What is rheumatoid arthritis?
Rheumatoid arthritis (RA) is an autoimmune disorder that causes inflammation throughout the body. This inflammatory disease causes the immune system to mistakenly attack the body and damage the joints, skin, eyes, lungs, heart, and vessels. Rheumatoid arthritis affects the lining of the joints and causes painful swelling that can lead to severe bone and joint problems.
What are the symptoms of rheumatoid arthritis?
Common signs and symptoms of RA include:
- Warm and swollen joints
- Stiffness in the joints
- Fatigue and loss of appetite
If you are experiencing early signs of rheumatoid arthritis, speak to your healthcare professional.
What causes rheumatoid arthritis?
It isn't entirely clear what starts the process of rheumatoid arthritis, but it is known that this is an autoimmune disease. The immune system protects your body against infection and sickness by attacking foreign substances like bacteria. In the case of autoimmune disease, the immune system instead attacks healthy tissues in the body. This is why rheumatoid arthritis can cause issues in other areas of the body outside of just the joints. Genes do not cause rheumatoid arthritis, but some genes can make it more likely that a person will react to environmental factors that could trigger the disease. Risk factors that make the disease more likely include: being a middle-aged woman, having a family history, smoking, and being overweight.
How do you treat rheumatoid arthritis?
Although there is no cure for rheumatoid arthritis, remission is possible with early treatment using disease-modifying antirheumatic drugs (DMARDs). Common medications for rheumatoid arthritis include NSAIDs such as ibuprofen, steroids, conventional DMARDs, biologic agents, and targeted synthetic DMARDs. Physical therapy and occupational therapy can also help individuals with joint flexibility and symptom management. Surgery to repair joints is an option for individuals who have not found success using medications and other interventions. Surgical procedures for rheumatoid arthritis include synovectomy, tendon repair, joint fusion, and total joint replacement. Opting for surgery may help you gain mobility back in your joints, but it carries risks with it as well.
The Power of Rheumatoid Arthritis Support Groups
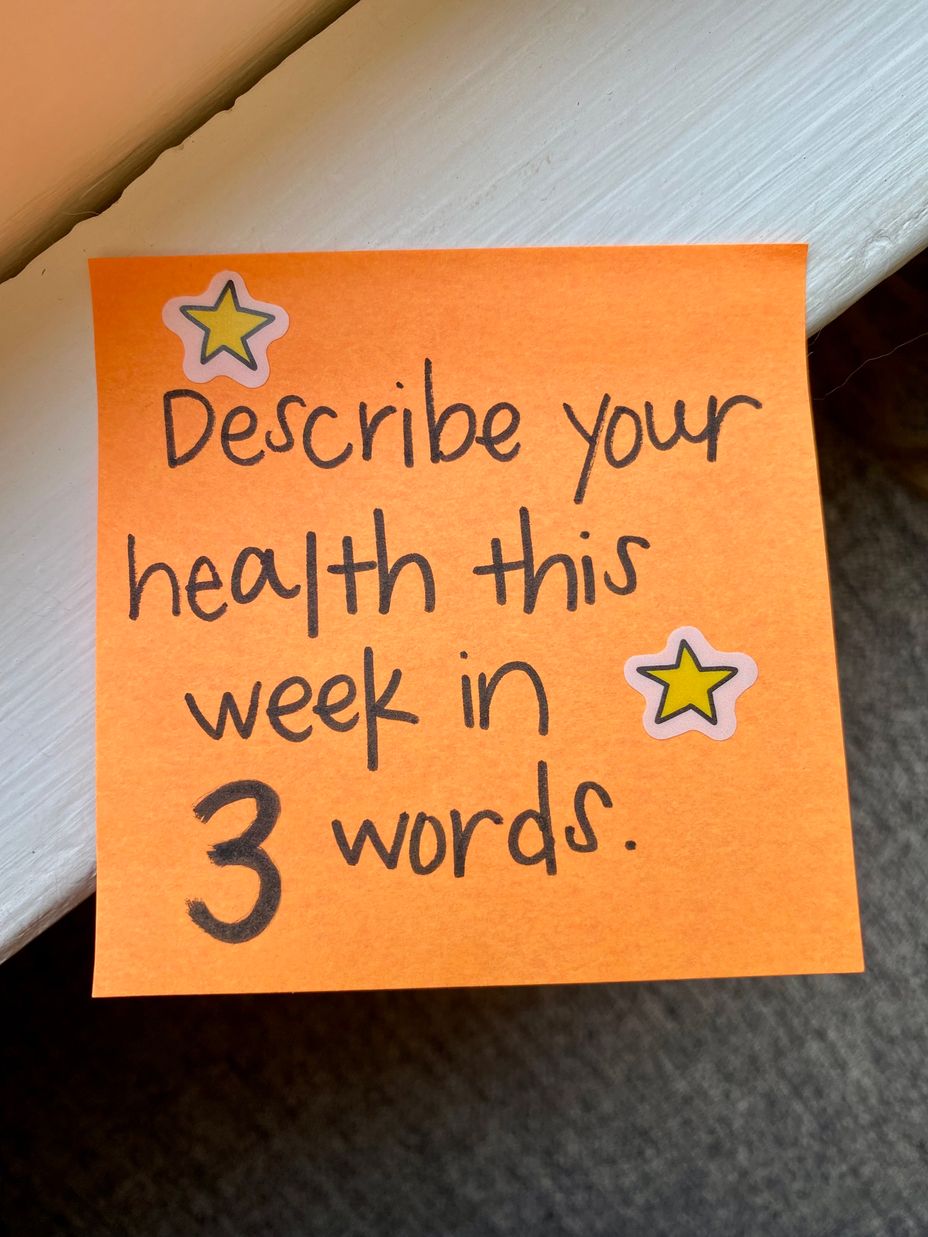
A rheumatoid arthritis diagnosis can result in feelings of isolation and loneliness. But with The Mighty, you’re never alone.
When you join our online rheumatoid arthritis support group, you’ll be connected with an extensive network of people who understand exactly what you’re going through. Our rheumatoid arthritis community has more than 150,000 members.
You’ll gain access to unlimited rheumatoid arthritis resources, including the latest news and medical research, tips for managing rheumatoid arthritis symptoms, and educational content that can help improve your day-to-day life.
Don’t let rheumatoid arthritis rule your life. Join The Mighty’s rheumatoid arthritis support group today.
Connections that Care
When you become part of our RA support group, you won’t just learn new coping strategies — you’ll find people who share your experience. Many of them have the same symptoms you do and are undergoing similar treatments.
As one of the largest rheumatoid arthritis support groups online, The Mighty’s platform acts as an open forum for people to ask questions, give advice, and share their stories. In addition to helpful tips on living with rheumatoid arthritis, our network of Mighty members can also help you find local social events in your area for additional support.
Join The Mighty’s rheumatoid arthritis support group and find your strength today.