What is Hidradenitis Suppurativa? All You Need to Know
Editor's Note
The Mighty’s educational content combines the expertise of both the medical and patient community to support you and your loved ones through your health journeys. For this hidradenitis suppurativa (HS) condition guide, we connected with three HS experts, read the latest studies and surveyed more than 40 people living with HS and their caregivers.
Hidradenitis Suppurativa at a Glance:
- Hidradenitis suppurativa (HS) is a chronic inflammatory condition that primarily affects the skin, causing painful lesions.
- Between 1-4% of people globally live with hidradenitis suppurativa (HS). However, there are likely many more cases that go undiagnosed because HS can mimic other skin conditions.1
- There are many options for HS management, including medications, lifestyle changes and surgery, but treatment often requires adjustment and a combination of approaches over time to get the best long-term control.2

Medically reviewed by Dr. Chris Sayed, M.D.
What Is Hidradenitis Suppurativa? | Common HS Misconceptions | Managing HS | Mental Health and HS | How To Talk To Others About HS | How To Find a Health Care Provider for HS | How To Support Someone With HS |
What Is Hidradenitis Suppurativa (HS)?
Hidradenitis suppurativa (hi-drad-uh-NIE-tis sup-yoo-ruh-TEE-vuh) may seem daunting to read about at first because of its complex name, but don’t worry, people often refer to the condition by its acronym, HS. Understanding how HS can affect the body and learning ways to treat the condition may require some new vocabulary. Before we dive deeper, here are a few key terms you should be familiar with:
- Follicle: The cylindrical structure made of cells in the outer layer of skin that opens to the surface of the skin and produces hair and oils
- Abscess: A lump or pocket of pus caused by an immune system reaction
- Sinus tract (tunnel): A space that forms under the skin that connects to the surface in one or more places and may be tender and leak pus
- Inflammation: An immune reaction that typically leads to redness, pain, swelling, and/or pus in response to infection or as a result of diseases in which it is not controlled properly.
HS is a chronic inflammatory skin condition that affects the hair follicles in areas of the body with a predilection for areas of hormone-dependent hair growth and where skin can rub together, such as the thighs, armpits, groin and buttocks.3 People living with HS usually first notice painful lumps under the skin in these areas, which may grow in size and drain pus or fade over the course of a few weeks. Some lesions do not heal over a short period of time and become chronic; these lesions may flare repeatedly over time. Other common hidradenitis suppurativa symptoms include soreness, scarring and fatigue.
Understanding how HS develops and progresses is complicated and still somewhat unknown. Current research suggests that HS occurs due to an inflammation around hair follicles, causing reddened bumps to appear. This might be due to the body overreacting to normal bacteria that live in the skin and hair follicles or fragility of hair follicles that causes them to rupture and spark an inflammatory reaction in the body.4 These reactions can form abscesses in different locations on the body. People who live with HS can experience the condition in differing levels of severity, which usually are classified by the Hurley Staging System:
- Stage I: One or few isolated nodules or abscesses in the skin that don’t result in scarring or sinus tracts
- Stage II: Defined by the presence of one or limited widely separated sinus tracts (tunnels) and/or scars related to HS in a body region
- Stage III: Multiple sinus tracts (tunnels) and scars that extensively affect a body region
Scientists are still trying to understand what is the root cause of hidradenitis suppurativa. There appears to be some genetic factors at play. According to one study, approximately 50% of people with HS reported a family history of the condition.5 Other factors that may contribute to HS include smoking, obesity and hormonal imbalances.6
Hidradenitis suppurativa most often affects younger women, with women overall three times more likely to have HS than men.6 While researchers are not yet sure why it is more common in women, it is likely that hormones play a role in the underlying cause or trigger for HS. Although HS is more common in women, men often have more severe forms of the condition.7
How Is Hidradenitis Suppurativa Diagnosed?
Hidradenitis suppurativa (HS) is diagnosed through a physical examination and study of a patient’s medical history. Unfortunately, there is no specific test for HS. However, your doctor may suggest biopsies or other laboratory tests to help rule out other diagnoses before making a HS diagnosis.7
Receiving an HS diagnosis can be a long journey: A recent study showed that the average time taken to reach an HS diagnosis is 10 years.8 Amit Garg, M.D., an HS specialist from Northwell, stressed the importance of addressing this issue:
“[I often see] HS patients that have symptoms for 7 to 10 years on average before a formal diagnosis of HS is given to them. And they experience symptom flares, but probably even progression of their disease. Helping patients and physicians navigate this issue of delayed diagnosis can support the overall care strategy much more effectively for HS patients.”
