What Is Fibromyalgia?
Editor's Note
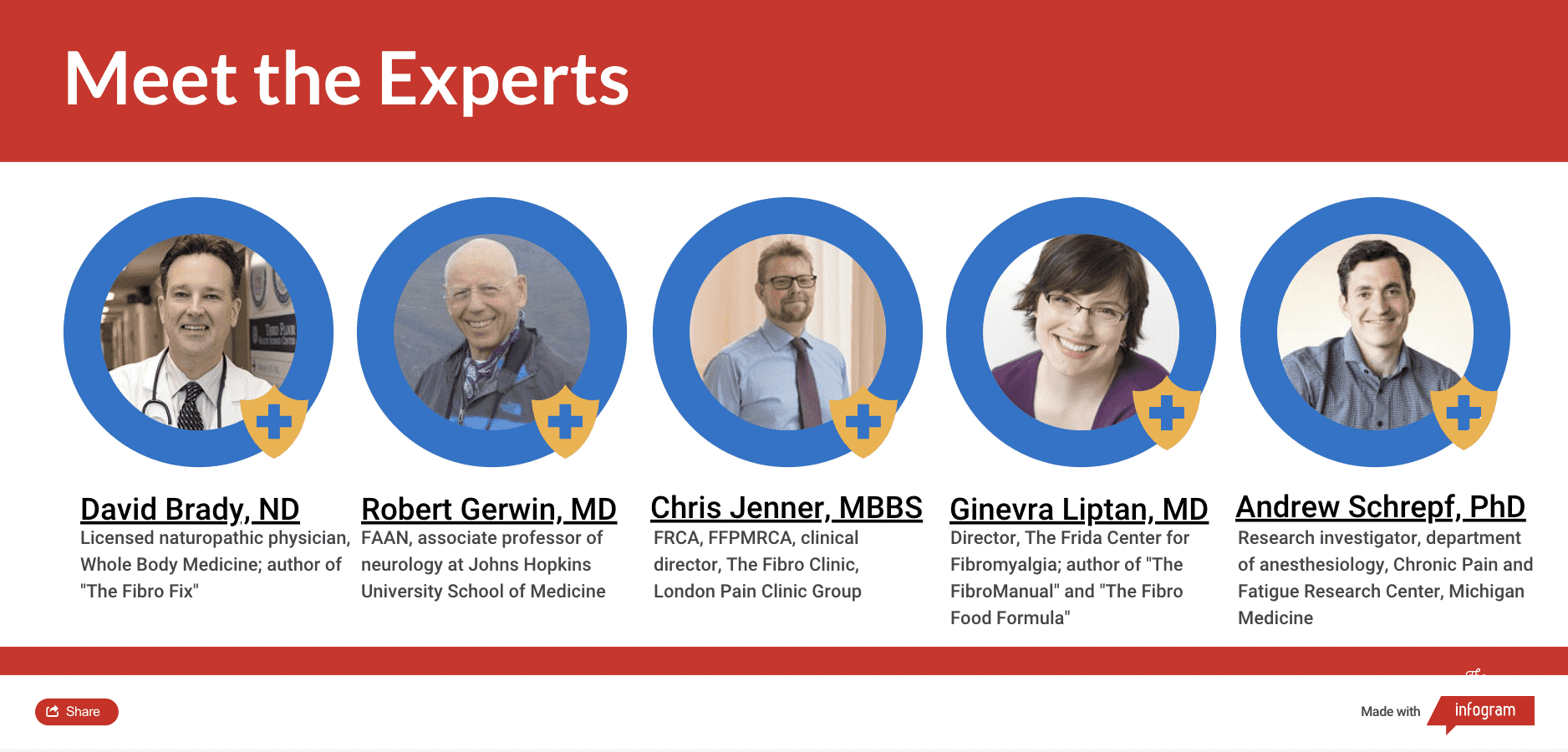
The Mighty’s Condition Guides combine the expertise of both the medical and patient community to help you and your loved ones on your health journeys. For the fibromyalgia guide, we interviewed five medical experts, read numerous studies and surveyed 13,997 people diagnosed with the condition. The guides are living documents and will be updated with new information as it becomes available.
