The Mighty's ER-positive/HER2-negative Metastatic Breast Cancer Condition Guide
The Mighty’s educational content combines the expertise of both the medical and patient community to support you and your loved ones through your health journeys. For this ER+/HER2- Metastatic Breast Cancer condition guide, we talked with a breast cancer expert, read the latest studies, and connected with more than 160 people living with breast cancer, and caregivers.
ER-positive/HER2-negative Metastatic Breast Cancer at a Glance:
- ER-positive/HER2-negative metastatic breast cancer is a specific type of breast cancer and has spread to other areas of the body (i.e., metastatic breast cancer).
- Breast cancer is the most common form of cancer diagnosed in women, and approximately 87% of all breast cancers are ER-positive/HER2-negative.
- ER-positive/HER2-negative breast cancer is the most common form of breast cancer, and luckily, has many different treatment options available for individuals diagnosed with this type of breast cancer.
Medically reviewed by Dr. Rani Bansal, M.D.

What Is ER+/HER2- Metastatic Breast Cancer? | Managing ER+/HER2- Breast Cancer | Common Breast Cancer Misconceptions | Mental Health and Metastatic Breast Cancer | How To Talk To Others About Metastatic Breast Cancer | How To Support Someone Living With Breast Cancer

What Is ER+/HER2- Metastatic Breast Cancer?
ER-positive/HER2-negative (ER+/HER2-) metastatic breast cancer is a specific subtype of cancer that originates in the breast tissue that has spread, or metastasized, to other parts of the body. ER+/HER2- breast cancer is the most common, accounting for approximately 87% of all breast cancers, and some individuals diagnosed with this type of cancer will also be diagnosed with metastatic breast cancer depending on how much it has grown or spread. Understanding what type of breast cancer you have specifically is important to receiving the best treatment. To help you better understand ER+/HER2- metastatic breast cancer, we’ve created this condition guide. Before we get into the details of this condition, we’re going to take a step back and provide you with an overview of what the “ER+/HER2-” means in your diagnosis and discuss some more aspects of breast cancer as a whole you should know about. Ready? Let’s get started.
What Is Breast Cancer Typing?
When a physician suspects you may have cancer, they will order a series of tests to determine what type of cancer you have. You could have a room full of individuals diagnosed with breast cancer and each cancer could be different. That’s why it’s so important to determine what kind of breast cancer you have, as treatments will vary heavily based on your results.
Some methods for determining breast cancer type include:
- Biopsy: This procedure is used to take a small sample of tissue from your body to be evaluated by a pathologist, a physician who specializes in visualizing the body and tissue samples.
- Immunohistochemistry (IHC) testing: This test is used on the breast cancer cells from your biopsy to determine if the breast cancer cells have increased number of HER2 and hormone receptors (such as estrogen or progesterone). This test uses chemical stains to see what type of receptors you have and relatively how many. For HER2 typing, test results will be either HER2-positive, negative, or borderline. For hormone typing, this test will see if your cells have receptors for progesterone and/or estrogen, which can act like “fuel” for certain types of breast cancer. A test positive for hormone receptors would be called “ER-positive.”
- Fluorescence in situ hybridization (FISH) test: This test uses special imaging techniques to determine if a biopsy contains the abnormal HER2 gene that causes the cell to produce too many HER2 receptors.
- Other screening, diagnostic, and monitoring tests that may be used to help determine the stage, type, or even presence of cancer include mammograms, thermograms, CT scans, bone scans, MRI scans, and more. You can learn more about the tests and screens you may encounter here.
Breast cancer typing will determine if the cancerous cells taken from the biopsy are one of the following four major breast cancer subtypes:
- HR+/HER2-
-
- Individuals with this subtype will be positive for hormone receptors (estrogen and/or progesterone) and are negative for higher-than-normal levels of HER2 receptors.
- HR-/HER2-
-
- Individuals with this subtype lack both hormone receptors and higher levels of HER2 receptors. This subtype is also known as triple negative breast cancer (TNBC).
- HR+/HER2+
-
- Individuals with this subtype will be positive for both hormone receptors and higher levels of HER2 receptors.
- HR-/HER2+
-
- Individuals with this subtype lack hormone receptors but have higher levels of HER2 receptors.
Having hormone receptors present for estrogen and/or progesterone makes these cancer subtypes more susceptible to estrogen and/or progesterone to fuel the cancer cells. We’ll take a deeper dive into what this means for your diagnosis. Read on for more!