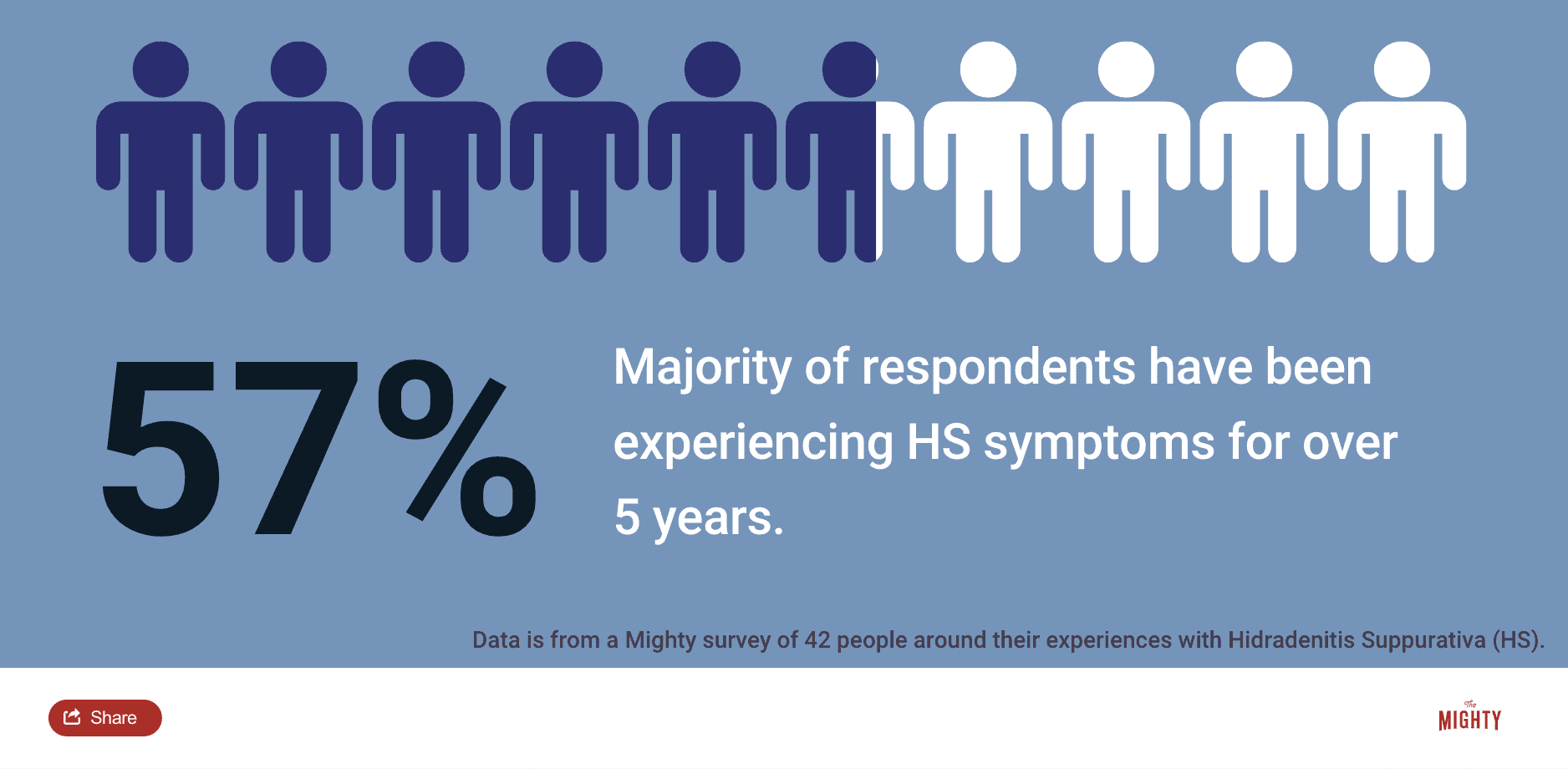
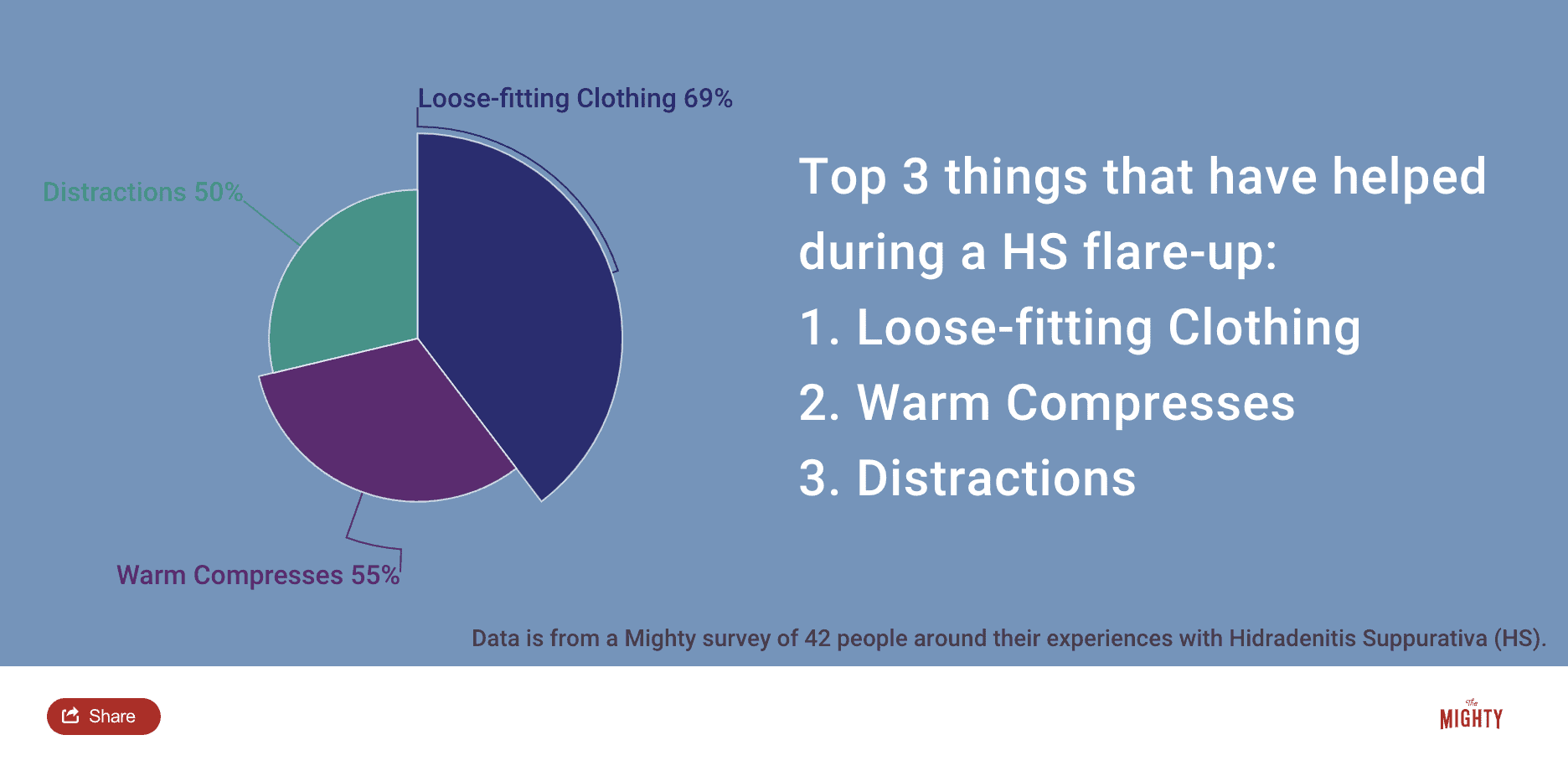
If you have waited a long time for the right diagnosis, you are not alone. To better understand the diagnosis journey for HS patients, we surveyed the Mighty community to learn more about their experience. Here is what they had to say:
- “I’m a retired nurse and it took a long time for a diagnosis! I had to tell the doctors what I thought I had and they thought I was a hypochondriac even with the symptoms I had.”