Learn More About Fibromyalgia: Symptoms | Diagnosis | Treatment | Resources | Related Conditions

Medically reviewed by Emma Guymer, MBBS, FRACP
Who Gets Fibromyalgia? | Where Does Fibromyalgia Come From? | Long-Term Outlook
Ever feel like this? You have achy pain all over your body, especially in your muscles. When you sleep — whether it’s five hours or 14 — you never feel refreshed and you’re always tired. Sometimes you forget where you just put your keys or your brain is in a fog. You might feel worse in the morning, when it’s cold or when the weather changes. If this sounds familiar, you may have fibromyalgia, a chronic illness with three main symptoms — widespread pain, chronic fatigue and cognitive trouble.
Fibromyalgia is a complicated illness that’s not well understood. In the past, it was mischaracterized as a mental health disorder. Even today, some doctors wave off fibro symptoms as being “all in your head.” This isn’t the case. Fibromyalgia involves alterations in the function of your nervous system and how your brain processes pain. It also causes a response in your hormone and immune systems that can lead to many different changes, including neuroinflammation or inflammation in the tissues in your nervous system.
Many doctors refer to fibromyalgia as a “hypervigilant” or “fight-or-flight” illness because your nervous system stays in alarm mode all the time. If someone in your family has fibromyalgia, you’re more likely to have it. If you’ve experienced trauma, such as sexual or physical abuse, a bad car accident or combat, you also have a higher chance of developing fibromyalgia.
It’s common to have fibromyalgia and other chronic conditions as well as mental illness, though fibromyalgia is not a mental health condition itself. These conditions could include:
- Irritable bowel syndrome (IBS)
- Chronic fatigue syndrome
- Migraine
- Irritable bladder syndrome
- Lyme disease
- Lupus
- Rheumatoid arthritis.
- Post-traumatic stress disorder (PTSD)
- Depression
- Anxiety disorders
Currently, there is no cure for fibromyalgia. Though fibromyalgia can be debilitating, there are many treatments to try. These might include:
- Medications
- Exercise programs
