Books With #RareDisease Representation
Many health challenges don’t get enough representation in literature. I think that definitely needs to change. Finding more common conditions in books is hard enough, but when you have a rare disease, it can be even harder to find yourself represented in a book.
That’s why I decided to compile a list of some YA books that contain characters with rare diseases. I hope some people can find a book to relate to on this list!
”Cursed” by Karol Ruth Silverstein Erica “Ricky” Bloom’s life has taken a turn for the worse. As if dealing with high school, her sister’s transition to college, and her parents’ divorce wasn’t enough, Ricky is diagnosed with #JuvenileIdiopathicArthritis . Ricky uses profanity to cope with her #ChronicPain , until her coping mechanisms are foiled by a boy with a diagnosis of#AcuteLymphoblasticLeukemia in his past and a snooty, but well-meaning, teacher. It turns out that not everyone is as they seem.
2.”100 Days” by Nicole McInnes
Agnes is not exactly like every other teenage girl. She likes pretty dresses, sewing, and music. She has a best friend. But Agnes has a disease that makes her appear several times older than her chronological age— #Progeria . With the help of her friend and an unexpected ally, Agnes’s last 100 days are her living her best life. But will the three friends be able to accomplish what counts before time runs out?
3.”How We Roll” by Natasha Friend
Quinn’s life changed when she was diagnosed with #AlopeciaAreata , which is not easy for anyone, let alone a high-schooler. A humiliating experience causes Quinn and her family to move. Quinn attempts to make friends, which proves difficult. Quinn meets Nick, who has #LimbAmputation because of a car accident. Can both Quinn and Nick learn to trust and let each other in before they build their walls too high?
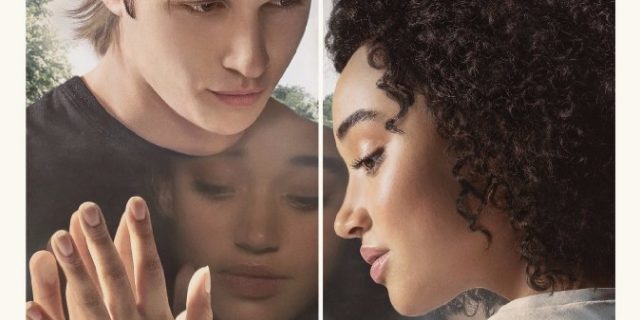
4.”Midnight Sun” by Trish Cook
Seventeen-year-old Katie Price has a rare disease #XerodermaPigmentosu m that makes exposure to even the smallest amount of sunlight deadly. Confined to her house during the day, her company is limited to her widowed father and her best (okay, only) friend. It isn't until after nightfall that Katie's world opens up, when she takes her guitar to the local train station and plays for the people coming and going. Charlie Reed is a former all-star athlete at a crossroads in his life—and the boy Katie has secretly admired from afar for years. When he happens upon her playing guitar one night, fate intervenes and the two embark on a star-crossed romance.
5.”Everything, Everything” by Nicola Yoon
Madeline Whittier has #SevereCombinedImmunodeficiencySCID , which means she can’t leave her house. But one day, she sees a mysterious boy named Olly. And Olly makes her want everything—including things she can’t have. Like love.
Art of Feeling” by Laura Tims
Samantha Herring has been in constant pain ever since the car accident that injured her leg and killed her mother. After pushing her friends away, Sam has receded into a fog of depression until she meets Eliot, a carefree, impulsive loner, who is unable to feel any pain at all. At first, Sam is jealous. She would give anything to not feel the pain she’s felt for the past year. But the more she learns about Eliot’s medical condition #CongenitalInsensitivityToPain the more she begins to realize Elliot’s self-destructive tendencies. In fact, Eliot doesn’t seem to care about anything—except Sam. And as they grow closer, they begin to confront Sam’s painful memories of the accident, memories that hold a startling truth about what really happened that day.
Happy reading! 📚💖