- “Mine was misdiagnosed for 23 years because my body type didn’t really fit what doctors normally see with HS patients.”
- “I’ve been asking doctors of all kinds about this health problem for about 15 years. Approximately 8 to 10 doctors and none knew what this is.”
In The Mighty’s survey, the majority of respondents experienced symptoms for over five years and nearly 30% still haven’t received a formal diagnosis. So why is HS so hard to diagnose? The truth is, HS is not a well-known condition in the medical community. It can be difficult to diagnose HS correctly, especially in the early stages of the condition and if the health care professional is not a dermatologist. Common misdiagnoses include:7
- Inflamed cysts
- Abscesses/boils
- Acne
- Cellulitis
- Herpes or other infectious diseases
Do some of these misdiagnoses seem familiar to you? HS mimics other conditions, but there are a few key differences between having HS and a “regular” cyst or abscess. A good dermatologist will assess you for the following HS-specific characteristics:
- Are your symptoms focused in a specific location like the armpits, groin or buttocks?
- Are your symptoms chronic?
- Do your abscesses have any scarring after a flare?
If you’re feeling frustrated and overwhelmed in your diagnosis journey, Mighty contributor Kashinda Marche wants to share this important reminder with you:
“One of the most powerful resources is yourself. You have to get to know yourself with this condition and figure out what works for you.”
Conditions That Occur With Hidradenitis Suppurativa
For people living with hidradenitis suppurativa, there are several somewhat unexpected conditions that people may experience alongside HS. While HS symptoms primarily affect the skin, the inflammation and psychological stress from living with HS can have an impact on other areas of the body as well.6
Here are some conditions that people who live with HS may also have:
Metabolic Syndrome
Metabolic syndrome is a group of health conditions that can have a large impact on the body. People who live with metabolic syndrome often have high blood pressure, triglycerides and blood sugar, which may lead to diabetes and cardiovascular disease. Obesity is also common.9 Metabolic syndrome increases inflammation in the body, which can be a key driver that can worsen HS symptoms. In a recent study, it was estimated that approximately 50% of people who live with HS also have metabolic syndrome.10
Because many people who are diagnosed with HS are also obese, it has led to the misconception that being overweight causes HS. There is no clear evidence that obesity causes HS. While maintaining a healthy weight is one of the lifestyle changes doctors recommend to help manage HS, it is only one tool in the HS management toolbelt: A hidradenitis suppurativa diet, focusing on balanced, nutritious meals, can be a part of this strategy, aiding in weight management and overall health. Yet, it’s important to remember that HS is a complex condition that likely can not be managed by weight loss alone.
Polycystic Ovarian Syndrome
Polycystic ovarian syndrome (PCOS) is a condition associated with irregular periods, excess levels of androgens like testosterone and cysts in the ovaries. A recent study showed that around 9% of women who had HS were also diagnosed with PCOS compared to 2.9% of women who did not have HS.11 The likelihood of women having PCOS and HS also increased in women who were obese and/or had diabetes.11
Because of this overlap in conditions, doctors who specialize in HS may prescribe hormone-blocking medications that are used to treat PCOS.12
Ulcerative Colitis, Crohn’s Disease and Arthritis
Inflammation throughout the body can worsen HS symptoms and is also associated with other health conditions like ulcerative colitis (UC), Crohn’s disease and arthritis. People diagnosed with HS may also experience symptoms related to UC and arthritis because of body-wide inflammation.
Because researchers have linked HS inflammation with other conditions that have a similar cause, some treatment options such as biologics — which are also used in arthritis and UC patients — have become available for HS as well.13
If reading about “one more thing” that may be added to the HS-related symptom bucket makes you feel anxious, Katie Meade, a Mighty HS contributor, wants you to know:
“Having HS with a combination of other chronic illnesses can be stressful and it may be hard to focus on several symptoms at once. My advice is to take it one symptom at a time and treat it the best you can, no matter how hard it is.”
When Other Health Conditions Tag Along With Hidradenitis Suppurativa
Mental Health Conditions
An often overlooked aspect of living with a chronic illness is the potential mental health impact. While HS is a very “visible” disease and treatment may be focused on the physical symptoms of the condition, many people living with HS also experience anxiety and depression symptoms.14 Like many physical health conditions, talking openly about mental health can sometimes be even more important than discussing direct symptoms. That’s why we’ve dedicated a section of this condition guide to mental health and HS.