- Pain management regiments
- Cognitive-behavioral therapy (CBT)
- Natural and integrative medicine therapies
- Lifestyle changes
It can take a while to find a combination of treatments that help. Researchers are working to find the cause of fibromyalgia, a potential cure and additional treatment options.

Who Gets Fibromyalgia?
An estimated 3 to 6 percent of the U.S. population lives with fibromyalgia, and it’s considered the most common chronic pain condition.9 Fibro is twice as common in those born female.10 Doctors believe women get fibromyalgia more often because of the construction of their nervous system. Male and female nervous systems operate differently because of the variations in male and female genes.2
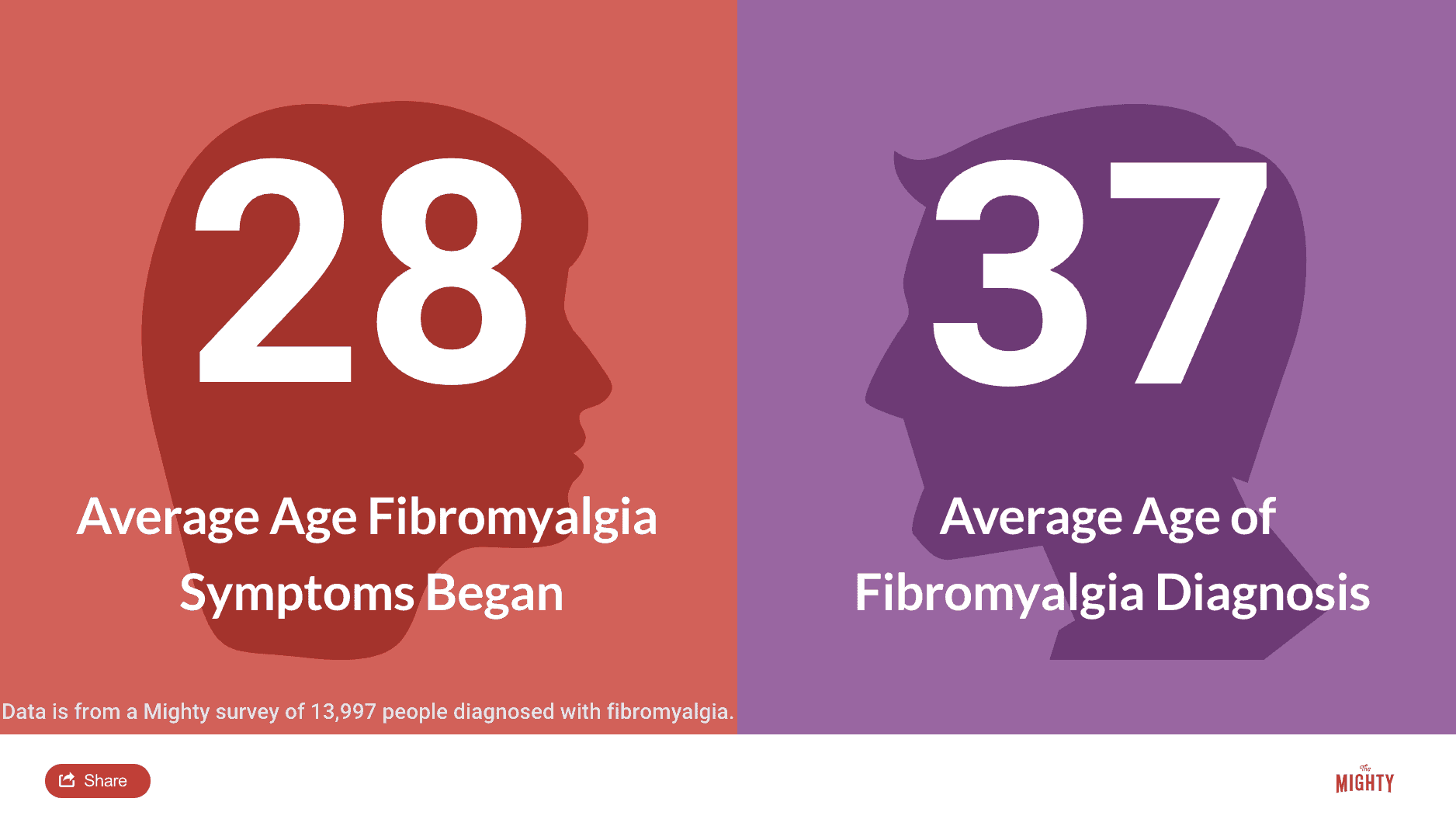
People of all ages can get fibromyalgia. However, fibromyalgia is most common among young adults in their 20s and 30s. Today, doctors more frequently make the diagnosis in teenagers, but many still go undiagnosed until much later.7 Fibromyalgia also occurs among all ethnic groups.
Where Does Fibromyalgia Come From?
We don’t know what exactly causes fibromyalgia. In the past, doctors found the symptoms of fibromyalgia mysterious — their patients didn’t look sick but they reported constant pain and fatigue. Doctors couldn’t find a source of the pain, so they dismissed their patients as having a mental health condition or said their symptoms were “all in their head.” Unfortunately, there are still doctors who may dismiss your symptoms because they don’t understand the latest research on the condition.
In their work to understand fibromyalgia, researchers first thought it was an autoimmune disorder. Autoimmune diseases occur when your body attacks healthy cells. However, that’s not what scientists observed in fibromyalgia. People with fibromyalgia had symptoms in their nervous system and their immune system that couldn’t be explained by any other chronic illness or mental illness. Fibromyalgia is best understood as a pain processing disorder in your nervous system caused by your fight-or-flight alarm system going off all the time. Fibromyalgia also impacts the immune system, and it is likely passed through families.
