fluctuations and side effects.

Surgery: Deep Brain Stimulation for Parkinson’s Disease
Deep brain stimulation (DBS) is a surgery used to control Parkinson’s motor symptoms including tremor, slowness of movement and stiffness. DBS was FDA-approved for Parkinson’s disease in 2002 and works by delivering electrical pulses to specific areas of your brain that control movement. These electrical pulses disrupt the abnormal nerve signaling happening in your brain (thanks to your loss of dopamine and other brain changes caused by Parkinson’s). By interrupting the abnormal signals, DBS can improve your motor symptoms, reduce on/off fluctuations and reduce the severity of dyskinesia (muscle movement you can’t control).16 Some new research suggests DBS used in people with early-onset Parkinson’s may actually slow down the progression of tremors.14
If you undergo DBS, you will likely be awake for the first part of the surgery, although DBS can in some cases be performed under general anesthesia, while you’re asleep.9 Talk to your doctor about which option makes the most sense for your body. Here’s what you might expect if you and your doctor decide DBS is right for you.
The first step is placing a “halo” — a metal ring screwed into your head that keeps your head from moving. Local anesthesia is provided so it is not painful. However, some surgeries are now “frameless” and don’t require a halo. Then, you’ll receive a local anesthetic while a small hole is made in your skull, near your ear. Through this hole, a wire connected to an electrode (a thin metal device that conducts electricity) is placed in one or both sides of your brain in the areas that control movement. The wire and electrode are very thin.8
The surgeon will use computer-generated images of your brain to pinpoint the location where the electrodes should be placed, and will use surgical tools to physically insert the electrodes. No pain medication is needed while the electrode is implanted in your brain because there is no sensation in your brain. To make sure the electrode is placed in the right spot in your brain, the surgeons will temporarily stimulate the electricity and see if it affects your motor symptoms, and make sure nothing else in your brain is affected. (If you’re awake, you can talk to your surgeons and let them know how you are feeling). The whole procedure takes around three to six hours.
After a week or so healing process (you might feel foggy, fatigued or just “out of it”9), you will have another surgery to implant the neurostimulator device in your chest to stimulate the electrodes in your brain, unless you had both surgeries done simultaneously9. Under general anesthesia, a wire is run from the electrode in your brain, under your skin, down your neck and into the device implanted in your chest, under your skin. This device contains a battery and is the source of the electricity that stimulates the electrodes in your brain.
A few weeks later, after your surgery incisions have healed and you are clear of any infection, your doctor will then work with you to adjust the settings of the stimulator so you get the right amount of electrical stimulation delivered to your brain while avoiding potential side effects. For example, the stimulation can be turned up higher if you are still experiencing a tremor.23 It could also be turned lower if you are experiencing dyskinesia (excessive involuntary movements). You and your doctors will know it’s working when you are experiencing less tremor, slow movement and rigidity.
Receiving stimulation shouldn’t be painful. Depending on your symptoms, you might have constant, continuous stimulation, or you might turn the device off at night or other times of the day you don’t need stimulation. It can take several doctor’s visits to get the settings just right. You’ll also have a handheld programmer device you can use to turn the stimulator on, off, or possibly adjust the settings.23 For example, if you are experiencing worse symptoms, you may be able to adjust the stimulation to get some relief. You might not always adjust it perfectly, but with some tweaking and help from your doctor, you can often get back on track.9
If you have a rechargeable neurostimulator device, you will need to charge it periodically, by placing a special antenna device on your chest, on your skin over your neurostimulator. This device connects to a recharging device via a wire. The recharging device will then recharge the neurostimulator battery. You will need to have another surgery to replace the neurostimulator in about 10 to 15 years when the battery wears out. If you don’t have a rechargeable neurostimulator, you will need to have another surgery to replace your neurostimulator usually every two to five years. Keep in mind that higher DBS settings drain the battery more quickly and may require more frequent battery changes.