Read more about life with HS from fellow Mighties here:
- People With Hidradenitis Suppurativa Share the Advice They Wish They Heard After Their Diagnosis
- What It’s Like Having Hidradenitis Suppurativa
- A Letter to the Person Diagnosed With Hidradenitis Suppurativa
- A Day in My Life During a Hidradenitis Suppurativa Flare-Up

Common Hidradenitis Suppurativa Misconceptions
Hidradenitis suppurativa (HS) can be extra challenging because of the impact the condition can have on your mental health, body image and self-esteem, which is often worsened by the stigma and misconceptions surrounding the condition.
HS and Obesity
One of the common misconceptions about HS is that people living with it “just need to lose weight” to control the condition. Although many people living with HS also experience obesity, the relationship between weight and HS symptoms is not as clear-cut as others may think.
There is no clear evidence that obesity causes HS. It is more likely that an underlying factor is contributing to both obesity and HS. Inflammatory conditions like HS are complex and often require multiple types of treatment to help control the condition — managing weight is only one potential treatment option.
“Lack” of Hygiene
HS can be difficult to hide and people may think of those struggling with HS as “unclean” because of the odor that some people may experience from abscess drainage. HS is not, however, caused by a lack of personal hygiene.
If you feel frustrated by this HS misconception, Allyson Byers, a Mighty HS contributor, wants you to know:
“I and so many others shower way more than the average person. HS really has nothing to do with your hygiene: you could be the cleanest person in the world and still get HS.”
HS and Sexually Transmitted Diseases
Because HS can occur in the groin area, there is also a common misconception that HS is a sexually transmitted disease (STD). This myth can create challenges with intimacy and dating because of the stigma associated with STDs in addition to the other misconceptions associated with HS. One Mighty member from our HS survey wants you to know:
“It’s not an STD, it’s not contagious. I feel insecure about not being able to wear regular underwear or the clothes I want because I have to wear loose-fitting clothes and men’s underwear. I can’t wear the bathing suits I normally wear, so I’m stuck with wearing things that don’t look good on me. I am intimidated by sexual intimacy because I am so embarrassed about my symptoms.”
Skin Conditions
When people think of skin conditions, acne and eczema often come to mind. HS is classified as a skin condition and there is a common misconception that skin problems can’t be severe. As Allyson Byers said:
“I hate whenever I say skin condition. I just feel like people are like, ‘Oh, that’s very mild’ and try to minimize how much it really affects my daily life.”
To learn more about what people living with HS have to say about misconceptions, check out these stories:
- 7 Misconceptions About Hidradenitis Suppurativa
- What I Want Others to Know About Life With HS
- Having Hidradenitis Suppurativa Does Not Make Me ‘Dirty’

Managing Hidradenitis Suppurativa
Finding a treatment regimen that works for hidradenitis suppurativa (HS) can be difficult because each person experiences the condition differently. The challenge of finding an appropriate therapy is compounded by the fact that the hidradenitis suppurativa causes are still poorly understood. If you looked up HS online after you received the diagnosis, you may be overwhelmed by what you found. You may be asking yourself:
- Will I ever be able to have a “normal” life?
- What does surgery for HS look like?
- Is HS progressive?
HS is a condition that has periods of worsening symptoms, called flares, which can sometimes improve on their own but usually require treatment. It can also have periods of time with few symptoms. The frequency and severity of flares depend on your HS severity stage. Recognizing the hidradenitis suppurativa stages is vital to choosing the correct therapies, as the condition can develop from isolated nodules (Stage I) to a widespread presence of sinus tracts and scars (Stage III). The type of hidradenitis suppurativa medication prescribed is typically tailored to the patient’s particular stage and severity. (If you missed that section, you can review the Hurley Staging System here).
The goal of HS management is to reduce the severity of your symptoms and to prevent symptoms from worsening, or in some cases, coming back at all.15 That’s why it’s important to work with your health care team not only when you’re experiencing a flare, but also when you’re feeling better.
Although there is currently no cure for HS, scientists and doctors are working together to find new ways to help manage the condition. To help relieve HS symptoms, there are many different strategies that fall under the umbrella of hidradenitis suppurativa treatment to explore with your health care team. Some of these options may include medication, surgical interventions and lifestyle changes.
Medications for HS often target inflammation in the body as well as bacterial infections. Your doctor may also recommend options to lower androgens like testosterone. Some medication types include:2,12
- Corticosteroids
- Antibiotics
- Immunomodulators
- Biologics
- Hormone blockers
Sometimes, medications alone are not sufficient to manage an HS flare and your dermatologist may recommend surgical interventions. The goal of surgery for HS symptoms is usually to excise, or remove, areas particularly affected by HS, like connected sinus tracts.15 Surgical interventions for HS can include:16
- Incision and drainage
- Unroofing
- Laser surgery
- Wide excision
Please note: images of surgery can be graphic and may be triggering to some individuals. Please explore hidradenitis suppurativa pictures of surgeries on the internet with caution.
Talking with your care team is important, not only in reducing your symptoms, but also in helping to prevent your HS from getting worse. HS is classified as a progressive disease, meaning that it often gets worse over time without treatment.7 However, with a good health care team, you can help create a toolbox of resources and interventions that yield the best outcome for your HS.
While we all wish for a permanent cure for hidradenitis suppurativa, the current reality is that treating this chronic condition typically involves long-term treatment plans and lifestyle changes, but research is ongoing and we remain hopeful for future breakthroughs.
So what does “successful” management of HS look like? Dr. Garg, an HS specialist from Northwell, says:
“Success to me is when a patient tells me he or she is satisfied with the control of symptoms, and that the disease has minimal impact on their lives.”
The first step toward managing your HS as well as possible is building a health care team best suited to your needs. Some resources that may help get started include:
How To Build a Health Care Team for Hidradenitis Suppurativa:
Although HS affects approximately 1% of people, it is still an under-diagnosed condition and it’s not rare for health care providers to be unfamiliar with the condition.1 That’s why finding the right health care team to support you is key in navigating life with hidradenitis suppurativa (HS).