What Are “Receptors” on Cancer Cells?
Cells are the building blocks that create tissues and organs. If you think about all of the “machinery” needed to accomplish this feat, you’ll soon realize that cells need to have messages or signals to know what to do. Cancer cells receive many different signals to grow and one type of signal comes from tiny receptors on the cell. Receptors are areas on the outside of the cell that receive these messages or signals and relay them to the inside of the cell. The number and type of receptor your cells have will help determine what kind of actions the cell will do, such as grow or replicate. That’s why understanding what type of receptors your cancerous cells have is so important – many cancer treatments target receptors to help reduce or stop the cancerous cells from receiving signals to grow.
With that in mind, what does ER+/HER2- mean? Breast cancer is very complex and is generally categorized in part by the type of receptors that are present on the cancer cell. When categorizing based on receptor type, breast cancers first are named by whether or not the cancer cells have receptors for hormones like progesterone or estrogen and then whether or not the cells have receptors for HER2. That’s why ER+/HER2- breast cancer is characterized by receptors that can interact with estrogen and at the same time, does not have receptors for HER2. Read on to learn more about these specific receptor types.
What Are Hormone Receptors?
Hormones are powerful messengers throughout the body, and play a key role in proper functioning of multiple body systems. However, these special molecules can also help cancer cells grow if there are too many or faulty receptors for hormones such as progesterone and estrogen on cancer cells. You’ve likely heard of the hormones progesterone and estrogen. While these hormones are present in those assigned male and female at birth, progesterone and estrogen are the dominant hormones that help regulate breast development, menstruation, and help support pregnancy.
Breast cancer that is ER+ is considered hormone receptor positive for estrogen. That means there are too many estrogen receptors on the cancerous cells and give them too many signals to grow when estrogen molecules fit into its receptor on a cell. Cancerous cells may also be progesterone receptor positive, which means that there are too many receptors for progesterone on the cancer cells. Many breast cancers will be positive for estrogen receptors, progesterone receptors, or both. Luckily, cancer treatments have been developed to help block these receptors or reduce the amount of hormone produced in the body. By doing so, these treatments will make it more difficult for the cancer cells to receive signals and will reduce their ability to grow.
What Are HER2 Receptors?
Like hormone receptors, HER2 receptors are also specialized areas on cells that are ready to receive signals and other messages. HER2 stands for “human epidermal growth factor receptor 2,” which is a gene in your cell’s DNA that creates these receptors. When you have a cancer biopsy, pathologists will determine whether or not these cells have an abnormal version of this gene.
In a healthy cell, HER2 receptors help your cells grow, divide, and repair themselves. Those who are HER2-positive have the abnormal gene, which creates extra receptors. That’s why having too many of these types of receptors can cause your cells to grow and divide too rapidly and become cancerous.
Unfortunately, having extra HER2 receptors on your cancer cells, or being “HER2+,” can make your specific type of breast cancer grow more rapidly and be more aggressive than other subtypes. The good news, however, is that HER2+ cancer is a common subtype of breast cancer, accounting for nearly 15% of all breast cancer cases. Research over the past few years has made incredible advancements and there are treatments that now include HER2-specific targeted therapies.
Other HER subtypes also include HER2-negative, HER2 Low, and HER3.
What Is Metastatic Breast Cancer?
When you are diagnosed with breast cancer, your doctor will likely tell you what subtype of breast cancer you have (i.e. ER+/HER2-) along with the stage the cancer is at. Cancer stages help give you and the doctor a better idea of the severity of the breast cancer, and whether or not it has spread outside of your breast tissue or nearby lymph nodes. Typically, earlier stages of breast cancer occur when the cancer has not spread beyond the breast tissue, whereas later stages of cancer can include cancer growth outside of the breast tissue.
When your cancer originated in the breast tissues but has since spread to other areas of the body, you will likely receive a metastatic breast cancer diagnosis. Metastatic breast cancer is harder to treat than earlier stages because your physician will have to target many different areas at once. Individuals living with ER+/HER2- metastatic breast cancer are more likely to have cancer in these areas of the body outside of the breast tissue:
- Bones
- Liver
- Lungs
- Lymph nodes
If you or a loved one has been diagnosed with ER+/HER2- breast cancer, read on for more information on how to work with your physician to get the best treatment.

Managing ER+/HER2- Breast Cancer
Because breast cancer is different for everyone, you and your health care team will develop an individualized treatment plan which will be based upon the specific subtype of breast cancer you have, and what stage your cancer is at.
