I'm new here!
Hi, my name is Armadillo26. I'm here because I want to live more peacefully despite my parents' COPD and lung cancer (My father passed from this).
Hi, my name is Armadillo26. I'm here because I want to live more peacefully despite my parents' COPD and lung cancer (My father passed from this).
Today my dad was diagnosed with lung cancer, my family is devastated by the news and I can’t stop crying at the thought of losing my dad #cancersuck #LungCancer
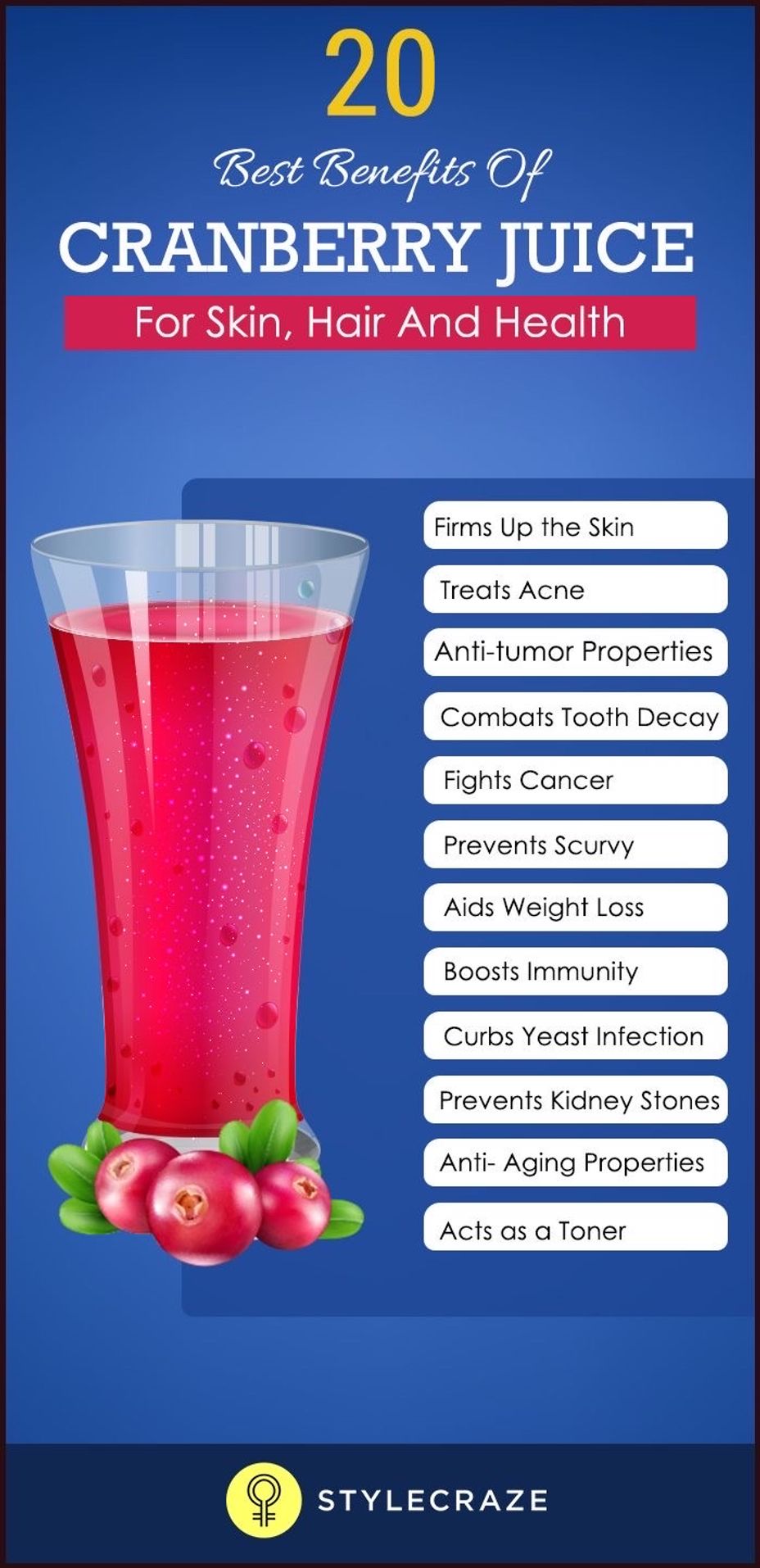
So I’m sitting outside on the back deck, relaxing in the sunshine and thinking about today and life in general but also enjoying my health. I started drinking cranberry juice a couple weeks ago. I prefer the mixed flavors but right now I’m going through two bottles of straight cranberry . And by the way today is the 17 year anniversary of my dad‘s passing from lung cancer five weeks from diagnosis to death. It’s been a wild ride and honestly, I’ve hated it because my emotions can go at any direction at any time. The life of an autistic woman who no longer has the anchor in her life, but I do the best I can #LungCancer #cranberryjuice #Autism
Hello! I am in the process of a official diagnosis of BP II. After a long stent of severe depression. My husband was diagnosed with lung cancer in 2019, and passed away in 2022. I had lots of depression throughout his cancer journey, and lots of anger as well. After he passed, things really changed. My depression was so debilitating and the RAGE. In 2 years I managed to run everybody out of my life but my mom, dad and 1 of 3 sons, work became entirely unmanageable. After many times of just laying in bed and calling my son and asking him to take me to the hospital because I don't want to live feeling like this, and eventually I put into plan to end my life. I finally opened up to a friend of mine that is a RN. I opened my heart and my shame to her. She told me I needed to get help, and down the rabbit hole I went.
I initially was put on Mirtazapine and OMFG, I felt like I was on meth, no sleep for about 7 days, running through the house thinking I was cleaning but instead it looked like a tornado touched down inside, I could not consetrate on any one thing without a flood of ideas just pouring into my head,the impulses, paranoia and then walking the tight rope of anger and rage.
I called my Dr. And they took me off of mirtazapine. So I am currently in the process of changing Dr.s, because that has been a whole other S**t show.
Now I am not on any meds, and have a multitude of both depression and mania. Hoping to get the ball rolling soon, because the mirtazapine really did help with my deep emptiness.
#BipolarDisorder
