Post-traumatic stress disorder (PTSD) and complex PTSD from emotional and psychological trauma are often considered invisible conditions. The invisible nature of these conditions can lead to being overlooked or under-considered when survivors visit general doctors and specialists who lag behind in trauma-informed practices. In addition to the effects of trauma itself, survivors are often stigmatized by those who mistakenly believe symptoms are “all in their head.”
Thanks to the work of researchers and professionals, however, great strides have been made in helping the public understand the physiology and neurobiology of trauma. Experts such as California’s Surgeon General Dr. Nadine Burke Harris and psychiatrist Dr. Bessel van der Kolk, among others, have linked the physical symptoms of emotional and psychological trauma.
When a survivor has been carrying the weight of an invisible illness, like PTSD or complex PTSD, it can be a great relief to discover there are tangible, measurable effects of trauma in the body. When survivors and their care teams are able to “see” the issue, it can often lead to more effective solutions for treatment.
Here are some ways you can “see” the effects of trauma:
1. In the Eyes
Cardiff University and Swansee University researchers recently released a study that looked at the pupils in the eyes of trauma survivors, which can be measured when shown images of stimuli. The pupils of trauma survivors showed an increased response when looking at both threatening and non-threatening images. In general, trauma survivors tend to take in more sensory information than the average population, which can often lead to a whole host of other issues, including overwhelm and fatigue. There is also a link between high-sensitivity and trauma.
2. In the Brain
Brain scans can reveal a number of insights as physical “proof” of trauma. In trauma survivors, it’s common for experts to observe a number of brain changes in several areas of the brain. An overactive amygdala, which controls the fight-flight response, means a survivor can be in a state of constant hypervigilance. A weakened prefrontal cortex (PFC) makes it difficult to concentrate, and an underactive anterior cingulate cortex (ACC) means emotional regulation is more difficult.
3. In the Body
In addition to psychological symptoms, including depression and anxiety, there are a number of physical ailments linked to trauma as well. Chronic fatigue, fibromyalgia, other autoimmune diseases, migraine, high blood pressure, night terrors, stomach ulcers, irritable bowel syndrome, and polycystic ovary syndrome (PCOS) seem to occur more often in trauma survivors.
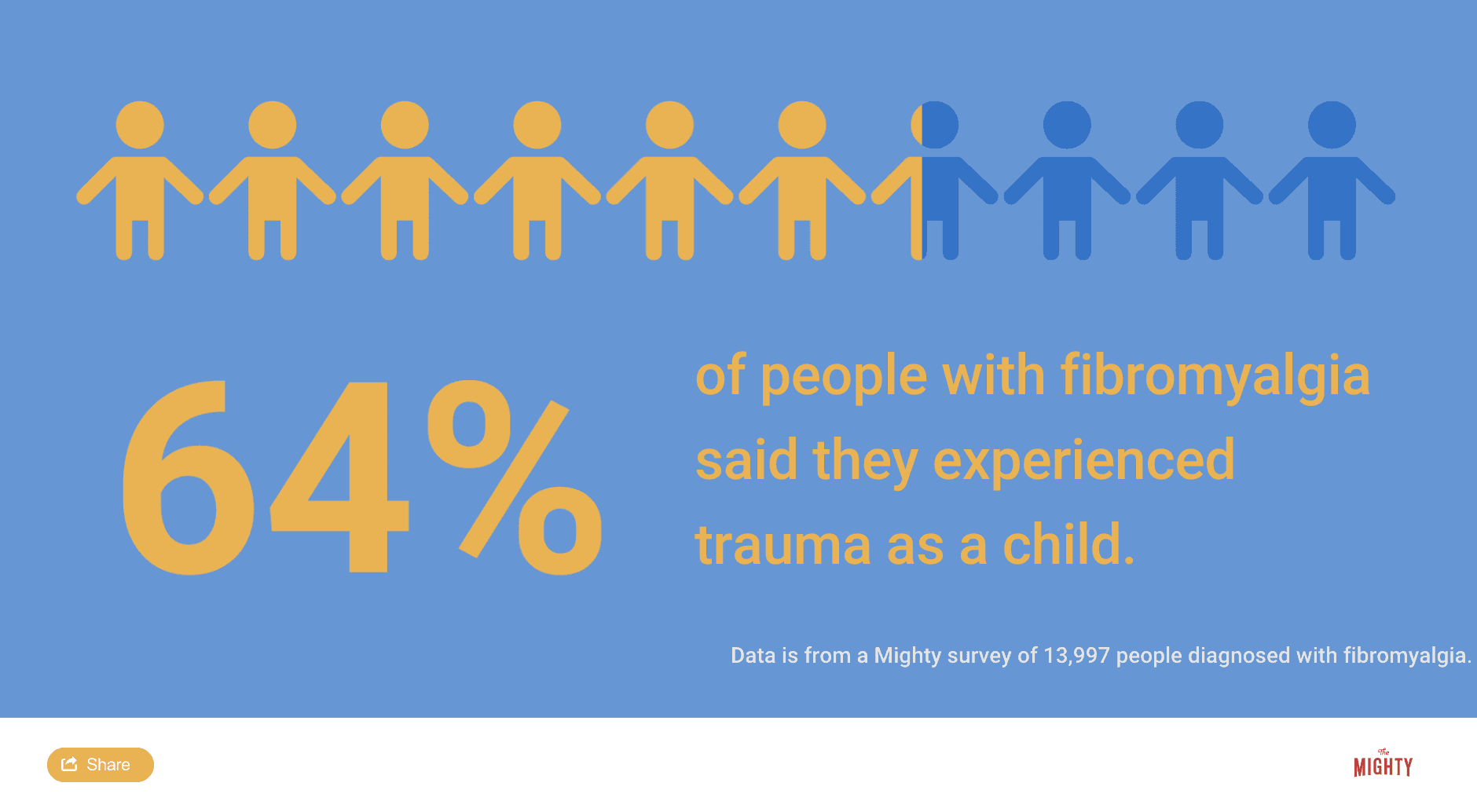
Trauma is one potential trigger of fibromyalgia, for example. It’s believed almost half of all men with combat-related PTSD also meet the criteria for fibromyalgia, a chronic illness that puts your nervous system into a hypervigilant state, causing chronic pain, fatigue and other symptoms. In addition, 64% of nearly 14,000 people diagnosed with fibromyalgia reported they experienced trauma as a child in a survey conducted by The Mighty.
Treating Physical Trauma Symptoms
While not all health issues are trauma-related, it is worth a deeper look at the root causes of these symptoms if you have a history of trauma. If you suspect trauma is an underlying cause of your physical ailments, it’s important to find health care professionals who are well-informed on the latest research on trauma-informed care.
Depending on where you live and your level of access to health care, you may need to search outside of your immediate area to find the right doctors or direct your health care team to further information to support you. The Adverse Childhood Experiences (ACEs) Study is a great place to start, and “The Body Keeps the Score” by Bessel van der Kolk is also an excellent resource to understand the connection between emotional trauma and physical pain.
Final Thoughts
Finding the right support for trauma recovery can be a harrowing experience on top of an already challenging condition. Trauma survivors often need a host of medical doctors, psychiatrists and therapists working in tandem to find the right solutions. Other “alternative” therapies, such as diet changes, massage, yoga, acupuncture or tai chi, may also be of benefit.
It can require a lot of patience and trial and error to find what works, but relief is possible. Often, the first step lies in acknowledging that the trauma is measurable and real.
Header image via UnitoneVector/Getty Images

