I'm new here!
Hi, my name is MystifiedBarbet164. I'm here because
Iam suffering from BDD since the last few months.#MightyTogether #BodyDysmorphicDisorder
Hi, my name is MystifiedBarbet164. I'm here because
Iam suffering from BDD since the last few months.#MightyTogether #BodyDysmorphicDisorder
Looking for support. My partner has BPD and I struggle with depression and anxiety. How do I manage my own depression when my partner splits on me? Example: I am at my partner’s parents house and my partner is at our apartment getting our cat, he called me very angry because our cat is giving him a hard time getting out of the house with him. During the 2 minute call he expressed how annoyed and frustrated he is and was swearing and loosing his cool. I am obviously unable to help because I am not there. Is there anything I can say to him to be supportive? #BDD #bpdrelationship #Depression #Advice
Whether this is correct title or not I’m not sure. I’m am just abit curious about a feeling I get.
It essentially is the butterfly feeling in your tummy. I get this feeling a lot when thinking of the opposite sex. I mean this in the sense of I “like” that person for a certain reason that makes me feel attracted to them.
I can tend to do this with many people and it can become a very confusing feeling.
I don’t know if it’s a symptom of complex ptsd or BPD, or whether I’m just wired wrong.
The complication in this, and please I don’t want to be judged or made to feel small and guilt, is that I have a gf. Our relationship is far from perfect.. but I have also had this feeling with previous partners and even when I was with my ex wife.
I don’t know what it’s all about. Maybe something for therapy?
Is this something associated with another condition?
I’m an Asian woman, 54, living on the west coast. I have BPD, Bipolar/schitzoeffective, anxiety disorder, maj depression and now I find out ADHD/autism. I’m dealing with a lot and it’s overwhelming. I’ve been melting down and I think this is me acknowledging my neurodivergence. I’m confused and feel empty a lot and my friends are few and the ones I have are starting to yell at me for not doing stuff right and I can’t be abused anymore. I lived that way for 50 years. It’s enough. Please reach out. Love to meet some of you.
#BDD #AutismSpectrum #Bipolar1 #SchizoaffectiveDisorder #MajorDepression #MentalHealth #AnorexiaNervosa #BingeEatingDisorder
Body dysmorphic disorder (BDD), occasionally still called dysmorphophobia, is a mental disorder characterized by the obsessive idea that some aspect of one's own body part or appearance is severely flawed and therefore warrants exceptional measures to hide or fix it. In BDD's delusional variant, the flaw is imagined. If the flaw is actual, its importance is severely exaggerated.
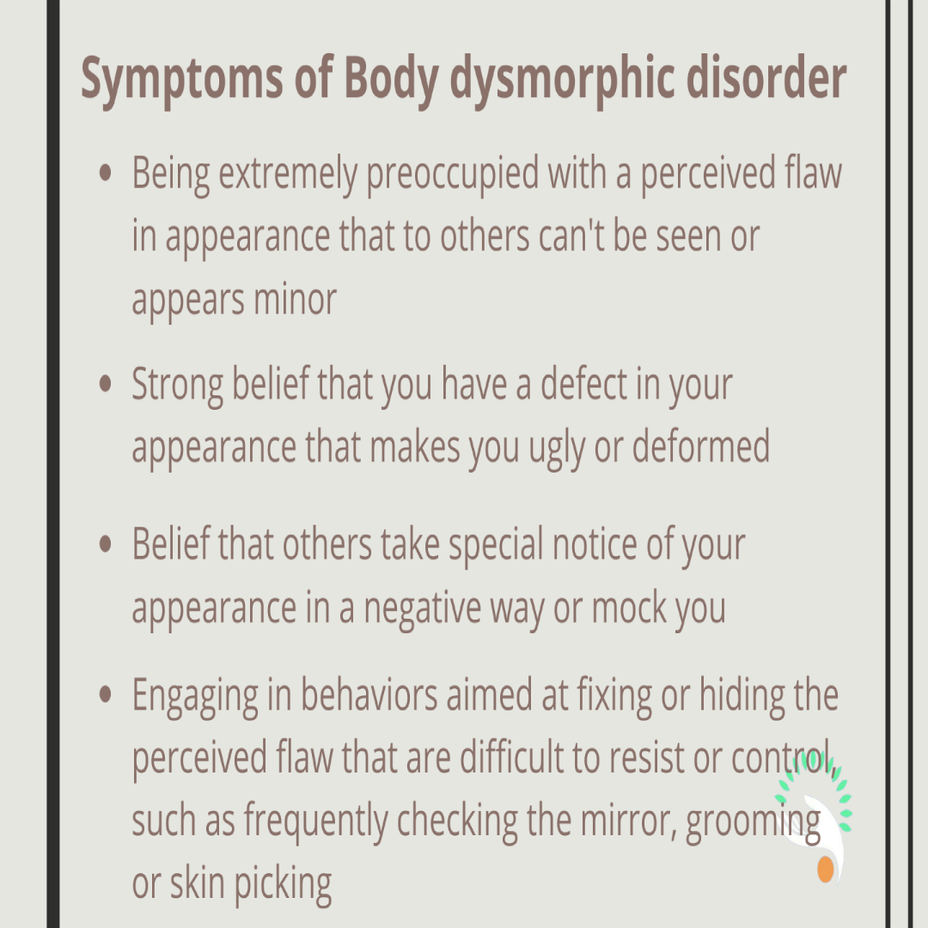
Symptoms of body dysmorphic disorder may include a person:
-strongly (but incorrectly) believing they have a physical defect that makes them ugly
-frequently checking their appearance in mirrors, or avoiding mirrors
-wearing a lot of make-up or growing a beard as cover
-spending a lot of time grooming
-constantly comparing their appearance to others
-seeking reassurance regarding their appearance
-following a strict diet
-exercising excessively or weight lifting
-taking anabolic steroids or dietary supplements
-undergoing cosmetic surgery
-tanning excessively
-compulsively picking at their skin
-frequently touching parts of the body they don’t like
-avoiding going out or being with other people, or being photographed
You can refer to this:
Had to go to a doctors appointment today to get my blood taken in relation to liver problems, I’ve also now been off my medication for a long while.