The Nervous System
Your nervous system, made up of several different systems, is a complex web that regulates the body’s functions. Fibromyalgia affects your autonomic nervous system. This controls the “automatic” functions in your body thanks to two separate branches — the sympathetic nervous system and parasympathetic nervous system.
Your parasympathetic system takes charge when you’re relaxed. Your muscles loosen up, the brain calms down and the digestive process begins. Your sympathetic nervous system revs up when it feels you are under attack. It activates your body’s fight-or-flight mode, tensing your muscles, pumping up your heart rate and increasing your attention and awareness.
When your hypothalamus, a part of the brain that coordinates your autonomic nervous system, senses danger, it sends a signal to the sympathetic nervous system to prepare the body to react: fight, flight or freeze. In a healthy nervous system, once the perceived threat ends, the hypothalamus signals the parasympathetic nervous system to take back over and calm the system back to a resting state. In fibromyalgia, however, your alarm system gets stuck in the “on” position.
Fibromyalgia causes you to stay in that hypervigilant state much longer than you’re supposed to. As a result, you experience chronic muscle tension (pain), trouble getting good sleep, issues with digestion and an overall sense of fatigue.7
In addition, fibromyalgia affects the complex systems in your brain that process pain. The systems in your spinal cord designed to reduce pain don’t work well if you have fibromyalgia, and the ones that amplify pain work overtime. Pain that wouldn’t bother most people is amplified when you have fibromyalgia.6 Scientists can see from neuroimaging brain scans that people with fibro process sensory information, especially pain, differently than the average person.10