You may be reading this and feel frustrated about trying to find a health care provider for your HS. Locating the right support for any chronic condition can take time and a little bit of trial and error. HS can be complex to treat and finding the right support can help you better navigate living with the condition, not only in regards to the physical symptoms but also with your mental health.
But where to begin? If you feel overwhelmed while looking for an HS-informed dermatologist, taking small steps can make the process easier. First, try to identify a primary care physician you trust and feel comfortable talking about your HS symptoms with. Your primary care physician can act as a centralized resource center and help you navigate the process of finding the right specialists to help in your care.
Here are the types of health care professionals who can help manage HS symptoms:
- Primary care physician (PCP)
- Dermatologist
- OB/GYN
- Surgeon
- Rheumatologist
- Mental health professional
It may seem like a long, winding journey to finding the best team for you, but know that it’s worth it. In her story, Why Finding a Doctor Who Is a Good Fit Is Important When Living With Hidradenitis Suppurativa,” Allyson Byers shared her experience of what finding the right doctor can feel like:
“When the doctor walked into our consultation, I felt like a whole person, not just an HS patient. She cared about my depression and anxiety and how it related to having HS. She took charge, and I felt cared for. I felt hope for the first time in a while. She gave me referrals to other specialists who could help. I left the office feeling in a better, not worse, mood. I trusted her. I felt heard.”
Like Allyson, you deserve to be heard. Being vulnerable about what you’re going through is possibly one of the bravest things you can do.
Talking To Your Health Care Provider About Hidradenitis Suppurativa
Talking to a health care provider about your hidradenitis suppurativa (HS) symptoms can be nerve-wracking. Whether you’re doing so for the first time or the 100th time, we’re proud of you for making strides to take care of yourself. In her story, “How To Make the Most Out of Doctor’s Appointments With Hidradenitis Suppurativa,” Allyson Byers shared her tips on talking to health care providers about HS.
If you’re feeling apprehensive about sharing everything with a health care provider, read this:
“It’s easy to feel embarrassed when you have boils or lesions in areas like your groin, butt or breasts. But it’s important to remind yourself that they are a medical professional who needs to have all the relevant information to help. Anytime I’ve chosen to not show certain flare-ups because I felt self-conscious, I’ve regretted it as soon as I walked out of the building.”
Allyson also recommended recording your HS symptoms to guide the conversation with your provider. While keeping track of symptoms can feel overwhelming at times, without an organized system in place, it can be hard to truly analyze how you’re feeling from day to day. An intentional monitoring system like a symptom tracker can help your health care team create a treatment plan that’s unique to you. To help support you in this journey, here’s an HS-specific symptom tracker we made to get you started.
To help you navigate your next visit with a health care professional, we also created a downloadable discussion guide. We hope this guide helps you get the most out of your appointments:
Hidradenitis Suppurativa Health Care Provider Discussion Guide
You can also find other health care team resources here:
- How To Make the Most Out of Doctor’s Appointments With Hidradenitis Suppurativa
- What Medical Professionals Often Get Wrong About Hidradenitis Suppurativa
- 5 Questions I Wish I Had Asked When I Was Diagnosed With Hidradenitis Suppurativa
Other Ways To Manage Living With Hidradenitis Suppurativa
Hygiene Tips
Staying on top of hygiene with hidradenitis suppurativa is important not only to help with wound healing and to prevent symptoms from getting worse, but also for your mental health. But hygiene and HS can be tricky. Before we begin talking about hygiene and HS, here’s a reminder you may need today: poor hygiene isn’t the cause of HS.
People living with HS may struggle with shaving and using deodorants/antiperspirants because they can irritate the skin. If these two tasks worsen your symptoms, try using natural or spray deodorants. If shaving is problematic, you can try laser hair removal or forego shaving altogether.
Another aspect of living with HS is wound care, especially during flares. Having open wounds from abscesses isn’t easy to tackle, but luckily, Mighty member Tiffany is here with some handy advice:
“I keep most of [my wounds] bandaged using tape, gauze, pads and either sterile water or antibiotic cream. I change them one to two times a day and shower daily and air out in front of a fan after reapplying bandages. This keeps them as dry as possible while also protecting my clothing and furniture.”
8 Hygiene Tips for People Living With Hidradenitis Suppurativa
Dressing for Life With Hidradenitis Suppurativa
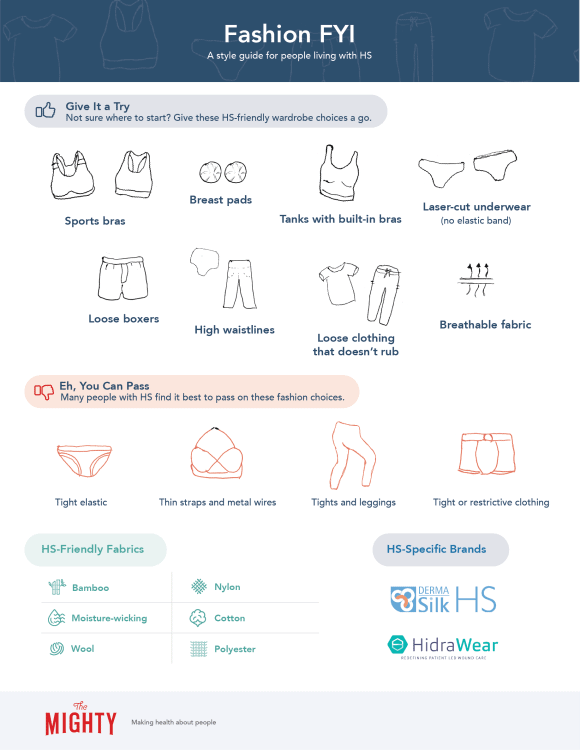
Maintaining a positive body image can be difficult when living with hidradenitis suppurativa, especially during a flare. You may be anxious picking out clothes that are HS-friendly and may be asking yourself these questions when shopping for a new wardrobe:
- Will the drainage stain these clothes?