DBS is regarded as safe and effective and helps a majority of patients improve their movement symptoms and could even help you reduce the number of drugs you need to take.23 People who respond to medications typically respond similarly to DBS, whereas patients who do not respond to medications often do not benefit from DBS and may not be recommended for surgery.31
DBS candidates also shouldn’t have cognitive issues, like thinking or memory problems. If you do have some cognitive difficulty, DBS may make those issues worse.17 Other risks include a small chance of brain hemorrhage where an artery bursts in your brain, a brain or spinal cord fluid leak, or infection. DBS side effects can include temporary tingling in your face or limbs, allergic reaction to the implant, speech or vision issues, and dizziness.8 It’s important to remember that DBS only helps your main motor symptoms.37 Imbalance, freezing of gait, and swallowing difficulties are unlikely to improve with DBS and may worsen after surgery. It is extremely important to have DBS performed at an experienced center, where a panel of experts will evaluate your overall health to determine if you are a good candidate for the surgery.

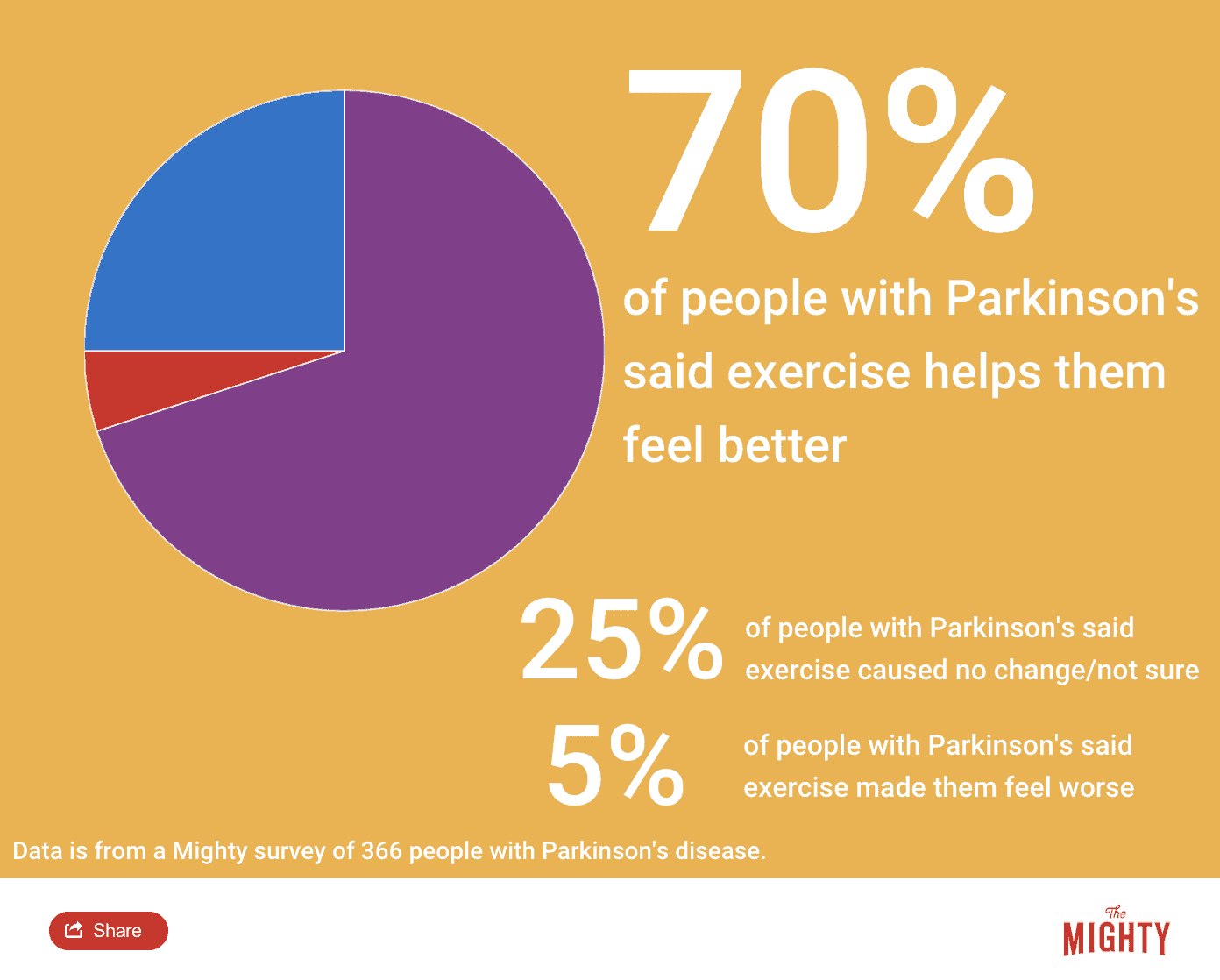
Exercise
At the same time you’re working with your doctor on figuring out your medication regimen, you should also look at one important way to manage your symptoms without medication: exercise. Studies show aerobic exercise that gets your heart rate up increases the amount of dopamine your body produces. Exercise can also improve your coordination, strength, balance, your cells’ production of energy, and brain function, and it may even slow down disease progression. Exercise also helps improve non-motor symptoms like depression, sleep and quality of life.
