Tonight I light every candle
Tonight I light every candle
For in five and a little less than half hours
Ten years will have passed
Since half my mind
Left half my body
Behind
And a new life began
Yet
/Never once was I ever left alone/
So on April the 25th
On my brother’s birthday
The day Grandma Adams died
At 4:25am
When the hemiplegia set in
This anniversary I’ll celebrate
the faithfulness of forests
Breath in lungs
Songs in trees
For every time they drove me
Just to feel the breeze
And the water flow beneath my feet
—
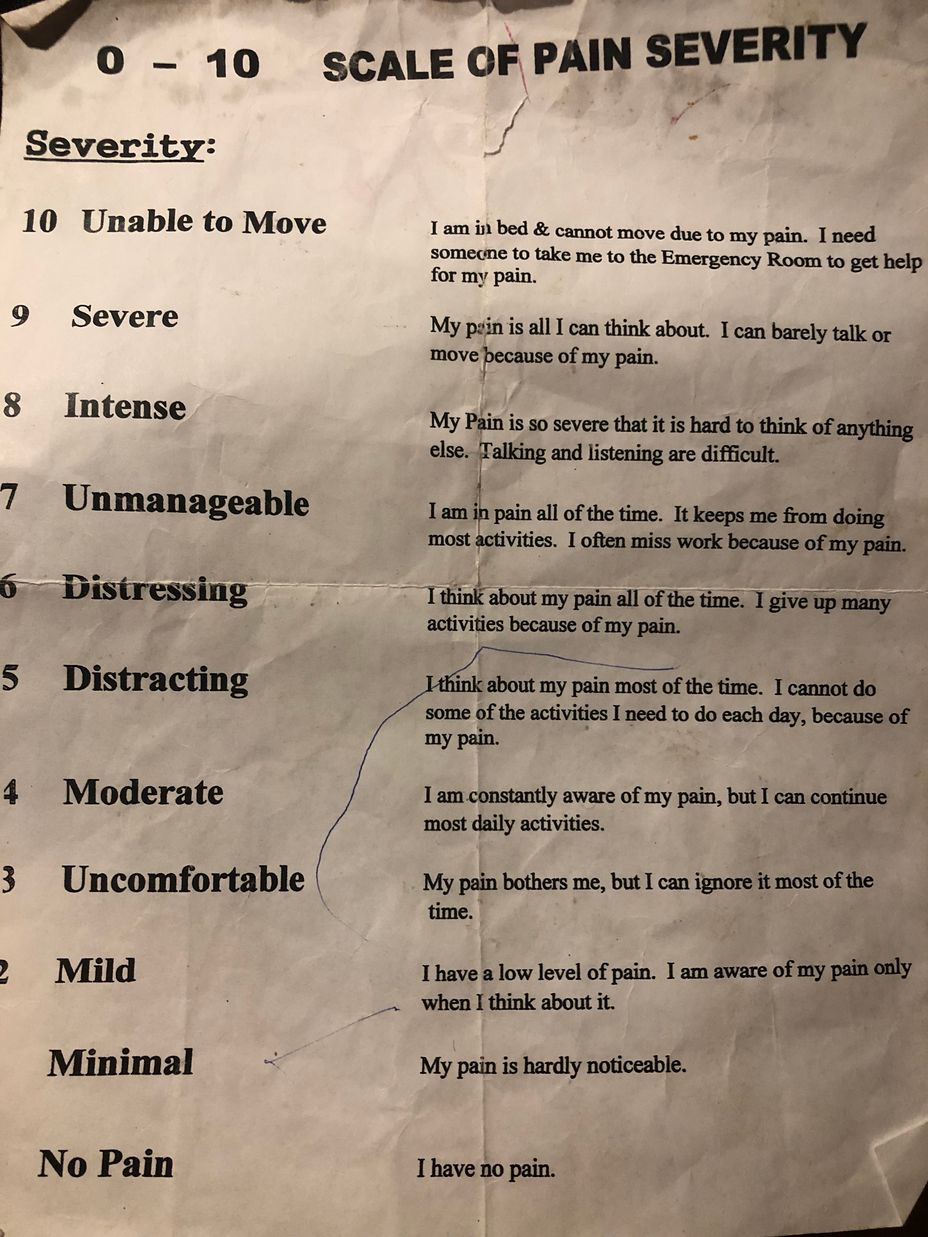
The poetic irony here being, migraine destroys all my attempts at returning such faithfulness. I only can depend on pain returning, but know not when or where, it’s duration, or intensity. For those who were strained beyond what their unyielding plans could bear, we have loved through heart emojis sent less and less often until obsolete. Those never truly lost, but faded like flash fire I still hold dear. Still find tooth-filled smiles in rooms only my heart can embrace. I miss their arms. They do not miss mine, for they do not think of me. To bothered by my broken promises and freed by the cut ties of friendship. I love them like stars without heat.
New friends, I struggle here to make.
Flames quick to light never last. I feel like, wet wood. Hilarious, waterlogged and drought cracked in the same being. Of course, I would. I am always two. Never not been.
But this is not about me
This anniversary.
This is to all who drove five hundred miles
Slept under new roofs
Ate dust
Swam in sulfur
Plastered and mortar
Those who made a house
into the best home it could be,
tried to bring I back to me
Those who went into the pines
dropped dead juniper to heat
our water through winter
Sisters who don’t share DNA
Calling me out
Across mountains
Still believing
There was something
Worth receiving
Those who remember
I have a heart ever-breaking
Not just a head
But a soul resurfacing
I’m not dead yet
Though they said I would be
A decade it’s been
I’m grateful to thee