It can cause a lot of mental conflict, like a battle in your own mind, but I push through as I know I need to do to reach a better place. #BorderlinePersonalityDisorderBPD #BDD #ComplexPTSD #PTSD #MentalHealth
My girlfriend and I have been on a break for 5 weeks, in order for her in her own words, “to work on myself so we can have a healthy relationship”. We had promised each other that we would remain loyal, dedicated, and supportive to each other as this whole break was to enhance our relationship in the long run. Unfortunately, I found out recently that she chose to sleep with a friend, breaking that promise that was made, and losing my trust. She had allegedly been cheated on by other relationships throughout her life, and told me she couldn’t have possibly trusted me to be loyal to our promise, so she had to do this in order to avoid personal hurt. I was loyal, and held that promise dearly, and now am utterly devastated by her choices. I’m trying to understand why she would’ve thought this was the only acceptable solution. Would anyone with similar experiences have ideas as to what logic was used here?
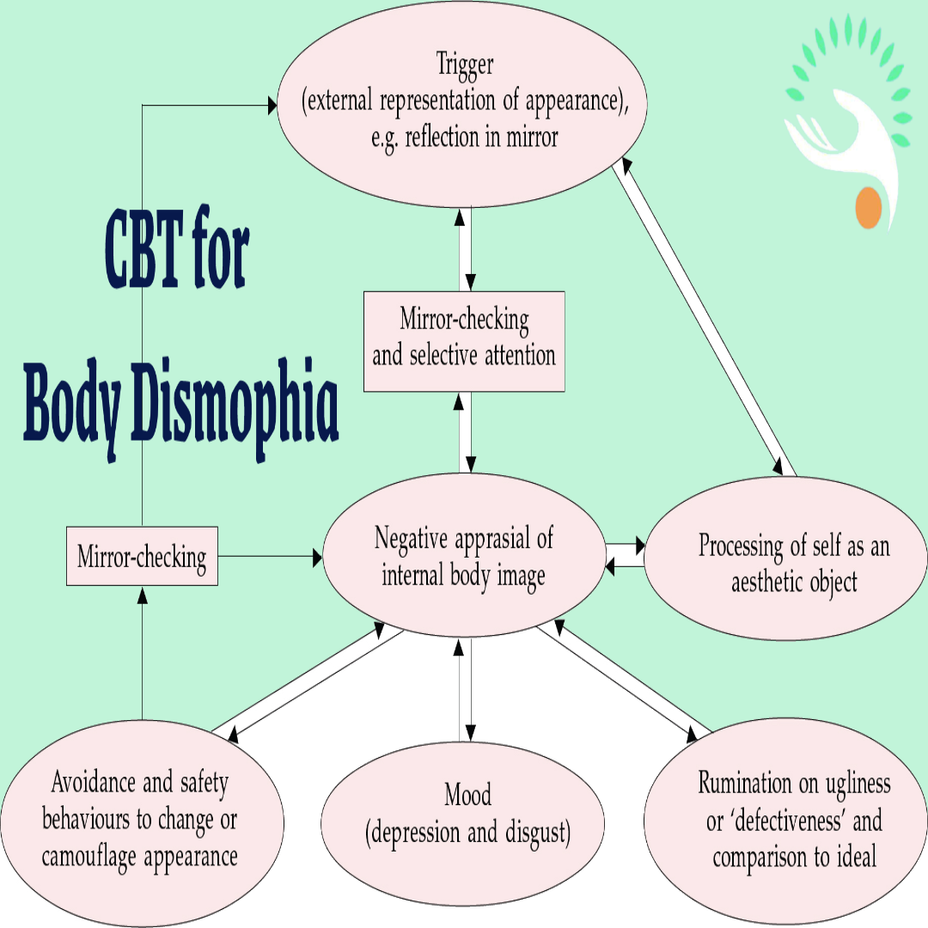
The model of BDD shown in focuses on the experience of patients when they are alone (rather than in social situations, when their behavior is likely to follow a model similar to that of social phobia; Clark & Wells, 1995). The model begins with the trigger of an external representation of the individual's body image, typically in front of a mirror. Alternative triggers include looking at a photograph taken when the patient was younger.
The process of selective attention begins by focusing on specific aspects of the external representation (e.g. the reflection in the mirror), which leads to a heightened awareness and relative exaggeration of certain features. As a result of this process, the person with BDD constructs a distorted mental representation of his or her body image.
Mirror-gazing activates idealised values about the importance of appearance and, in some patients, values about perfectionism or symmetry and thinking of the self as an aesthetic object. This leads to a negative aesthetic appraisal and comparisons of three different images - the external representation (usually in a mirror), the ideal body image and the distorted body image. Not surprisingly, these repeated comparisons leave the patient uncertain about his or her appearance, which encourages further mirror-gazing.
The patient's desire to see exactly how he or she looks is only rewarded by looking in the mirror. However, the longer the person looks, the worse he or she feels and the more the belief of ugliness and defect is reinforced. When not looking in a mirror, the individual may focus attention on his or her internal body image and ruminate on its ugliness. There is often a marked discrepancy between the actual and the ideal body image, and this inevitably leads to depressed mood and negative thoughts.
You can refer to this: