Moebius Journey, with Wesley
My second pregnancy was as uncomplicated as my first. Hence, after the scan in my third semester, I looked forward to the birth. I was rushed into the theatre after three failed epidurals and Wesley was delivered by Emergency Caesarean.
While battling to open my eyes in the recovery room, trying not to concentrate on the pain after my caesarian, I heard one of the nurses passing a comment: “shame, if only she knew”. The doctors told me: “he might not be able to see, hear, talk, walk, in fact, he won’t be educable. He hardly has a brain. He will need constant caring and would need to be institutionalized”.
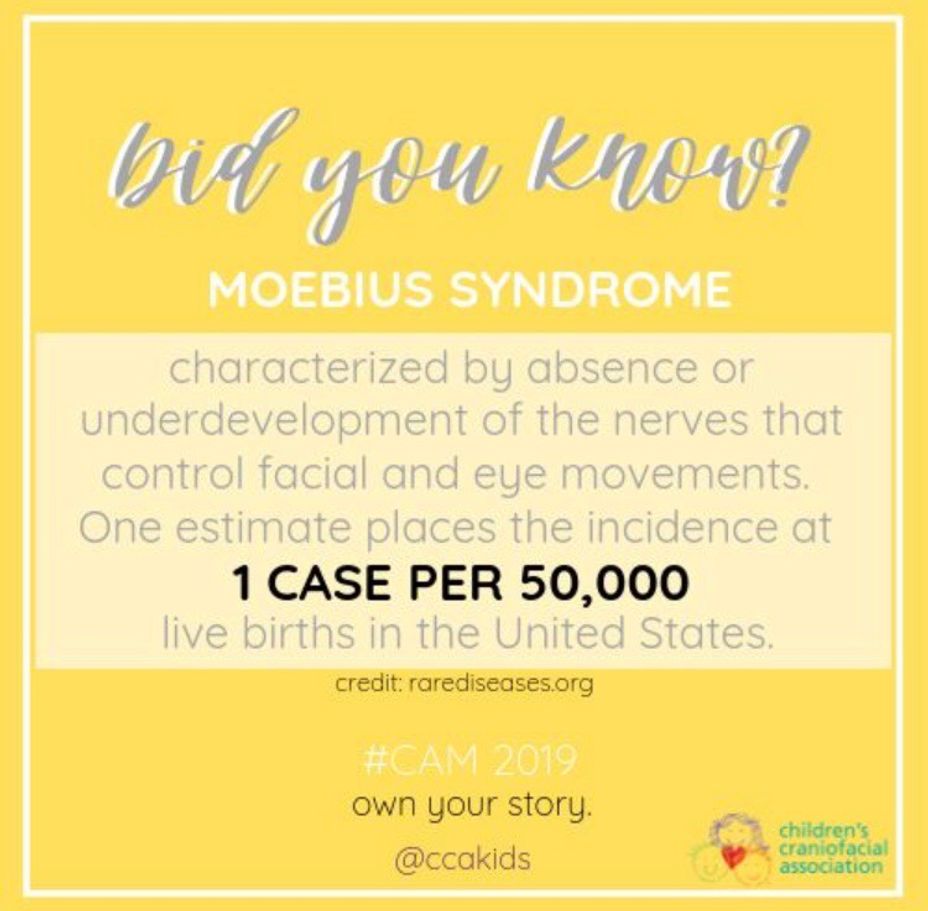
Still, in shock, I was told: “Your baby is very sick and might only live for 2 weeks, but if by a miracle he survives, he might not grow older than 18 years”. The diagnosis was Hydrocephalus, Moebius Syndrome and Poland Syndrome. I recall how devastated and helpless I felt.
For 3 days I shut myself off from the world, refusing to see him or hold him. Instead, I prayed, cried and perfected my negotiation skills with God, whom I couldn’t allow to get off lightly. After all, I told Him: if you entrust me with this special child, give me the courage to cope, the love to hold him and protect him and the determination to never give up on him, and a three-some pact was sealed that day. Wesley survived against all odds, and up to the age of 13 years managed a hassle-free VP Shunt which had been inserted when he was 4 days old. I recall a further conversation with God when I thanked him for giving Wesley to us but telling him how I longed to hear him say “mommy”.
His development was noticeably slower than other babies, but a friend who cared for him since the age of 9 months would give me a rundown of his daily activities when I fetched him after work. She recalls how he would turn his head as cars passed the house, attracted by the sounds he heard. When he was just a few months old my sister sent him a Fischer Price CD player, with nursery rhymes. His favourite was Twinkle Twinkle Little Star, yet, when we changed the CD to Baa Baa Black Sheep, Wesley objected with what could only be described as an early toi-toi (an African way of objecting to unhappiness by means of chanting or dancing). He displayed a strong rhythmic sense and he showed his appreciation for music by thumping his feet to the beat especially when we turned the volume down. In true Wesley fashion, at the age of three, 23 July 1999, bypassing the crawling stage, Wesley could walk, talk, and pretty much caught up with his peers reaching each and every Moebius milestone.
What struck me was that Wesley’s development was never recognized or acknowledged by doctors purely because he bypassed the expected “due date” which resulted in his achievements becoming a reason for the family to celebrate and acknowledge his blessings. With my wonderful support system at home, we crossed each and every hurdle with flying colours while Wesley enjoyed the words of encouragement and praise, and of course the fuss.
With many instances of school bullying and beating, Wesley remained strong-willed, positive and kind-hearted. Until about 3 months before he died, he never raised his voice at me. Like always, he greeted me at the door, asked about my day and would follow me into the room. There I would hear about his day and what he did, whom he saw and which girl attracted his attention that day. We would usually talk about the “girl” situation, reassuring me that he wouldn’t step out of line, that he believes a girl should be treated with respect but also lovingly reminding me that he had heard that “lecture” far too many times. He would ask about dinner and follow me into the kitchen as if he was going to help, only to make sure what’s for dinner and off he would go to his room. That night though, was different, he returned from his room minutes later, boldly shouted: “why me, why not Melissa or Kristen, why did you have to do it to me”. I was shocked, hurt and bewildered. After what seemed like hours, all I could utter was “Wes, I don’t know. I’m sorry; I think you should ask God.” Some time had passed when he eventually came back into the kitchen saying: “Mommy Kay, I’m sorry. I’m ok, I’m fine with who I am – besides, soon I will be able to smile just like you”.
Soon forgotten, Wesley was his old self – keeping the girls in line and as so often word of advice to his elder sister, reprimanding her on her dress code with a “I see too much, or please wear something else before you step out of the house or a firm warning to stay clear of drugs and alcohol and a subtle plea not to venture into easy relationships” – the advice Melissa now tells me she misses dearly and valued so much about her brother.
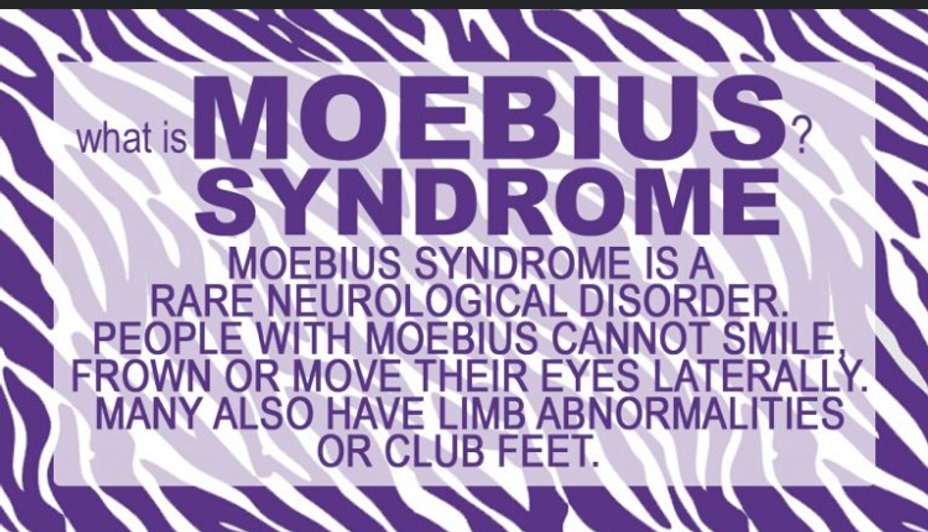
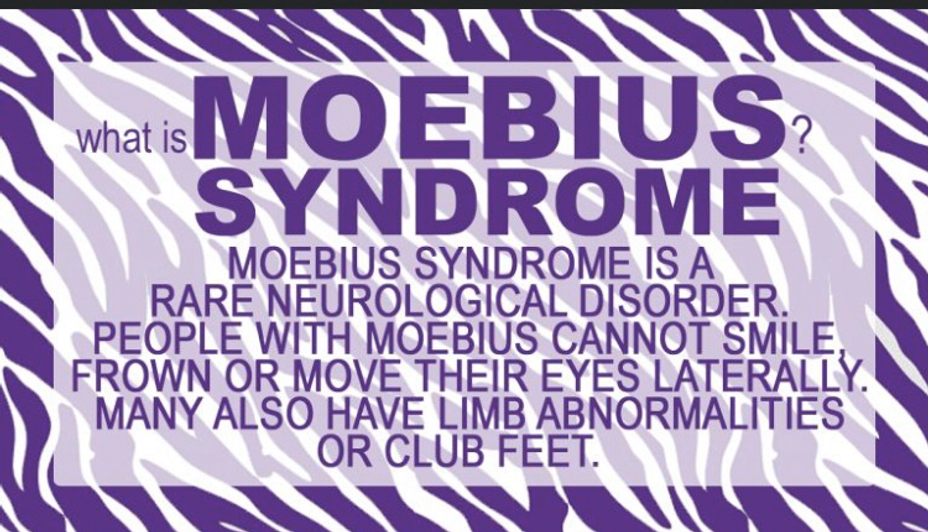
In short a bit about Moebius Syndrome
We have to be careful how we make someone living with this syndrome feel.
The facial expression of another person is often the basis on which we form significant impressions such as friendliness, trustworthiness, and status.
What we often overlook is that while someone living with Moebius Syndrome has no facial expression, he/she can easily interpret the shock on another person’s face when coming in contact with them.
With obvious facial differences, speech problems, eating difficulties, children with Moebius Syndrome are often victims at the school where they are teased and bullied.
They have difficulty in participating in ordinary child-like activities such as blowing out their birthday candles, inflating balloons or even blowing bubbles.
Children might become withdrawn from society as they feel less wanted or welcome amongst their peers and are forced to deal with their emotions of anger, rejection, depression and loneliness to name a few.
On the brink of adulthood, Wesley showed signs of fear, scared that he would not fit in with friends and family. Judging from our conversations about girls, his greatest concern was if he would be able to kiss or whether she would feel the “butterflies”, but with a clear warning from me to be careful of those butterflies which always sent him off with a roar of laughter.
When Nelson Mandela picked up and read the letter wherein Thando’s mother appealed for his help, lives were bound to change. Through him, the improbable became possible. How thankful we should be that this humble, kind spirited man walked out of prison with no hatred or vengeance in his heart. Lives changed, and so did mine. Through an unselfish act of Nelson Mandela, children like Thando, Wesley, Kelobogile, Divan and many others have received quality of life!
Thando was also born with a rare genetic disorder affecting the facial nerves. Thando couldn’t smile!
Without hesitation, he approached a very prominent businessman, Bertie Lubner who in return consulted with his son Marc who then contacted Prof George Psaras. A Canadian, Dr Ronald Zucker, flew to South Africa to meet with Marc and George to assess Thando as a suitable candidate for the procedure he had performed on children with Moebius Syndrome. In 1999, with Nelson Mandela as a Founder Patron, The Smile Foundation was born.
Thus far the Smile Foundation has hosted many Smile weeks and during such a week up to 40 children receive free medical procedures which range between cleft-lip & palate, cleft-lip, facial burns, facial paralysis or Moebius Syndrome (also referred to as Moebius Sequence)
On the eve of the Smile operation, 24th May 2007, Wesley was calm, yet excited as he had made a date with a special girl at school. I am told that he promised her ‘a night out’ but insisted that I drive them because ‘my mother would stress too much’.
With the operation being successful, the wonderful caring he received while in the hospital and the assurance that he would be back for the second phase, Wesley and I left for home, his dream like Martin Luther King’s had come true!
Friday, 20 July 2007 was like many other evenings for him. He had his favorite audience listening to his selection of music, hosting his private talk shows – including weather forecasts and the latest reviews on politics etc, when suddenly he rushed to urge me to phone Prof Psaras to tell him that he felt a twitch, that when he wakes up tomorrow morning he was sure that he would smile for me. His sisters hugged and kissed him, sharing his excitement. I told him I couldn’t do it, that it was too late and that I was not sure where Prof Psaras was at the time. I assured him that I would inform Prof Psaras via email Monday morning and that he should be patient till then.
When I found him sitting on the bed early hours of Saturday morning, I immediately told him that we should go to the hospital, about 50km away. Wesley told me that God was taking his pain away and that I shouldn’t panic. But nothing seemed to matter to me more than to get him to hospital. I offered him mild pain medication and soon after he dozed off to sleep. He alerted me again at 9h00 that morning.
When the Neurosurgeon eventually got to see Wesley, he was talkative, cheerful and responsive. A full blood count was taken, he was going to be sent for a scan and if there was a reason for concern, they would hospitalize him for observation. Being admitted to the trauma unit, I was not allowed to stay with him and stepped out for 20 minutes for them to complete the tests.
Upon my return to the ward, I found him with his head turned, not responding to my voice and I could clearly see that his lips had turned blue. The nursing sister who had asked me to leave, assuring me that she would notice when something went wrong, was nowhere near him but came running when she heard me crying frantically for someone to help.
After an emergency operation to release the fluid from the brain that same day, and the subsequent observation thereafter, we were told by the Neurosurgeon that he had reached his mortality, that Wesley would not ever be the same again. Wesley was declared brain dead and that day, 22 July 2007, we had to say our goodbyes.
I don’t know if it will get better or if this deep sense of loss ever fades, but I am glad and grateful that we had Wesley. Clear to me now, is that if I could do it over again, and my journey includes Wesley with Moebius, I would want to do it again.
My Moebius journey has not ended as I intend to share and help other parents in South Africa who might be battling with the same challenges we faced.
After his smile operation, Wesley shared another dream with me – to start an organization to help others like him. The initiative is an attempt to provide non-financial support to children born with Moebius Syndrome and their parents. The support hinges around information-sharing, such as coping skills for feeding, which often is the most concerning factor at birth. Furthermore, the need to identify and document children with Moebius Syndrome will form an integral part.
The battle within them about being loved, belonging, and feeling wanted is only a few of the trials they face and it remains our duty as parents to protect and guide them. More importantly, we have to positively expose them to the community so that the outward manifestations of this syndrome can be positively embraced.