They say time heals all wounds.
But some moments don’t heal —
they settle inside you, quietly shaping who you become.
I was still young — fresh into my medical journey.
Bright eyes, trembling hands, a heart full of hope.
And then came her.
A beautiful, glowing woman —
Pregnant, with obstructive jaundice, but always smiling.
She had the kind of presence that lit up the room —
soft laughter, big dreams,
and a baby girl waiting to be born.
She talked about names, painted nurseries,
and worried about stretch marks and baby clothes —
not about dying.
But death doesn’t wait for permission.
It sneaks in —
even into labor rooms filled with new life.
It happened suddenly.
During delivery.
A blink.
A pause.
Then chaos.She collapsed.
We rushed — I remember barking out orders with a voice that didn’t even sound like mine.
My hands were trembling, my mind racing.
Pulmonary embolism.
We knew it was critical — and we fought.
God, we fought.
But medicine doesn’t always win.
And neither did we.
She died.
Her baby girl — stillborn.
Two lives…
Gone.
Just like that.
And outside that room —
was her son.
Six years old.
Wide-eyed.
Confused.
Then screaming.
Not because someone told him,
but because somehow —
he knew.
And her husband…
I will never forget the sound he made.
A sound that didn’t come from the throat,
but from the soul —
like something inside him had shattered and could never be put back.
That was my first death.
The first time I saw a life —
two lives —
slip away.
And it broke me.
But I didn’t have time to grieve.
There were more patients.
More tasks.
More faces waiting for the doctor with the steady hands and calm voice.
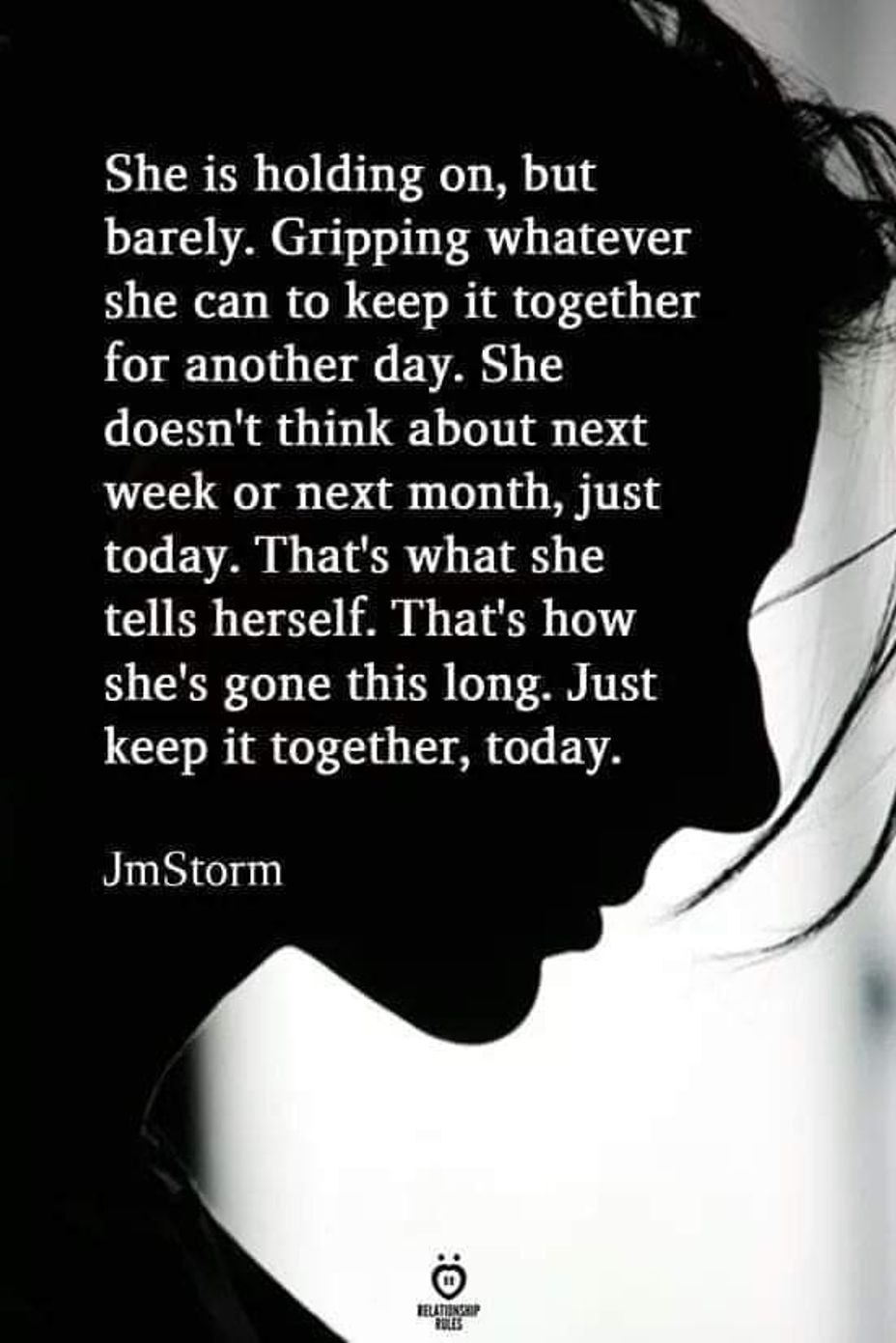
But inside…
I wasn’t steady.
I wasn’t calm.
For weeks, I carried her with me.
I couldn’t sleep.
I couldn’t eat.
I would wash my hands over and over,
trying to scrub off something invisible.
Not blood —
but guilt.
Was there something more we could have done?
Did I miss a sign?
Did I say enough? Do enough?
It was a spiral —
and no one noticed.
Because we wear white coats.
And white coats hide everything.
That experience pushed me into a dark place.
A place where I questioned my calling,
my worth,
even my right to carry the title “Doctor.”
But here’s the thing no one tells you:
Grief doesn’t make you weak.
It makes you real.
It makes you human.
And if you don’t let yourself feel it —
you go numb.
And when a doctor goes numb,
patients become numbers.
And the healing dies with the compassion.
So to every healthcare worker who’s ever watched a life slip away:
It’s okay to break down.
It’s okay to cry.
It’s okay to need help.
We were taught to be strong.
But we were never taught to be kind to ourselves.
And that’s where we fail.
Mental health is not a luxury.
It is survival.
To the young doctor out there —
tired, scared, barely holding on —
please don’t bury your pain in silence.
Talk to someone.
Write it down.
Pray.
Breathe.
Let yourself feel —
so you don’t forget how to care.
And to the families who’ve lost someone in our hands —
I want you to know:
We remember.
We carry them with us.
Their names. Their faces.
Their last moments — etched into our souls.
She was my first loss.
She wasn’t just a patient.
She was a mother.
A wife.
A dreamer.
And now, part of her lives in me.
Because every time I deliver bad news,
every time I stand by a bed that goes quiet —
I remember her.
And I keep showing up —
not because it gets easier,
but because it matters.
What it feels like to see a life slip away?
It feels like your heart breaking…
and still choosing to return to the battlefield the next day.
That…
is the silent strength of being a healerLet there be light in healers’ lives so that they can heal us all.
#PTSD
#MentalHealth
#healthehealer
#empathyispower