Any type of exercise is better than no exercise — the important thing is that you keep moving. Try walking, using the equipment at the gym, swimming, hiking, dancing, biking, yoga… anything you enjoy that gets you moving and is safe to do. There are even exercise classes specifically designed for people with Parkinson’s disease. These classes offer exercises tailored to movement issues you’re having, as well as a social benefit of meeting other people with Parkinson’s disease.
The best-known of these Parkinson’s exercise classes is Rock Steady Boxing, a nonprofit that offers boxing classes for people with Parkinson’s disease. It was founded in 2006 by a former lawyer who was diagnosed with Parkinson’s at age 40, and his friend, a boxer.34 Rock Steady Boxing classes can be found around the world and address Parkinson’s symptoms in a few specific ways. Boxing uses both sides of your body in opposition (for example, right arm and left leg movement), which can be great for improving coordination and strength. It has a thinking and memory-building element too since you have to remember a sequence of moves. It can also help with your voice since you need to call out different numbers. In addition, it provides time to socialize with others who get what you’re going through and feels empowering.13
You may be able to find other Parkinson’s exercise classes by doing some research in your own community. But at the end of the day, the most important thing is that you get some form of regular exercise.
Check out this video for more on why exercise should be a regular part of your treatment.

Other Therapies to Consider
Trained therapists across a number of disciplines can work with you to develop exercises and lifestyle strategies to improve specific challenges you’re having as a result of Parkinson’s disease. You don’t have to wait until you’re struggling to seek out a therapist — it’s important to intervene early. These lifestyle changes will hopefully benefit you now and down the road.37
Physical Therapy
A physical therapist can help you do exercises to improve your balance, gait, coordination and dealing with symptoms like freezing. For example, a physical therapist can teach you to cope with freezing episodes by using a laser which projects a line on the ground, stepping over such lines on the ground to cue your brain to start moving again, and walking assisted by rhythmic musical cues.13
One specific type of physical therapy for Parkinson’s is LSVT BIG, which utilizes overexaggerated movements to retrain your body’s smaller, slower movements caused by Parkinson’s. For example, buttoning a button with more purposeful, forceful movements, like you’re “angry” at the buttons, can help you button faster.22 Some research found LSVT BIG to be more effective at improving your movement abilities than general exercise.24 (Though you may find both helpful.)
Occupational Therapy
Occupational therapists teach you how to do everyday activities that have become difficult for you. For example, how to do daily tasks when you have a tremor (like putting on socks or brushing your teeth) and how to keep track of when your food has gone bad after you lose your sense of smell.13
Speech Therapy
Speech therapy helps you deal with vocal issues like a soft voice or slurring words, as well as swallowing issues.25 One specific type of speech therapy is LSVT LOUD, which coaches you to use a louder voice. Research demonstrates this therapy can improve vocal volume and vowel quality.12
Social Worker or Case Worker
A social worker can help you find mental health treatment, home health care programs, programs that provide financial assistance if you are unable to work and help with organizing childcare. They can help you identify which parts of your life are a struggle for you, and help connect you with resources to solve those problems.