It can be scary to be diagnosed with metastatic cancer, but Dr. Rani Bansal, an oncologist from Duke University, wants you to know:
“You are not alone in your diagnosis journey. Your health care team will be with you every step of the way. Our goal is to create a treatment plan that is the best fit for you, so that you can be comfortable knowing you are receiving the best care possible.”
If you or a loved one has been diagnosed with ER+/HER2- breast cancer, know that being here and reading this condition guide is a great first step after receiving or expecting a diagnosis. Given continued advancements in cancer care, each patient’s specific treatment plan may be different. However, learning as much as you can about the different ways to treat this condition will give you further insight on your options and creating a health care team you trust is critical.
If you looked up breast cancer online after you received the diagnosis, you may be overwhelmed by what you have found. You may be asking yourself:
- What does treatment for ER+/HER2- breast cancer look like?
- How will breast cancer affect my day-to-day life?
- What is the prognosis for patients with ER+/HER2- breast cancer?
Some options that you may be recommended by your care team include pharmaceutical options, such as oral or infusion systemic therapy (i.e., chemotherapy, targeted therapy, or immunotherapy) radiation, surgical options, and self-care or non-pharmacological options.
Endocrine or “Hormone” Therapy
When diagnosed with a hormone receptor positive breast cancer, treatments that block hormones (i.e., estrogen or progesterone) may be offered to you. These highly-effective drugs are used to block how the hormone interacts with receptors and/or prevent the creation of these hormones in your body in the first place. These are usually the first line of treatment and may be used in combination with other therapies, such as targeted therapies, depending on your situation. There are many different types of hormone therapies, so some trial and error may be needed to see which one works best against your cancer.
Targeted Therapy
Targeted therapies are treatment options that target cancer cells, or specific parts of your body that help cancer cells grow, while keeping healthy cells mostly unaffected by the treatment. These targeted treatments may be used instead of chemotherapy in some individuals.
The most common targeted therapies used with hormone treatment for ER+ breast cancer are CDK 4/6 inhibitors. These are medications that target cellular growth. Cells have growth “checkpoints” they must overcome in order to continue growing and cancer cells can have defects in these checkpoints. That’s why CDK 4/6 inhibitors can be an effective treatment option for cancer, as they help prevent cells from growing too quickly.
Starting targeted therapies sometimes require additional tests to be done to determine what types of mutations or other aspects of your cancer exist, so that the best therapy can be determined for your specific cancer. For example, if you have a genetic mutation called BRCA 1 or BRCA 2, you may be eligible for therapies that prevent cancer cells from fixing their own damage.
Chemotherapy
Chemotherapy is a medical treatment that uses powerful drugs to target and kill cancer cells. This type of therapy is usually given over multiple sessions in cancer treatment clinics (also known as infusion centers) or in some cases can be given in pill form to take at home. Chemotherapy may be used to help slow down the growth of cancerous cells or to help shrink tumors.
While many people wonder if they’ll experience chemotherapy as part of their treatment for cancer, know that chemotherapy is not the first therapy typically used for ER+/HER2- breast cancer. However, if your breast cancer has stopped responding to hormone or targeted therapies, then your oncologist may recommend chemotherapy. The type and duration of chemotherapy for ER+/HER2- metastatic breast cancer is highly variable and depends on each individual. If you are offered chemotherapy as an option, it will be tailored to you by your oncologist.
Immunotherapy
Immunotherapy is a type of treatment that helps boost your body’s ability to “fight off” cancer cells with its own immune system. Cancers can occur when genetic mutations occur in a cell, which make it more challenging to turn off growth. Immunotherapies can help target specific “checkpoints” in growth, so that cancer cells have a reduced ability to grow “unchecked” in the body. Immunotherapy is not typically used in ER+/HER2- metastatic breast cancer; however, there may be certain situations when your oncologist would recommend it.
Radiation Therapy
Radiation therapy is a form of treatment that uses radiation (high beams of energy) to target specific areas of the body to kill cancer cells. Radiation therapy may be used to help reduce tumor sizes before surgical treatment or used after surgical treatment to prevent the recurrence of cancer. For individuals with metastatic breast cancer, radiation therapy is often used to help manage symptoms of pain or discomfort. This is termed “palliative radiation” as the goal of radiation is to palliate symptoms.