Trauma
When you hear “fight-or-flight response,” your mind might automatically think of trauma. Many fibro patients report sexual or physical assault at some point in their life, often that happened during childhood. There’s also a strong overlap between fibromyalgia and the trauma-related mental illness post-traumatic stress disorder (PTSD). Nearly half of men diagnosed with combat-induced PTSD also meet the criteria for a fibromyalgia diagnosis.8
The link between trauma and fibro, however, isn’t so straightforward. Fibromyalgia tends to develop when you experience high amounts of psychological stress during trauma or a physical illness — and this is common in any traumatic situation. Fibromyalgia also can run in families (more on this later), which means your parents pass the genes on to you. However, having a gene for fibromyalgia doesn’t necessarily mean you will get the condition. You may never get fibromyalgia and never know you carry the gene. But if you have a gene, you have a much higher risk of developing the condition.
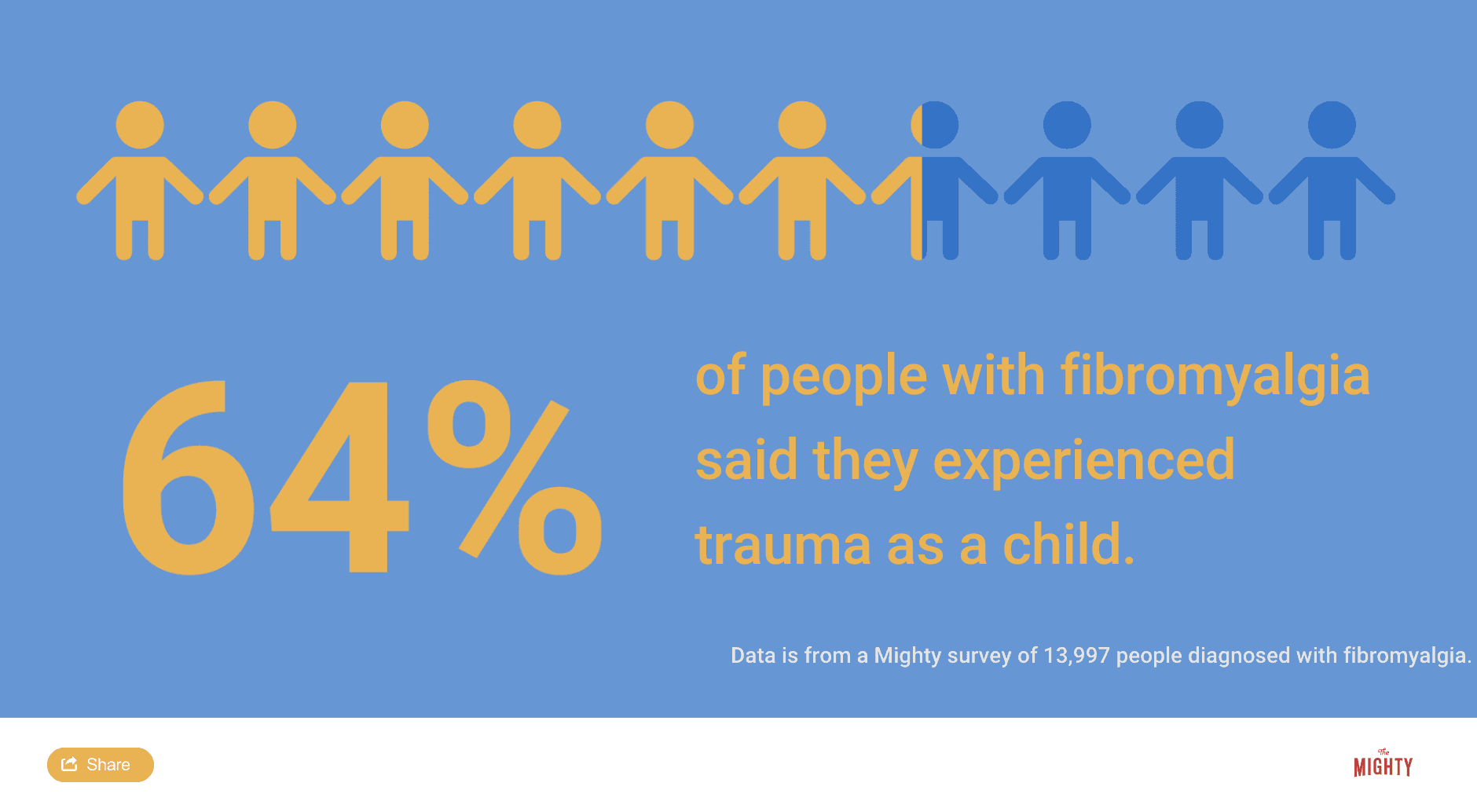
Trauma like abuse, wartime combat, a bad car accident or violence, can be enough to trigger your fibromyalgia. It’s like a one-two punch. You have a genetic predisposition for fibromyalgia. Then a trauma triggers the gene to express itself and you develop the condition. The timing of when you experience a trauma also seems to factor into whether you will get fibromyalgia, though it’s unclear why. Women who experience trauma in their adolescence seem particularly prone to having fibromyalgia.