- Will the material irritate my skin?
- Is the material breathable?
- Will the style cover my flare-ups?
Everyone deserves to feel comfortable in their own skin, and wearing HS-friendly clothes can boost your self-esteem as well as prevent future flares. That’s why we interviewed Mighties, who live with HS, to create a style guide just for you!
Hidradenitis Suppurativa Self-Care Tips
No matter what you’re going through, self-care serves as an important and often overlooked pillar in managing a health condition, whether that looks like a five-minute midday meditation or whipping up a batch of your favorite cookies. We asked fellow Mighties what HS-specific self-care practices they’d recommend.
Here’s what Mighty contributor Allyson Byers had to say:
“I’ve decided recently to just get my laundry done. It’s so hard for me to do laundry. I’m going through clothes so fast, I can be [at] the laundry machine all day long.”
If a laundry service isn’t for you, she also suggested taking it easy with naps and restorative yoga:
“Naps are a really big thing. I just get so tired. It’s just because your body’s fighting itself all day, so I allow myself to take at least like every afternoon. I do a lot of restorative yoga. I loved going to spin class but that just exacerbated symptoms. So something like restorative yoga is really easy. And I can still just go at my own pace, but it still feels like I’m moving my body a little bit.”
In her story, “What Self-Care Looks Like With Hidradenitis Suppurativa,” Mighty contributor Katie Meade suggested exploring moisturizers and finding a skin-care regimen that works for you. Another self-care tip she suggested? Try a body pillow:
“Relaxing with a body pillow, or a long pillow, helped me a lot before I went into remission with my HS. It helped me not only sleep, but also helped me spread my arms out, away from the HS site.”
Have any self-care suggestions to add? We’d love to know! Pop them in the comments at the end of this guide to share them with your fellow Mighties.
Mental Health and Hidradenitis Suppurativa
When we talk about hidradenitis suppurativa, it’s important to remember that living with the condition can also have a major impact on your mental health.
Recent studies suggest depression rates of those living with HS are higher than for other skin conditions.17 The psychological effects for people living with HS were comparable to people living with cancer, cardiovascular or lung conditions.18
Based on what we know, it’s so important to talk about the connection between mental health and HS: there is more to living with HS than what you can see. HS can lead to a number of mental health issues, including substance use, depression, anxiety, body dysmorphia and suicidal ideation. Accordingly, treatment plans for hidradenitis suppurativa should factor in mental health support.19
If you are struggling with your mental health because of HS, know that you’re not alone. Mighty contributor Allyson Byers shared how HS affects her anxiety:
“With chronic illnesses, you have no idea what the next day is going to bring. Are you going to wake up with a new lesion or boil? Or are you going to have to cancel plans? Can you work the next day? It’s just really stressful to try and live in the moment and enjoy things but also not be freaked out about what’s going to happen tomorrow. Or even in the future, are things just going to get worse?”
Tackling stigmas associated with HS can also be taxing, and you may feel shame about having HS. Sometimes finding community can make a huge difference in how you feel about yourself. Mighty contributor Kashinda Marche shared this advice:
“Finding others who live with HS can help because it helps take the weight off of the shame from it. You’re not as shameful anymore because now you’re amongst 10 other people like you. You’re talking about this ‘gross’ and painful condition, but then you learn that they’ve got families, too. It just makes things a little bit lighter in that area. Which makes the whole emotional weight from HS a little bit lighter.”
If you’re looking for a place to connect about HS, you can check out The Mighty’s HS topic page and post Thoughts and Questions in the HS community. You can also read these stories from Mighties who have been there:
- How I Took My Self-Esteem Back From Hidradenitis Suppurativa
- Learning to Love and Care for Myself With Hidradenitis Suppurativa
You can also find HS-specific patient support groups at Hope For HS, a nonprofit that advocates for HS patients.
How to Get Help In a Crisis
If you’re struggling with suicidal thoughts, know you are not alone — and there is help for people who feel suicidal. If you need help right now, you can call the National Suicide Prevention Lifeline at 1-800-273-8255 or text “START” to 741-741. Head here for a list of crisis centers around the world, and visit our suicide prevention resources here.
How To Talk To Others About Hidradenitis Suppurativa
Talking about your experience living with hidradenitis suppurativa (HS) with others, especially those unfamiliar with the condition, can be difficult. They may not understand how big of an impact HS can have on your daily life and mental health. They may get bogged down by the misconceptions associated with the condition.
While talking about difficult things can be draining (you’re doing great, by the way), we hope you can find someone who you feel comfortable talking about your needs and experiences with — whether it’s your doctor, someone in your family or a partner. If you need a place to turn, our Mighty community is always here for you.
Talking To Friends and Family About Hidradenitis Suppurativa
Picture this: Your family and friends want to go hiking, spend a day at the beach or get lunch outside on a hot summer day. In all their excitement, they may not realize that some activities can actually worsen your HS symptoms or cause more pain. You may be tempted to go and feel “normal,” but later regret doing so because of the increased symptoms you have to deal with afterward.
Suggesting activities that better fit your needs doesn’t make you a burden. It doesn’t make you “complicated” or “too much.” It’s easy to forget that other people may say no to hikes or sitting out in hot, sweaty temperatures simply because they don’t enjoy those activities, and that’s OK. Don’t worry about saying “no”: Advocating for yourself and putting your needs first is important because nobody knows your body better than you.
Try getting creative with plans and try some of these HS-friendly activities:
- Netflix watch parties
- Indoor “camp-outs” with s’mores from the oven
- Video game competitions — who is the family champion?