Surgical Treatment
Surgical treatments are used to physically remove tumors and other regions affected by cancer from the body. Surgical treatment could include a mastectomy (removal of the entire breast), lumpectomy (removal of a tumor), or even removal of other areas of the body that have become cancerous or may become cancerous like the lymph nodes. Surgical treatments are more often used in the localized treatment setting. In the metastatic setting, surgical treatments usually have less of a role but may be used in certain cases.
Combination Therapy
When you discuss treatment options for ER+/HER2- metastatic breast cancer, you will likely be prescribed a combination therapy. Combination therapy is when an oncologist uses different treatment options together to create the best possible outcome. Example combinations could include using endocrine therapy plus CDK4/6 inhibitors, oral chemotherapy, or other targeted therapies. There are now medications that have combined chemotherapy and targeted therapy drugs together to produce a stronger effect against cancer cells, which are called antibody drug conjugates (ADCs). Every person’s treatment regimen will be different depending on where the cancer has spread or how extensive it is, among many other factors.
Self-Care and Non-Pharmacological Options to Help Manage Living With Metastatic Breast Cancer
Metastatic breast cancer can have vast effects on the body. Treatments for breast cancer can be extensive, and each treatment has its own potential side effects. Your care team will help you manage those side effects as best as possible, but there are some strategies you can use to help make managing the process easier on your own.
Here are some tips community members suggested that might help:
- Massage therapy
- Meditation or deep breathing exercises
- Yoga
- Eating a healthy diet and exercising regularly
Some other aspects of living with breast cancer that you should consider include:
- Possibility of hair loss due to treatment
- Family planning and effects of treatment on fertility or ability to have children
- Mobility if treatment or cancer has affected your ability to walk or your energy levels
Living with any form of breast cancer can be a scary experience, but know that there are many people who have been through this experience – you are not alone! You can find support from others or find tips on speaking with your health care team on The Mighty’s breast cancer topic page. You can also read these stories about managing breast cancer on these great blogs:
What Does “Successful” Treatment for ER+/HER2- Metastatic Breast Cancer Look Like?
When receiving a cancer diagnosis, the first question that is often asked is around life expectancy and how likely you’ll be able to be cured from it. The answer to this question can be challenging, especially for metastatic breast cancer. Plus, every person’s cancer is unique so “typical” timelines may not be representative of your specific type of cancer.
ER+/HER2- metastatic breast cancer overall is considered incurable. However, there are many treatment options, and reaching remission or a place of stability with the cancer is possible if your particular cancer responds well to treatment. To learn more about ER+/HER2- metastatic breast cancer, we talked to Dr. Rani Bansal, an oncologist, about what she considers “success” in treatment for ER+/HER2- metastatic breast cancer. Here’s what she said:
“I want [my patients] to be able to live their life and be able to do everything that they want to do, and have that for as long as possible. Unfortunately, I can’t take their breast cancer 100% away, but I can try to get it to a point where it’s controlled, and it’s not affecting their everyday life. With ER+/HER2- metastatic breast cancer, many long-term treatment options are available in a pill form, so success could look like getting to a place where you manage your breast cancer through pills versus regular visits to treatment centers for therapy.”
If you’re feeling a little bit overwhelmed by your new diagnosis, that’s OK! Know that you have support available to you to help you along your cancer journey. Finding an oncologist you trust, and building a support team is the first step. You can read more about finding a doctor and who you might consider for your health care support team below.
How to Find a Doctor for ER+/HER2- Metastatic Breast Cancer
Finding the right care team can be challenging for any complex health condition, but it’s one of the most important steps you can take to managing metastatic breast cancer. The question you may be asking yourself is where to begin? Read on for advice from fellow Mighties!
First, find an oncologist (cancer specialist) and primary care physician you trust and feel comfortable with. Your oncologist and primary care physician can help you find the right specialists to help in your care. Know that you can “shop” around a little bit to find the right fit. If you don’t trust the doctors assigned to you, ask for a second opinion from someone else.
Different healthcare professionals can help manage ER+/HER2- metastatic breast cancer diagnosis, including:
- Primary care physician (PCP)
- Medical Oncologist
- Radiation Oncologist
- Surgical Oncologist
- Symptom Management/Palliative Care Physician
- Plastic surgeon, if you have surgical treatments
- Specialists associated with areas the cancer affects (i.e., a gastroenterologist if your metastatic cancer affects your GI system)
- Occupational therapist/physical therapist
- Mental health professional
In a recent survey of Mighty members, 76% of respondents said an oncologist helped them make a decision about treatment. Twenty-three percent said their primary care physician helped them as well. Together, these two professionals along with any others in your care team can help provide the best path forward in managing your ER+/HER2- metastatic breast cancer.