Not everyone who has survived trauma will develop fibromyalgia, and you can still have fibromyalgia even if you can’t identify a traumatic experience in your life. Other incidents, like bad auto accidents where you experienced whiplash, have a strong connection to fibromyalgia. If you have another chronic illness, like Lyme disease or chronic fatigue syndrome, that can also trigger fibromyalgia.7
The Immune System
Fibromyalgia also affects your immune system. It’s not an autoimmune disorder — it doesn’t cause your body to attack healthy cells — but it does cause immune system dysregulation. When immune cells become inflamed, they send a signal that something is wrong in the body. With fibromyalgia, your inflammation signals aren’t firing right — they send the wrong signals at the wrong time to the wrong places. This is why sometimes, especially when your fibro flares, you feel achy like you have the flu. Researchers have confirmed that inflammation can occur in the brain and nervous system as well.1
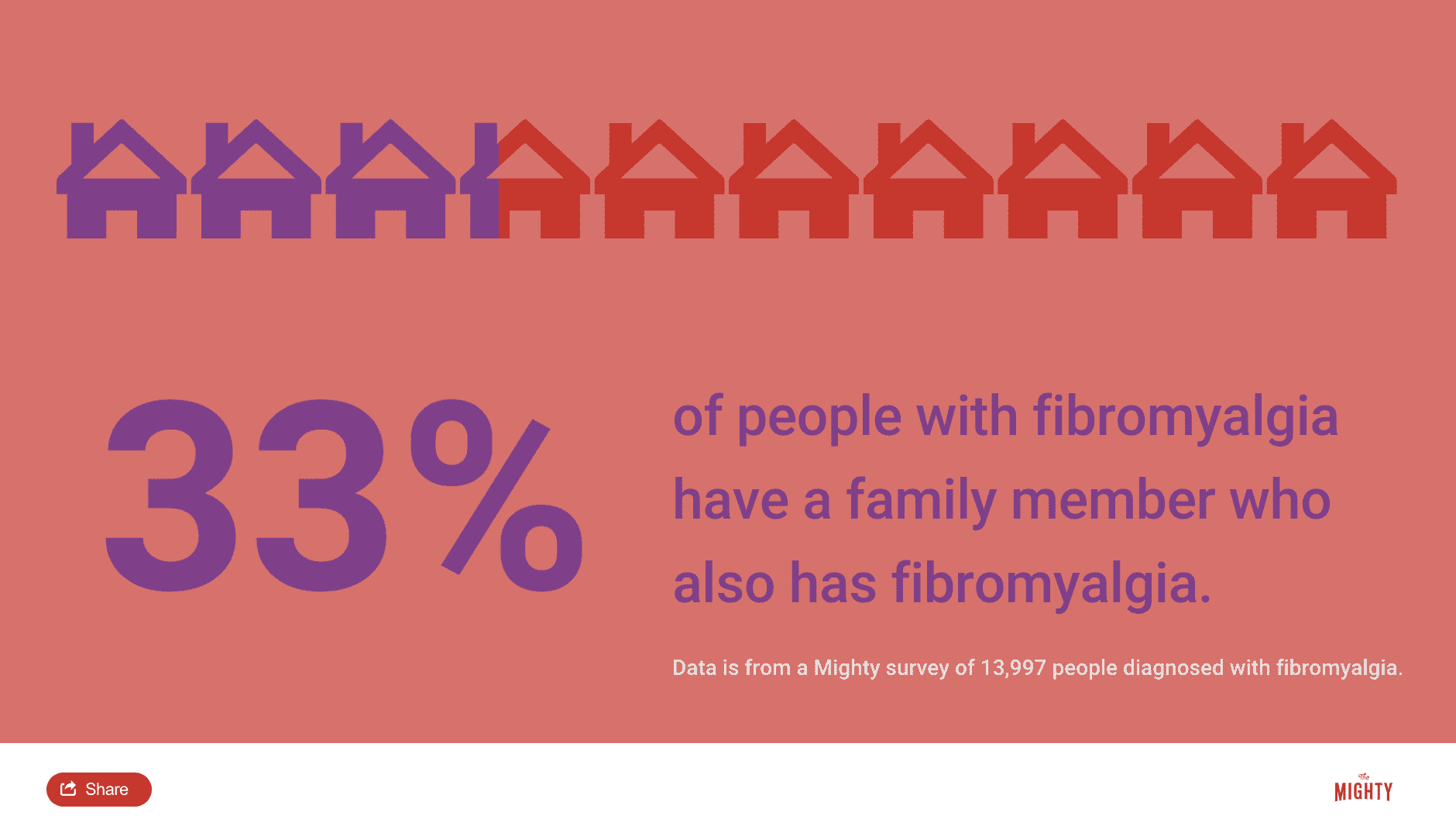
Genetic Causes
There’s evidence that fibromyalgia runs in families. If your parents, siblings or children have the condition, you’re more likely to be at risk. Researchers haven’t identified all the genetic markers linked to fibromyalgia yet, however, they have identified differences in genes linked to the pain control systems.
