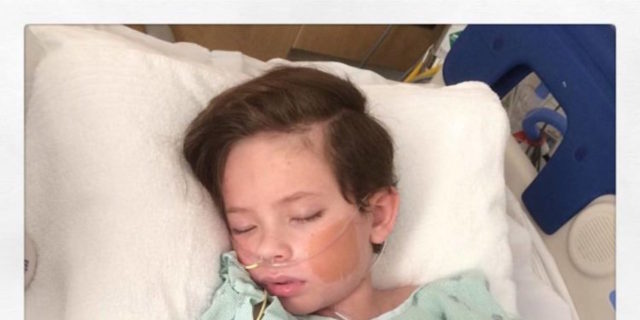
Zoo Time #Epilepsy #FebrileInfectionRelatedEpilepsySyndrome
Our family just moved to a new city for my husband’s job. Now we have to find a new PCM, Neurologist, Therapist, school- it can be a bit overwhelming. We’ve been unpacking all week, but today we decided to take a break and head to the zoo. Of course, this means bringing regular meds, rescue meds, and our VNS magnet just in case. Especially since we are currently weaning medication. We did have to leave earlier than planned, as our LO was getting too hot, and water just wasn’t cutting it for him. One of his anticonvulsants doesn’t allow him to sweat as much as he should, which can cause him to overheat and possibly lead to a seizure. Thankfully, we left early enough to prevent that from happening. No seizures. Overall though, we had a fun break.