One Mighty Member shares her advice on where to start:
“When seeking a good doctor for cancer, start by researching and seeking recommendations from trusted sources such as primary care physicians, friends, and family members. Communication is key. Look for a doctor who is experienced in treating your specific type of cancer and who you feel comfortable communicating with.”
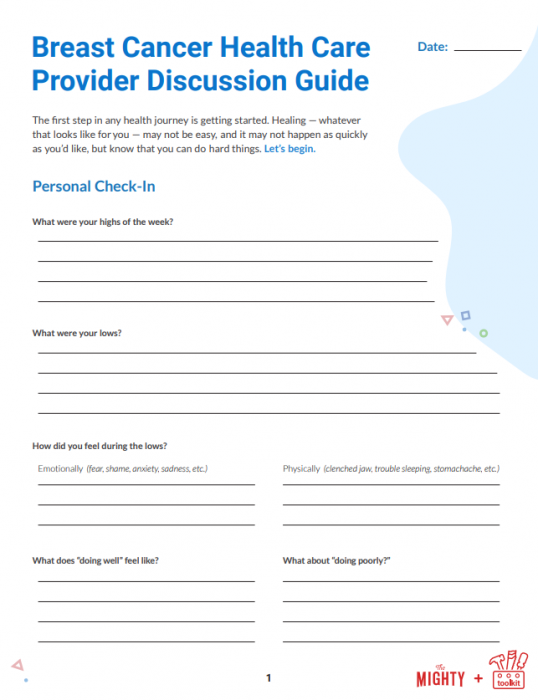
To help you navigate this journey, we created a downloadable discussion guide to help you prepare for a visit with your oncologist to help discuss your breast cancer diagnosis and next steps. We hope this guide helps you get the most out of your appointments:
It can be scary to receive any cancer diagnosis, and looking up treatments online can feel very daunting because of the volume of studies and potential therapies available. But don’t worry – that’s a good thing! There is a lot of research being conducted to help improve treatment outcomes for people living with cancer and your health care team will help you navigate it. You are not alone in this journey.
To learn more about ER+/HER2- metastatic breast cancer management, check out these resources:
Common Breast Cancer Misconceptions
Breast cancer is a well-known condition; however, there are still many misconceptions around breast cancer that can make life more challenging for those living with it. To better understand their lived experiences, we asked individuals living with breast cancer and their caregivers about what they wish others understood. Here’s what they had to say:
- “How lonely and frightening and overwhelming it can be, sometimes out of the blue. The mental health battle can be massive.”
- “Breast cancer doesn’t only happen in women. Men can get breast cancer too.”
- “Breast cancer can happen in young individuals too – it isn’t something that’s just restricted to older women.”
- “I wish people understood that just because you don’t have a history of breast cancer in your family, doesn’t mean that you are immune to it. Anyone can get breast cancer – it does not discriminate.”
- “I wish that they understood that breast cancer doesn’t end with treatment. Even after you are in remission, the effects of the cancer and cancer treatments linger both physically and mentally.”
- “The fear doesn’t end completely when you are in remission. Everytime you feel, or think you feel, a bump or lump, or some other symptom, the fear that the cancer has returned comes back in full-force. Annual scans to make sure you’re still in remission are terrifying because of this too.”
We hope that the words shared from the breast cancer community can help you better navigate and understand some of the challenges those living with breast cancer face. You may see your friend, family member, or community member look “fine” or “strong enough” to handle their journey with breast cancer. Just remember – they didn’t sign up to be strong, they had to be to survive, and that doesn’t mean they also don’t struggle at the same time with their cancer journey before, during, and even after treatment.

Mental Health and Metastatic Breast Cancer
It’s important not to overlook the impact breast cancer can have on your mental health.
In a survey of more than 160 people with breast cancer on The Mighty, 71% of respondents said that they experience depression or sadness, and 69% reported feeling anxiety or panic symptoms. Receiving a breast cancer diagnosis can be scary, and may surface many worries or fears for the future. Mental health is often overlooked in health care and isn’t often a core aspect of cancer treatment plans. This issue is highlighted in our survey, where 68% of all respondents said that the most difficult day-to-day challenge of living with breast cancer was actually the impact cancer had on their mental and emotional health, not the side effects of treatment.