They have found that fibromyalgia patients often have a gene related to a dysfunctional enzyme — a substance in the body that facilitates chemical reactions between cells. This enzyme should break down the chemicals involved in the fight-or-flight process, but something goes awry when you have fibromyalgia. You’re also more likely to have genes programmed for abnormal receptors in the fight-or-flight or pain nerves.8
Other Research
Researchers continue to discover new information about fibromyalgia. For example, they’ve found that fibromyalgia could be related to an area of your brain called the default mode network (DMN). The DMN helps us reflect on our lives, and is typically most active when you’re at rest or daydreaming.
When you’re doing a goal-oriented cognitive task, the DMN is usually quieter. Using brain scans, researchers found that the DMN in patients with fibromyalgia seems to be online more than usual during cognitive tasks. It was caught communicating with the insula, another part of the brain that influences sensory processing like pain when it should be quiet.10

Long-Term Outlook
Fibromyalgia can be a serious illness. Many have such severe symptoms it impacts their ability to go to work or school or even complete basic tasks around the house. When you have fibromyalgia, you’re twice as likely to be hospitalized versus someone without the condition.3 Approximately 30 percent of those diagnosed with fibromyalgia qualify as disabled.4 Your experience may be different.
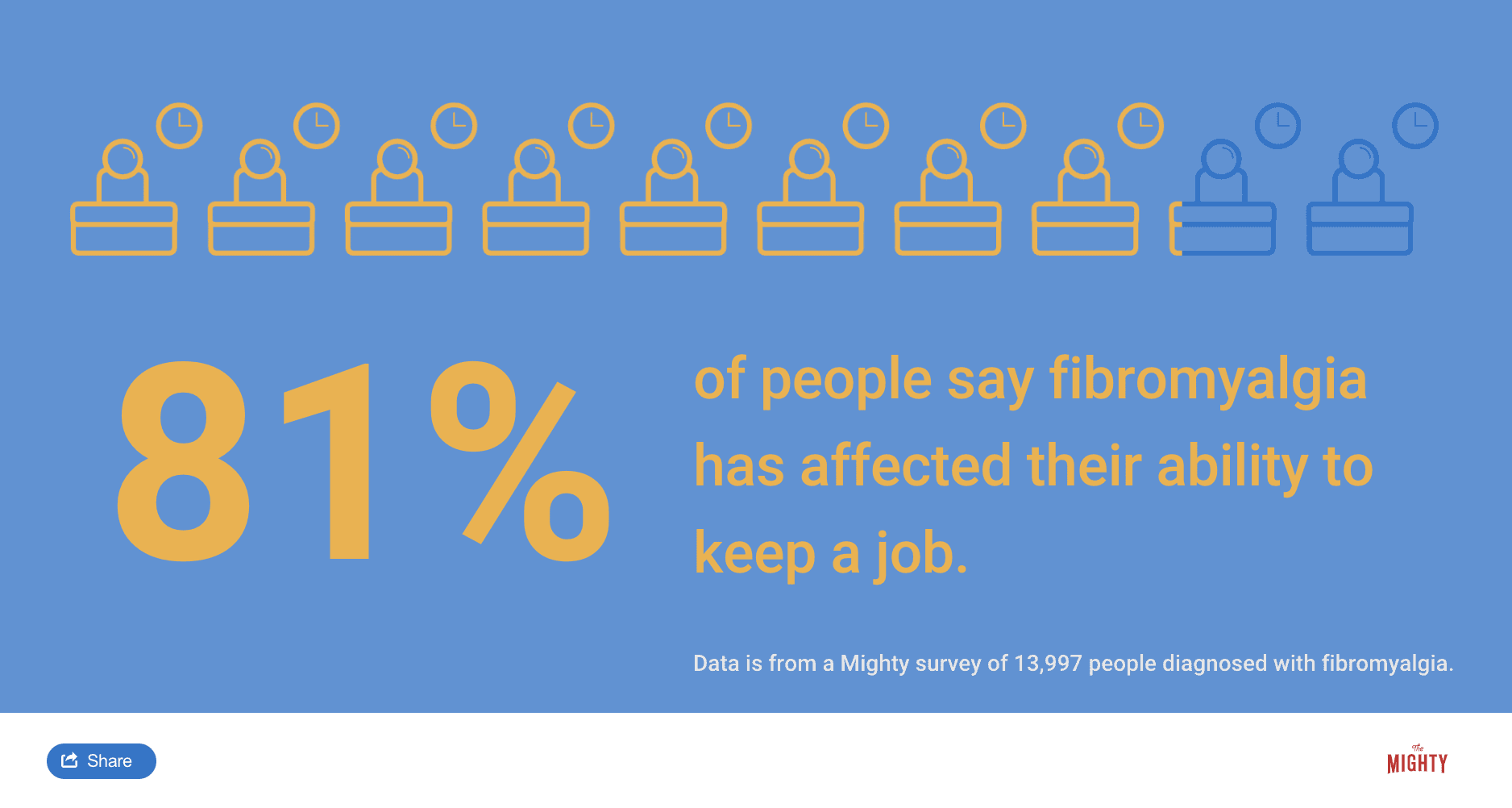
It can also be expensive and difficult to afford the care you need with fibromyalgia. Treating the disease often requires experimenting with different medications and doctors, which can be costly even if you have insurance. One 2007 study found that those with fibromyalgia typically spent between $100 to $1,000 a month out of pocket for medical costs related to the condition. Another study revealed that fibromyalgia patients paid nearly $1,500 for alternative treatments and spent a total of about $5,300 annually out of pocket for all medical expenses.4