My husband may have stage one lung cancer. Super fortunate, I know, to have found this early. He was screened as part of a study of long term smokers at Kaiser. We have been given feedback from doctors that it is likely cancerous, not in the nodes and the prognosis is great. We have been coping reasonably well. but I am a little concerned/frustrated by some of my husbands defense mechanisms. He often avoids uncomfortable conversations and we have not yet told our young adult daughter or his siblings. He has a biopsy next Friday and then perhaps surgery, and if not radiation. We've been married 26 years and I know him. He would love to just have me do the dirty work, but I think this is his responsibility. We are on the same page about our daughter and she lives in the same city as us. He has said that if he does radiation, he wouldn't even tell his sisters, and even suggested that he doesn't really want to say anything to his sisters at all. I think he thinks if he doesn't call his sisters that I will do it for him. I told him that if he needs surgery he has to tell his sisters beforehand because I didn't want to be the one to tell them if something g-d forbid doesn't go well. I made it clear that I would not do that for him. AITA?
1. Panic over health changes, test results. and treatment changes.. Feel hesitant about sharing fears with spouse because he already heard a brief bit of it last week and he also takes caref his 88 year old mum twice a week.
2a. Also both ourselves and our families are neurodidiverse including autism for ourselves, BPD among some of his family, and OCD, within my family and possibly Aspergers (sp?). Also cpstd from older generations, in both our families.
No we don't have family contact if we can help it. Family involvement can make it worse.
3. I was diagnosed in June 2021 luncaner with lung cancer in the lower right lobe, staged 4a or 4b. I was advised to get my affairs in order, but was put on a chemo regime. Had a delighted oncologist 6 weeks later ,as the regime was working at the time.
4. I've had scans of all types over 3.5 years, and genetic testing. Last year, some small Mets were detected and I was put back on infusions while staying on targresso ( oral, daily). I have had difficulty with infusions, usually dealing with brain fog and some incontinence(sorry). Last fall I experienced balance problems and had a few falls within my home. my mum-in -law lent me her rolling walkerto try out. I now own one.
Along with my cane collection.
The collection which I didn't use after falling backwards off my front step while trying to use my quad cane on Sept 10 of thisyear. My back is OK now, except for lost back and knee strength from resting on the futon bed without walking much.