Christina Bay, Mighty Member shares one of her mental health struggles with breast cancer:
“Cancer is time-specific. A lot of time is spent waiting. Waiting for results, waiting for tests, waiting until you can have treatment, waiting until you have recovered from one treatment to have the next treatment, waiting to heal from surgery, waiting for side effects to disappear. The list is endless. Waiting, as I’ve recently discovered, is daunting.”
If you are struggling with fear and the endless “waiting” as Christina described, read this advice from Ann Marie Giannino’s blog:
“Cancer is a life-threatening illness, it definitely messes with your head, not to mention your body and state of well-being. When I think of what helps me the most with my PTSD [from cancer] is sharing my fears with all of the incredible survivors that I have come to know through the internet, social media, support groups, friends of friends, etc. There are so many of us out there that have been through this and know exactly what the fear is all about. Support and a shoulder are huge for me. I know a lot of survivors that feel the same way. We help talk each other down from the ledge so to speak.”
If you are struggling with your mental health while living with breast cancer, know that mental health professionals are available. Seeking help does not make you less “strong,” it is simply an act of kindness to yourself, a way you can help yourself become stronger in different ways, not strong in the first place. You may be thinking, “but I have cancer and my anxiety or depression is just around the cancer – how will a therapist understand the experience?” Luckily, there are therapists and other mental health professionals who specialize in therapy for individuals who have experienced cancer.
It’s important to note that it’s OK if you’re still feeling anxious, depressed, or stressed even if you are in remission. You may still feel the effects of cancer on your mental health even after everything is “OK” with the cancer itself. Forty-two percent of individuals we surveyed stated that they had questions about support after treatment, especially around recurrence. Stress around scans is real and valid, and finding support can help with that process.
Other aspects of breast cancer that can impact your mental health are treatment-related side effects like fatigue, pain, and hair loss. Body image can be affected by hair loss and surgical treatment. Know that getting plastic surgery after treatment is something you can pursue – and not feel “weird” about! There are even plastic surgeons who specialize in options for breast reconstruction after cancer treatment.
It can be hard to be vulnerable, but opening up to your health care provider and a therapist is important. These conversations may give you coping strategies and treatment options to improve your quality of life.
If you’re looking for a breast cancer community check out these stories from fellow breast cancer advocates:
- PTCD – “Postraumatic Cancer Disorder”
- When I Took a Moment to Embrace My New Normal and Not Fear Cancer
How to Get Help in a Crisis
If you’re struggling with suicidal thoughts, know you are not alone. There is help for people who feel suicidal. If you need help right now, you can call the National Suicide Prevention Lifeline at 1-800-273-8255 or text “START” to 741-741. Head here for a list of crisis centers around the world and visit our suicide prevention resources.

How to Talk to Others About Metastatic Breast Cancer
Receiving a metastatic breast cancer diagnosis can be challenging for both you and your loved ones. There will be many concerns and everyone reacts differently to stressful situations. Some may be in disbelief, some may get easily frustrated during this time. One tool you can use is information about what to expect along this journey from your health care providers and other breast cancer advocates who have been there. By better understanding what you’re about to experience or currently experiencing together, you and your loved ones will be better equipped.
Although a journey with metastatic breast cancer can be challenging (you’re doing a great job, by the way), we hope this section can help you become more comfortable talking about what you’re going through with your loved ones, your doctors, or even with others living with breast cancer. No matter what, our Mighty community is here to help. We’ve got your back.
Being open about your needs and boundaries is important when talking about your journey with breast cancer. You may encounter people who don’t want to get involved because it’s “too personal,” but you really want the support. You may also find yourself in a difficult situation where a family member or friend wants you to participate in an activity that is more difficult because of your cancer or cancer treatment. For example, they may not know how much your treatment affects your energy levels or if certain activities are painful. It may be tempting to just “fake it ‘til you make it” for a while. But your energy is precious – take the rest you need. Yes, you can come first!
Karin Sieger shares these important words in her story on The Mighty:
“I was not brought up to put myself first. I was brought up to think of it as bad manners and selfish. The concepts of entitlement and even self-care did not exist in our vocabulary or in our family ethos. All my life I have been focused on being fair to others. But now I know I have learned very little about being fair to myself, and about protecting my own needs. Now I know that self care, pacing myself, and looking after myself is essential to my physical, mental, emotional and spiritual wellbeing.”