Despite the lifelong challenges of living with fibromyalgia, it’s a misconception that nothing can be done to help. There are many treatment options for managing your symptoms even though it can be hard to find what will work for you. However, many people find they do better and experience some improvement or relief from their symptoms with the right combination of treatments.5 Fibromyalgia is a painful and frustrating condition, but there is hope.
Related: Here are some ways people describe what it’s like living with fibromyalgia.
- “To the Person Who Thinks My Fibromyalgia Isn’t Real“
- “A Typical 24 Hours With Fibromyalgia“
- “I’m Damned If I Do and Damned If I Don’t When It Comes to My Fibromyalgia“
Learn More About Fibromyalgia: Symptoms | Diagnosis | Treatment | Resources | Related Conditions
Last updated Dec. 12, 2019

Sources
- Albrecht, D. S., Forsberg, A., Sandström, A., Bergan, C., Kadetoff, D., Protsenko, E., . . . Loggia, M. L (2018). Brain glial activation in fibromyalgia – A multi-site positron emission tomography investigation. Brain, Behavior, and Immunity. doi:10.1016/j.bbi.2018.09.018
- Brady, D. (2018). Fibromyalgia [Telephone interview].
- Fibromyalgia | Arthritis | CDC. (2017). Retrieved from https://www.cdc.gov/arthritis/basics/fibromyalgia.htm
- Spaeth, M. (2009). Epidemiology, costs, and the economic burden of fibromyalgia. Arthritis Research & Therapy, 11(3), 117. https://doi.org/10.1186/ar2715
- Fitzcharles, M., Ste-Marie, P. A., Rampakakis, E., Sampalis, J. S., & Shir, Y. (2016). Disability in Fibromyalgia Associates with Symptom Severity and Occupation Characteristics. The Journal of Rheumatology,43(5), 931-936. doi:10.3899/jrheum.151041
- Gerwin, R. D. (2018). Fibromyalgia [Telephone interview].
- Liptan, G. (2018). Fibromyalgia [Telephone interview].
- Liptan, G. (2016). The fibromanual: A complete fibromyalgia treatment guide for you and your doctor. New York: Ballantine Books.
- National Fibromyalgia & Chronic Pain Association (NFMCPA). (n.d.). Retrieved from https://www.fmcpaware.org/
- Schrepf, A. (2018). Fibromyalgia [Telephone interview].