Dating With Hidradenitis Suppurativa
Intimacy with hidradenitis suppurativa can be difficult. First, you may be wondering about the logistics: Can you be intimate without causing flare-ups or increasing your pain? You may be wondering what a partner will think about your HS. Will they think it’s “gross?” Will you still feel sexy around your partner during a flare? HS commonly occurs for the first time in young adults, so you may be terrified of navigating the dating world for the first time on top of your HS.
To get insight into how others have navigated intimacy, we interviewed Mighty contributor Kashinda Marche on dating with HS. Her main piece of advice? Communication is key:
“When living with HS, you’ve got to let your partner know. Because if they know what’s going on with your body, and they love you, they will work with you to do whatever it takes so that they’re not hurting you.”
By talking with a partner openly about what you’re going through, you can make sure both of your needs are met:
“[Telling them about HS is important] so that they can feel safe because there’s this myth that HS is contagious. [Hiding your HS] can also cause this massive guilt. If you communicate well, you can also relieve yourself of the guilt.”
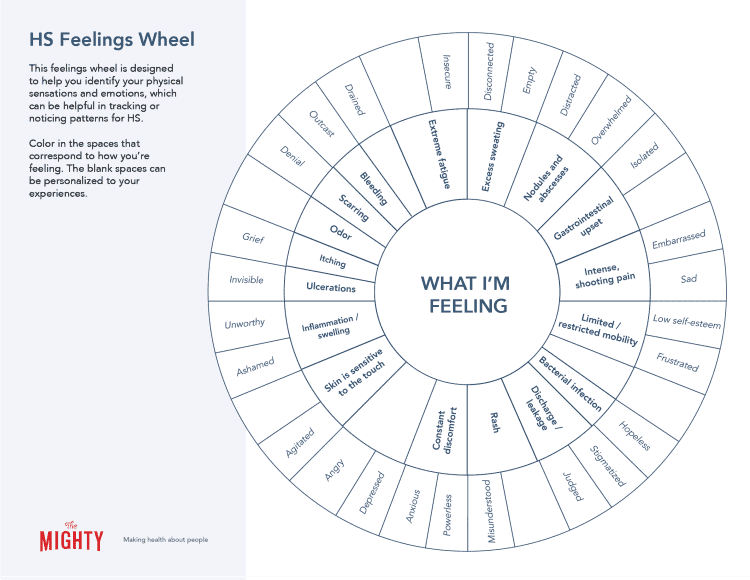
Talking about embarrassing symptoms and what emotions you’re feeling can be challenging. But if you’re comfortable, a visual aid can serve as a good starting point. The HS Feelings Wheel below can help you (and maybe even those you care about) connect the dots between the emotions and physical symptoms you’re experiencing, without you having to say a word.
Remember this: Your loved ones care about you. It may be hard to “break the ice” about HS at first, but they can become your biggest ally and advocate.
You can read more about how other Mighties have navigated relationships with HS here:
- How I Describe Hidradenitis Suppurativa to My Friends
- The Challenges I Face At Work As Someone With Hidradenitis Suppurativa
- Dating Someone With Hidradenitis Suppurativa
If you’re having trouble navigating anxiety around intimacy, you can also find resources and counseling from the American association of sexuality educators, counselors and therapists.

How To Support Someone Living With Hidradenitis Suppurativa
It can be challenging to support someone with a condition you haven’t heard of before or don’t really understand. You may find yourself asking, “What is hidradenitis suppurativa?” As you search to understand, remember this: the journey and the willingness to understand are what matters most. You don’t have to know all the tiny details about a condition to be part of someone’s support system.
Being supportive starts with transparent communication, having an open mind and being present. If you’re wondering how to put that into words, Mighty contributor Kashinda Marche said it best:
“Be honest and say, ‘Listen, I don’t know much about HS. It looks like it’s pretty heavy. But I’m here. I’m here to listen, if you want to talk about it, you could tell me whatever. I left my judgment at the door. And if you don’t know a lot about it, then I’m here for you. Let’s learn about it together. How do you want to do this?’”
Often, it’s the little things that can make all the difference. Here’s what helps Mighty contributor Allyson Byers:
“I really love it when somebody texts to check in or just gives me a call. Sometimes, [it’s as simple as] ‘how are you?’ It’s so easy to isolate yourself and to feel like I’m just gonna go through this flare-up or this pain by myself. And so having someone reach out makes you feel really like people are thinking about me, even if I haven’t been able to hang out with them or go do things.”
What many people may not understand about HS is how much of an impact it can have on day-to-day activities, like going to the grocery store, cleaning the house or picking up prescriptions. HS can be very painful, so offering practical help can be incredibly helpful.
To learn more about the experiences of others living with HS and how to support them, check out these Mighty stories:
- 4 Ways to Ask for Support During an HS Flare
- What Self-Care Looks Like With Hidradenitis Suppurativa
- 5 Lessons I’ve Learned About Dealing With a Chronic Illness in the Workplace
Learn More About Hidradenitis Suppurativa (HS)
If you’d like to learn more about HS and download some actionable resources, check out The Mighty’s Digital Toolkit for Living With Hidradenitis Suppurativa.
This toolkit includes:
- 2 mini Mighty Guides for taking care of yourself and boosting your self-esteem
- A printable worksheet to help explain your experience with HS to others
- An HS flare tracker (great for doctor’s appointments!)
- Instructions for how to make a hot or cold compress to ease the pain
- 6 printable (and digital!) coupons to give to your loved ones when you need support
- 2 cards you can color in and send to a friend, family member or yourself
- 4 affirmations for tough days with HS from people who’ve been there (print or save them to your phone/desktop)
This condition guide was created with support from many Mighty contributors and medical experts. You can learn more about the individuals interviewed for the creation of this resource here:
- Amit Garg, M.D.
- Chris Sayed, M.D.
- Allyson Byers, Mighty contributor
- Kashinda Marche, Mighty contributor
- Carla Lohr, Mighty staff member
And to the 42 Mighties who took our HS survey: thank you!
1Saunte, D., & Jemec, G. (2017). Hidradenitis Suppurativa: Advances in Diagnosis and Treatment. JAMA, 318(20), 2019–2032. https://doi.org/10.1001/jama.2017.16691
2Kerdel F. A. (2014). Current and emerging nonsurgical treatment options for hidradenitis suppurativa. Seminars in cutaneous medicine and surgery, 33(3 Suppl), S57–S59. https://doi.org/10.12788/j.sder.0094
3Margesson, L. J., & Danby, F. W. (2014). Hidradenitis suppurativa. Best Practice & Research Clinical Obstetrics & Gynaecology, 28(7), 1013-1027. doi:10.1016/j.bpobgyn.2014.07.012
4Napolitano, M., Megna, M., Timoshchuk, E. A., Patruno, C., Balato, N., Fabbrocini, G., & Monfrecola, G. (2017). Hidradenitis suppurativa: from pathogenesis to diagnosis and treatment. Clinical, cosmetic and investigational dermatology, 10, 105–115.https://doi.org/10.2147/CCID.S111019
5Assessment of familial risk in patients with hidradenitis suppurativa.
Bruinsma RL, Fajgenbaum K, Yang Y, Del Mar Melendez-Gonzalez M, Mohlke KL, Li Y, Sayed C.Br J Dermatol. 2020 Nov 5.
6Cartron, A., & Driscoll, M. S. (2019). Comorbidities of hidradenitis suppurativa: A review of the literature. International journal of women’s dermatology, 5(5), 330–334. https://doi.org/10.1016/j.ijwd.2019.06.026
7Micheletti R. G. (2014). Natural history, presentation, and diagnosis of hidradenitis suppurativa. Seminars in cutaneous medicine and surgery, 33(3 Suppl), S51–S53. https://doi.org/10.12788/j.sder.0092
8Kokolakis, G., Wolk, K., Schneider-Burrus, S., Kalus, S., Barbus, S., Gomis-Kleindienst, S., & Sabat, R. (2020). Delayed Diagnosis of Hidradenitis Suppurativa and Its Effect on Patients and Healthcare System. Dermatology (Basel, Switzerland), 236(5), 421–430. https://doi.org/10.1159/000508787
9Mayo Clinic. (2019, March 14). Metabolic syndrome – Symptoms and causes. https://www.mayoclinic.org/diseases-conditions/metabolic-syndrome/symptoms-causes/syc-20351916
10Daniel A. Gold, Virginia J. Reeder, Meredith G. Mahan, Iltefat H. Hamzavi,
The prevalence of metabolic syndrome in patients with hidradenitis suppurativa, Journal of the American Academy of Dermatology, Volume 70, Issue 4, 2014, Pages 699-703, ISSN 0190-9622, https://doi.org/10.1016/j.jaad.2013.11.014
11Garg, A., Neuren, E., & Strunk, A. (2018). Hidradenitis suppurativa is associated with polycystic ovary syndrome: a population-based analysis in the United States. Journal of Investigative Dermatology, 138(6), 1288-1292. “https://doi.org/10.1016/j.jid.2018.01.009
12Scheinfeld N. (2013). Hidradenitis suppurativa: A practical review of possible medical treatments based on over 350 hidradenitis patients. Dermatology online journal, 19(4), 1.
13Shuja, F., Chan, C. S., & Rosen, T. (2010). Biologic drugs for the treatment of hidradenitis suppurativa: an evidence-based review. Dermatologic clinics, 28(3), 511–523. https://doi.org/10.1016/j.det.2010.03.012
14Machado MO, Stergiopoulos V, Maes M, et al. Depression and Anxiety in Adults With Hidradenitis Suppurativa: A Systematic Review and Meta-analysis. JAMA Dermatol. 2019;155(8):939–945. doi:10.1001/jamadermatol.2019.0759
15Menderes, A., Sunay, O., Vayvada, H., & Yilmaz, M. (2010). Surgical management of hidradenitis suppurativa. International journal of medical sciences, 7(4), 240–247. https://doi.org/10.7150/ijms.7.240. Trigger Warning: Graphic Content.
16Azuse, E., RN, & Lloyd III, MD, FACS, W. C., MD, FACS. (2020, November 21). Are You a Candidate for Hidradenitis Suppurativa Surgery? Retrieved from https://www.healthgrades.com/right-care/hidradenitis-suppurativa/are-you-a-candidate-for-hidradenitis-suppurativa-surgery
17Onderdijk, A. J., van der Zee, H. H., Esmann, S., Lophaven, S., Dufour, D. N., Jemec, G. B., & Boer, J. (2013). Depression in patients with hidradenitis suppurativa. Journal of the European Academy of Dermatology and Venereology : JEADV, 27(4), 473–478. https://doi.org/10.1111/j.1468-3083.2012.04468.x
18Matusiak, L., Bieniek, A., & Szepietowski, J. C. (2010). Psychophysical aspects of hidradenitis suppurativa. Acta dermato-venereologica, 90(3), 264–268. https://doi.org/10.2340/00015555-0866
19Nguyen, T. V., Damiani, G., Orenstein, L., Hamzavi, I., & Jemec, G. B. (2020). Hidradenitis suppurativa: an update on epidemiology, phenotypes, diagnosis, pathogenesis, comorbidities and quality of life. Journal of the European Academy of Dermatology and Venereology : JEADV, 10.1111/jdv.16677. Advance online publication. https://doi.org/10.1111/jdv.16677
Check Out The Mighty’s Hidradenitis Suppurativa Topic Page!
If you live with hidradenitis suppurativa and want to connect with other Mighties who’ve been there, check out The Mighty’s HS topic page. Join the conversation around HS, learn more about HS resources and become part of a family who gets it.