Being open with your family and friends about your limits and needs doesn’t make you “too much.” Saying “no” won’t make you a “worse” friend. Your group wants to be with you because of who you are. So be your own best advocate. After all, no one knows your body and its limits better than you do.
Try taking the lead and invite your group to a breast cancer-friendly activity:
- Organize a Netflix watch party
- Start a virtual book club with friends
- Organize a playdate for your children, so that they can be entertained while you and a friend do a calm activity like sitting outside listening to music or watching a movie
- Learn a new craft, especially one that can be done with a limited amount of energy
If you’re struggling at work, especially during treatment, know that there are options available to help through your employer’s human resources (HR) department. You may be eligible to go on short or long-term disability, or Family and Medical Leave (FMLA). Accommodations may be made to help you complete your work, such as working remotely, assistive devices if you experience pain, or different work hours to better accommodate your treatment schedule. You may also be able to access free mental health resources with your employer’s health insurance plan or HR benefits.
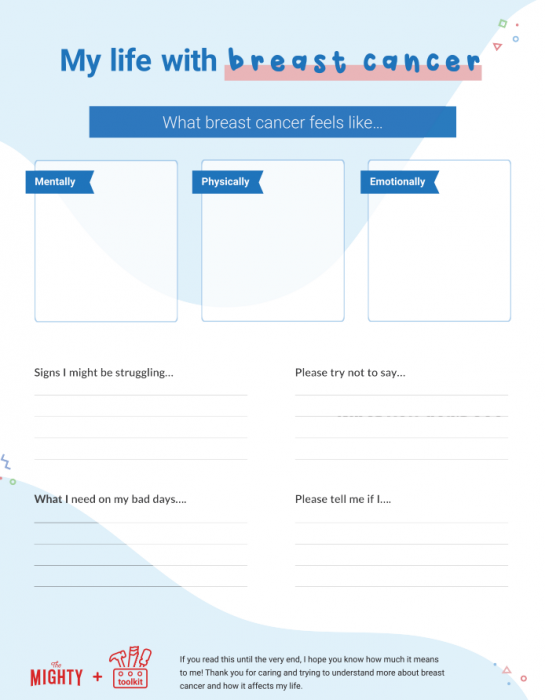
We know it can be tough to communicate your needs and experiences with people in your support system (especially on rough health days), so we created the worksheet below for you to fill out when you’re feeling up to it. Share it with those who are eager to learn more about what you go through with metastatic breast cancer. We hope this can be a bridge to better communication for everyone. You all deserve it.
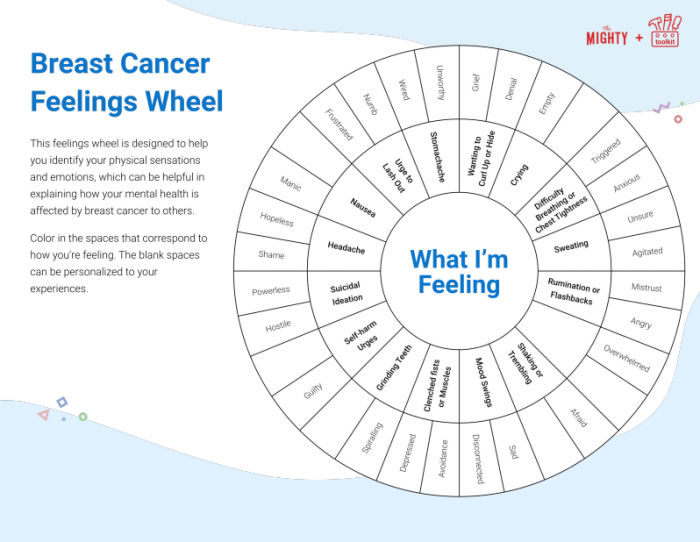
We also created this Mighty feelings wheel with common physical sensations and emotions. It’s a great visual tool for sharing with loved ones or someone on your treatment team. As a bonus, coloring in the sections that best match what you’re feeling can be a welcome distraction, too! We hope these tools can be a bridge to better communication for everyone. You all deserve it.

How to Support Someone Living With Breast Cancer
It can be challenging to support someone with breast cancer. It’s not that you don’t care for the person who has just received this life-changing diagnosis, but it can be difficult to figure out the best way for you to show support. Do you wear pink? Do you cook meals for them? Here’s the bottom line: Being present and willing to learn more about what they’re going through is what matters most. You don’t have to be an oncologist who specializes in breast cancer to be a key supporter for someone living with it.
The key to success is good, open communication paired with active listening. Don’t make assumptions about what they’re going through. Fifty-six percent of the individuals we surveyed about their experience with breast cancer said that connecting with friends and family helped support their mental health and journey with cancer. And that’s where you come in – ask them what would help them, and respect their answer. Maybe you’re the friend that’s in the “no cancer zone” that they can connect to without any mention of cancer, even if it’s just for five minutes. Perhaps you’re the one they have a separate text thread with where they can share their worries and fears without feeling like they’re being “too much.” Whatever it looks like with your friend, family member, or even community member, know that you’re a part of their support network.
You don’t have to be a specialist to help them along their journey, but becoming knowledgeable about the type of cancer and treatment they’re experiencing can help a lot. They may be overwhelmed and need some help researching options or organizing all of their information. Sixty-nine percent of our survey respondents said that spending time researching or gathering information on breast cancer was helpful to support their mental health and cancer journey. Just remember: if the person you’re trying to support doesn’t want to talk about their diagnosis in detail, don’t force it. Everyone will have their preferred way of navigating their journey with cancer.
We’ve offered you a few ways you can help show support in a good way, but what are some ways that may not be the best idea? In this article about his wife’s breast cancer journey, Keith Hardeman shared these tips on what to avoid when trying to support someone with breast cancer:
- Avoid suggesting how people with breast cancer should feel or act. Each person’s journey is unique – let them experience their journey on their own terms.
- Be careful how you frame the journey. Sometimes positivity can be helpful, but don’t try to immediately turn crappy into happy every time.
- Think twice before inserting your faith. Some people lean on their faith when faced with a complex health condition like metastatic breast cancer, but others do not.
- People living with cancer do not need or want unsolicited treatment advice. Try and keep the special diets or “but this therapy worked for X” to yourself unless asked.
- When offering support, give something that is tangible.
Here are some suggestions the community highlighted:
- Offer to drive them to and from treatments
- Be a notetaker during doctor’s appointments
- Help with childcare
- Help find resources around cancer treatments and insurance costs
- If you’re a breast cancer survivor or are also undergoing treatment, share your experiences
- Assist with cleaning the house, washing clothes, or preparing meals, especially after treatment sessions
- If they ask, help find a mental health professional who can provide further support
Cancer treatment and beyond can be a long journey. Everyone’s experiences will be different but just reading this educational resource is a thoughtful first step. Thanks for being here.

This condition guide was created with support from many Mighty contributors and medical experts. You can learn more about the individuals interviewed for the creation of this resource here:
- Rani Bansal, M.D.
- Tammy Polo
- Lauren Rockwell, MSW
And to the Mighties who took our breast cancer survey: thank you!

Check Out The Mighty’s Metastatic Breast Cancer Topic Page!
If you live with metastatic breast cancer and want to connect with other Mighties who’ve been there, check out The Mighty’s metastatic breast cancer topic page. Join the conversation around metastatic breast cancer, learn more about resources, and become part of a family who gets it.

Sources
Breast cancer molecular types. City of Hope. Retrieved April 1, 2023, from https://www.cancercenter.com/cancer-types/breast-cancer/types/breast-cancer-molecular-types#:~:text=One%20in%20five%20invasive%20breast,receptor%202%20(HER2)%2Dpositive.
Breast Cancer – Metastatic: Types of Treatment. Cancer.Net. Retrieved April 1, 2023, from https://www.cancer.net/cancer-types/breast-cancer-metastatic/types-treatment#:~:text=Hormonal%20therapy%20is%20considered%20the,for%20treatment%20at%20any%20stage.
Cancer Stat Facts: Female Breast Cancer Subtypes. National Cancer Institute. Retrieved April 1, 2023, from https://seer.cancer.gov/statfacts/html/breast-subtypes.html.
Chemotherapy. Mayo Clinic. Retrieved April 1, 2023, from https://www.mayoclinic.org/tests-procedures/chemotherapy/about/pac-20385033.
Hormone receptors: estrogen and progesterone. BreastCancer.org. Retrieved April 1, 2023, from https://www.breastcancer.org/pathology-report/hormone-receptor-status.
Radiation therapy for breast cancer. Mayo Clinic. Retrieved April 1, 2023, from https://www.mayoclinic.org/tests-procedures/radiation-therapy-for-breast-cancer/about/pac-20384940.
Testing for HER2 status. BreastCancer.org. Retrieved April 1, 2023, from https://www.breastcancer.org/pathology-report/her2-status.