However I became afraid of my body/balance and my house which is about my age. And is semisplit level.
5. My back and period wobbles were becoming my biggest over the cancer.
Then I had an MRI done on my head two or three weeks ago. My main oncologist's
Associate broke the news to us (he was the "onc" scheduled that day) that there appeared to be a lesion on the cerebellum. My poor husband was shaken.
6. Now,2-3bweeks before this news I was switched off tragresso to a new med just approved by FDA. It's formulated--along with a new infusion--to target mmy cancer and possible mets. By last Thursday he had called another prescription for a steroid to work on the lesion. He wants to see how this works before pushing on to radiation therapy. But he would like meto ge ta follow up MRI-- farther had that request in by Friday.
7. So far, the steroid seems to add tothe brain fog. I'm supposed to take it 3x a day with food , along with my nightly Paxil. On Saturday, my husband and I got our flu and covid vaccinessothat effect may have added to my fog and weekend panic.
8, Monday will be my first day on my own since the steroids (he tends to his mom on Monday and Thursday).I will attempt to work from home with brain fog. Tuesday is my next infusion at 8:45. (I forgot--Monday I get a blood draw at7:30am for my Tuesday infusion. )
9. i'm wiped out physically mentally emotionally and spiritualy.
Tuesday is the election for hell which I wanted to participate in--but I can't find my ballot. Following an infusionin the morning, I don't trust myself to fill out a provisional ballot.
We did find old paper work for the Dept of moto vehicles. So now I can get my cardp tags I should have ordered last month. What the hell, im afraid to drive myself. It barely matters.
Next week is a 3 day weekend. Maybe I'll get our taxes extension filed. Like I was supposed to last month. I hate ADHD. or AuHD. My brains and life and finances are falling apart. I don't have my funeral or will planned. I'm the one that does the bills,like my Mom did. I know how that turned out when she passed before my dad.
Oh and retirement. I had to wait until this year to retire and still retain my med benefits for my husband and I, Last week the college I work for announced that we a)l have to work on campus starting January. I replied on Wednesday this week that I wanted to retire. I wanted to use next 3 day weekend to work on retirement. After the lesion news of last Thursday--
I don't know .
My phaser is set to stunned.
Anyone got a prayer or a Saint or some juju. Because I'm out.
I just want to post the truth here, that none of my friends or coworkers know and my husband doesn't fully understand.
I had a damned meltdown yesterday Sunday Sept 29. I'm 64, dx with lung cancer in 2021, still on chemo, have develop occasional incontinence, balance problems, fell on Sept 10, was diagnosed with a ruptured L6, am trying to heal my back while working from home at a job I hate, (they dont know I've a fall, they may know I am now slurring my speech because I am answering the phone lines)
...and my C-PTSD is kicking because I haven't completed a weekly work report I was assigned at the end of August because no one has completed my Training on where to find all the data.
...and now I'm panicking waiting for this week's blowup via zoom meeting
... and now I have to go and find something to eat before work starts and cry a bit for release.
Damn sorry for this post
I've started having falls in the last 12 months. Last Tuesday was outside the house. I finally went to urgent care on Friday; they recommended a visit to ER for a CAT scan. Found a flattened L6 disc. No shards which is good. They said their focus is pain management right now
The pain is doable; my focus is not falling again and find exercise for knee strength and total body balance.
I'm also under chemo treatment for lung cancer (3 years since dx)
I have a chronic fear and mistrust of my body. When will that stop?
Hi, my name is Warpig. I'm here because
I've had full body weakness for about 5 years...... initially in my search for answers I was diagnosed with multiple myeloma but as time went on my weakness got worse.......then came the shortness of breath...No specialist's that I saw could determine what that was after numerous appointments and scans......going back to my myeloma specialist.....he ordered a PET scan..... finally a lung biopsy as he suspected lung cancer......nope.....I have severe Valley fever.....the lesion in my lung was from Valley fever....that may explain the shortness of breath but not the weakness....my next appointment is with a neuromuscular specialist..... I'm trying to help with what I think it may be.........#MightyTogether
Hi, my name Jenny coxy I'm a survivor of lung cancer .
I'm here to meet new people, interact and make new friends