Mental Health Support
Mental health is a significant component of Parkinson’s disease, both as a symptom and side effect of brain changes associated with Parkinson’s, medications and the overall stress of dealing with a chronic illness. Don’t be afraid to talk with your doctor about seeing a mental health professional like a psychiatrist, psychologist or therapist, or joining a support group. These professionals can help you with coping strategies and, if appropriate, mental health medications.13
Mobility Devices
As your disease progresses, you may find yourself having more difficulty with balance, walking, standing and stamina. Wheelchairs, scooters, walkers and canes are important tools that can prevent falls and other injuries and allow you to be more independent and go where you want. If you don’t like the thought of using a walker or other assistive devices, remember it’s important to protect you from falling and breaking a bone, which can be very dangerous.25
Nutrition
There is no specific “Parkinson’s diet,” though some research suggests following a Mediterranean diet consisting of vegetables, legumes, fruit, cereals, unsaturated fatty acids, fish and wine with low-to-moderate dairy, meat and poultry and limited processed foods and sweets is associated with a lower risk of developing Parkinson’s disease.3 In addition, since constipation is a common Parkinson’s symptom, it’s a good idea to eat high fiber foods and drink plenty of water to keep your digestive system moving.13
One specific dietary requirement you should be aware of is that protein can interfere with your absorption of the medication levodopa. Levodopa competes with protein to be absorbed in your gut, so protein from your food may get absorbed while the levodopa doesn’t, reducing its effectiveness. For this reason, it’s best to take levodopa around 45 minutes before you eat or 60 minutes after you eat so you leave a gap that allows the medication to be absorbed without competing with food.13
Social Support
Like many (if not most) other illnesses, Parkinson’s can feel much more manageable if you have a strong support system of family and friends. People who report having strong social support also tend to describe having a more positive life experience with Parkinson’s.4 Fighting loneliness by spending time with loved ones can help reduce depression, keep you more physically active, reduce stress by providing support for everyday tasks (like rides to doctor’s appointments and help shopping) and help you stay engaged in your hobbies and interests.
Alternative Therapies
Alternative or complementary therapies include things like acupuncture, massage and herbal medicine. There is not a lot of documented evidence complementary methods help Parkinson’s more than medication and exercise. These therapies have not been studied specifically for Parkinson’s disease and don’t come with a list of potential side effects, dosages, risks or instructions specific to Parkinson’s disease. But just because there isn’t a list doesn’t mean there aren’t risks, like interacting with other medications you’ve been prescribed. Always check with your doctor before trying a new treatment method.37 That being said, the following therapies may be of interest to you.
Mindfulness
Mindfulness focuses on becoming more aware of your body and the present moment you are in. Some research found mindfulness techniques led to a small increase in reported pain, but also improvements in motor symptoms and increased reported quality of life.30
Whether you practice mindfulness or other forms of stress-reduction, like meditation, massage, art or music therapy, or reiki, it’s important to seek out ways to reduce your overall stress levels, as stress can make symptoms feel worse.33 Find your favorite ways to cope with stress and incorporate them into your routine.
Supplements
Supplements should be taken with extreme caution under a doctor’s supervision. Some supplements affect how quickly you will absorb your other medications, so it can be dangerous to take them without a doctor’s input. One supplement is velvet bean (mucuna pruriens), which contains naturally-occurring levodopa. If you don’t want to take levodopa medication, your doctor might be OK with you taking velvet bean so you at least get a little levodopa in your system.25 However, the amount of dopamine in each dose of mucuna pruriens can vary, and therefore may cause unpredictable side effects. Again, talk to your doctor before trying any supplements.
Positive attitude
“Thinking positively” is certainly not a “cure” for Parkinson’s disease, and you should never feel pressured to “just be positive” all the time. However, your outlook on your disease and future can make a difference in how you approach the condition — and how you experience it. Two people can have the same “version” of Parkinson’s, but one person’s outlook might be more hopeful: for example, they exercise, take charge of their health and focus on having a hopeful view of their future. The person with a worse outlook, who doesn’t exercise, doesn’t take an active role in their care and focuses on the negatives, may not do as well.37
Positivity can look different for everyone. Maybe for you, a positive attitude is cultivated through faith; for someone else, focusing on hobbies, friends and family helps them stay hopeful. A positive outlook isn’t a cure-all, but it certainly doesn’t hurt.

Parkinson’s Community Recommendations
Mighty community member Allison shared these top seven things healthy “Parkies” do, which can serve as a guide to help integrate healthy ways of getting ahead of your Parkinson’s:
- Don’t treat exercise as optional.
- Follow through with your neurologist’s recommendations.
- Don’t see yourself as weak or a burden.
- Regardless of diagnosis, remain grateful.
- Be your own advocate.
- Give yourself permission not to be perfect.
- Beef up your PD “wolfpack” — your support system.
Discover why these seven tips are so important here.
Another member of our Parkinson’s community, Bruce Ballard, shared his “seven habits of highly effective Parkies.” Check them out below:
- Exercise frequently and (if you can) walk everywhere.
- Challenge yourself with simple tasks Parkinson’s disease tried to put a stop to.
- Listen to your favorite music on playlists, but play the songs in random order.
- Balance what you eat to avoid constipation and its opposite partner in crime, fecal incontinence.
- Learn something new.
- Maintain good sleep hygiene.
- Socialize and have fun.
Learn more about Parkinson’s: Overview | Symptoms | Diagnosis | Resources

Sources
- Abbott, A. (2010). Levodopa: the story so far. Nature, S6–S7. doi: https://doi.org/10.1038/466S6a
- About NUPLAZID® (pimavanserin) (n.d.). Retrieved from https://www.nuplazid.com/about-nuplazid#isi.
- Alcalay, R. N., Gu, Y., Mejia-Santana, H., Cote, L., Marder, K. S., & Scarmeas, N. (2012). The association between Mediterranean diet adherence and Parkinsons disease. Movement Disorders, 27(6), 771–774. doi: 10.1002/mds.24918
- Ambrosio, L. C., Portillo, M. M., Rodriguez‐Blazquez, C. R., Rojo, J. C. M., Martinez‐Martin, P. C., Violante, M. S., … undefined, undefined undefined. (2019). Influencing factors when living with Parkinson’s disease: A cross‐sectional study. Journal of Clinical Nursing, 28(17-18), 3168–3176. doi: 10.1111/jocn.14868>
- Bonifacio, M. J., Palma, P. N., Almeida, L., & Soares-da-Silva, P. (2007). Catechol‐O‐methyltransferase and Its Inhibitors in Parkinson’s Disease. CNS Drug Reviews, 13(3), 352–379. Retrieved from https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1527-3458.2007.00020.x
- Borovac, J. A. (2916). Side effects of a dopamine agonist therapy for Parkinson’s disease: a mini-review of clinical pharmacology. Yale Journal of Biology and Medicine, 89(1), 37–47.
- Chagas, M. H., Zuardi, A. W., Tumas, V., Pena-Pereira, M. A., Sobreira, E. T., Bergamaschi, M. M., … Crippa, J. A. (2014). Effects of cannabidiol in the treatment of patients with Parkinson’s disease. Journal of Psychopharmacology, 28(11), 1088–1098. doi: 10.1177/0269881114550355
- Deep Brain Stimulation. (n.d.). Retrieved from https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Deep-Brain-Stimulation.
- Eagles, M. (2019, April 23). [E-mail interview].
- Eagles, Matt. (2019, August 20). [E-mail interview].
- EXELON PATCH. (n.d.). Retrieved from http://www.exelonpatch.com/index.jsp.
- Fox, C., Ebersbach, G., Ramig, L., & Sapir, S. (2012). LSVT LOUD and LSVT BIG: Behavioral Treatment Programs for Speech and Body Movement in Parkinson Disease. Parkinsons Disease, 2012, 1–12. doi: 10.1155/2012/391946
- Goldman, J. (2019, May 3). [Telephone interview].
- Hacker, M. L., Delong, M. R., Turchan, M., Heusinkveld, L. E., Ostrem, J. L., Molinari, A. L., … Charles, D. (2018). Effects of deep brain stimulation on rest tremor progression in early stage Parkinson disease. Neurology, 91(5). doi: 10.1212/wnl.0000000000005903
- Have you heard about Duopa® (carbidopa and levodopa)? (n.d.). Retrieved from https://www.duopa.com/advanced-parkinsons-disease-treatment/delivery-system.
- Hickey, P., & Stacy, M. (2016). Deep Brain Stimulation: A Paradigm Shifting Approach to Treat Parkinsons Disease. Frontiers in Neuroscience, 10. doi: 10.3389/fnins.2016.00173
- Inacio, P. (2019, February 1). In Parkinson’s, Deep Brain Stimulation May Raise Dementia Risk, Study Says. Retrieved from https://parkinsonsnewstoday.com/2019/02/01/deep-brain-stimulation-increased-risk-dementia/.
- Learn more about INBRIJA. (n.d.). Retrieved from https://www.inbrija.com/about.
- Lees, A.J. (2002). Drugs for Parkinson’s disease. Journal of Neurology, Neurosurgery & Psychiatry, 73, 607-610.
- Lopes, J. M. (2019, January 15). Parkinson’s Therapy Inbrija Approved in US for Treatment of Off Periods. Retrieved from https://parkinsonsnewstoday.com/2019/01/10/fda-approves-inbrija-treatment-off-periods/.
- Lotan, I., Treves, T. A., Roditi, Y., & Djaldetti, R. (2014). Cannabis (Medical Marijuana) Treatment for Motor and Non–Motor Symptoms of Parkinson Disease. Clinical Neuropharmacology, 37(2), 41–44. doi: 10.1097/wnf.0000000000000016
- LSVT BIG. (n.d.). Retrieved from https://www.lsvtglobal.com/LSVTBig.
- Luca, C. (2019, April 23). [Telephone interview].
- Mcdonnell, M. N., Rischbieth, B., Schammer, T. T., Seaforth, C., Shaw, A. J., & Phillips, A. C. (2017). Lee Silverman Voice Treatment (LSVT)-BIG to improve motor function in people with Parkinson’s disease: a systematic review and meta-analysis. Clinical Rehabilitation, 32(5), 607–618. doi: 10.1177/0269215517734385
- McKeown, M. (2019, May 6). [Telephone interview].
- Northera. (n.d.) Retrieved from https://www.northera.com.
- Oliveira de Carvalho, A., Filho, A., Murillo-Rodriguez, E., Rocha, N. B., Carta, M. G., & Machado, S. (2018). Physical Exercise For Parkinson’s Disease: Clinical And Experimental Evidence. Clinical Practice and Epidemiology in Mental Health:CP & EMH, 14, 89–98. doi:10.2174/1745017901814010089
- Ovallath, S., & Sulthana, B. (2017). Levodopa: History and Therapeutic Applications. Annals of Indian Academy of Neurology, 20(3), 185–189. doi: 10.4103/aian.AIAN_241_17
- Percutaneous Endoscopic Gastrostomy (PEG) Procedure Details. (n.d.). Retrieved from https://my.clevelandclinic.org/health/treatments/4911-percutaneous-endoscopic-gastrostomy-peg/procedure-details. >
- Pickut, B., Vanneste, S., Hirsch, M. A., Hecke, W. V., Kerckhofs, E., Mariën, P., … Cras, P. (2015). Mindfulness Training among Individuals with Parkinson’s Disease: Neurobehavioral Effects. Parkinsons Disease, 2015, 1–6. doi: 10.1155/2015/816404
- Quinn, J. (2019, May 7). [Telephone interview].
- Riederer, P., & Laux, G. (2011). MAO-inhibitors in Parkinsons Disease. Experimental Neurobiology, 20(1), 1–17. doi: 10.5607/en.2011.20.1.1
- Robb, K. (2019, May 5). [E-mail interview].
- Rock Steady Boxing. (n.d.). Retrieved from https://www.rocksteadyboxing.org.
- Tagliati, M. (2019, April 25). [Telephone interview].
- Virhammar, J., & Nyholm, D. (2016). Levodopa-carbidopa enteral suspension in advanced Parkinson’s disease: clinical evidence and experience. Therapeutic Advances in Neurological Disorders, 10(3), 171–187. doi: 10.1177/1756285616681280
- Yang, L. (2019, May 3). [Telephone interview].
- Zuardi, A. W., Crippa, J. A., Hallak, J. E., Pinto, J. P., Chagas, M. H., Rodrigues, G. G., … Tumas, V. (2009). Cannabidiol for the treatment of psychosis in Parkinson’s disease. Journal of Psychopharmacology, 23(8), 979–983. doi: 10.1177/0269881108096519