I'm new here!
Hi, my name is WhirlySparrow4038. I've been diagnosed with
#MightyTogether #BipolarDisorder #Anxiety #Depression #Epilepsy
Hi, my name is WhirlySparrow4038. I've been diagnosed with
#MightyTogether #BipolarDisorder #Anxiety #Depression #Epilepsy
This was one of the biggest lessons I've learned in the past few years. True healing happens in real time. We can't "think" or "talk" our way into healing. We have to experience it.
#Addiction #Agoraphobia #Anxiety #AnorexiaNervosa #AutismSpectrumDisorder #BorderlinePersonalityDisorder #BipolarDepression #BipolarDisorder #CeliacDisease #ChronicFatigueSyndrome #Depression #Epilepsy #MentalHealth #ADHD #Schizophrenia #SeasonalDepression #PTSD
Use this for the days ahead, whenever you need it.
#PTSD #Agoraphobia #Anxiety #AnorexiaNervosa #AutismSpectrum #BipolarDisorder #BipolarDepression #BorderlinePersonalityDisorder #ChronicFatigueSyndrome #CeliacDisease #Cancer #Depression #Epilepsy #Dysautonomia #EatingDisorders #Grief #Selfharm #SuicidalThoughts #Fibromyalgia
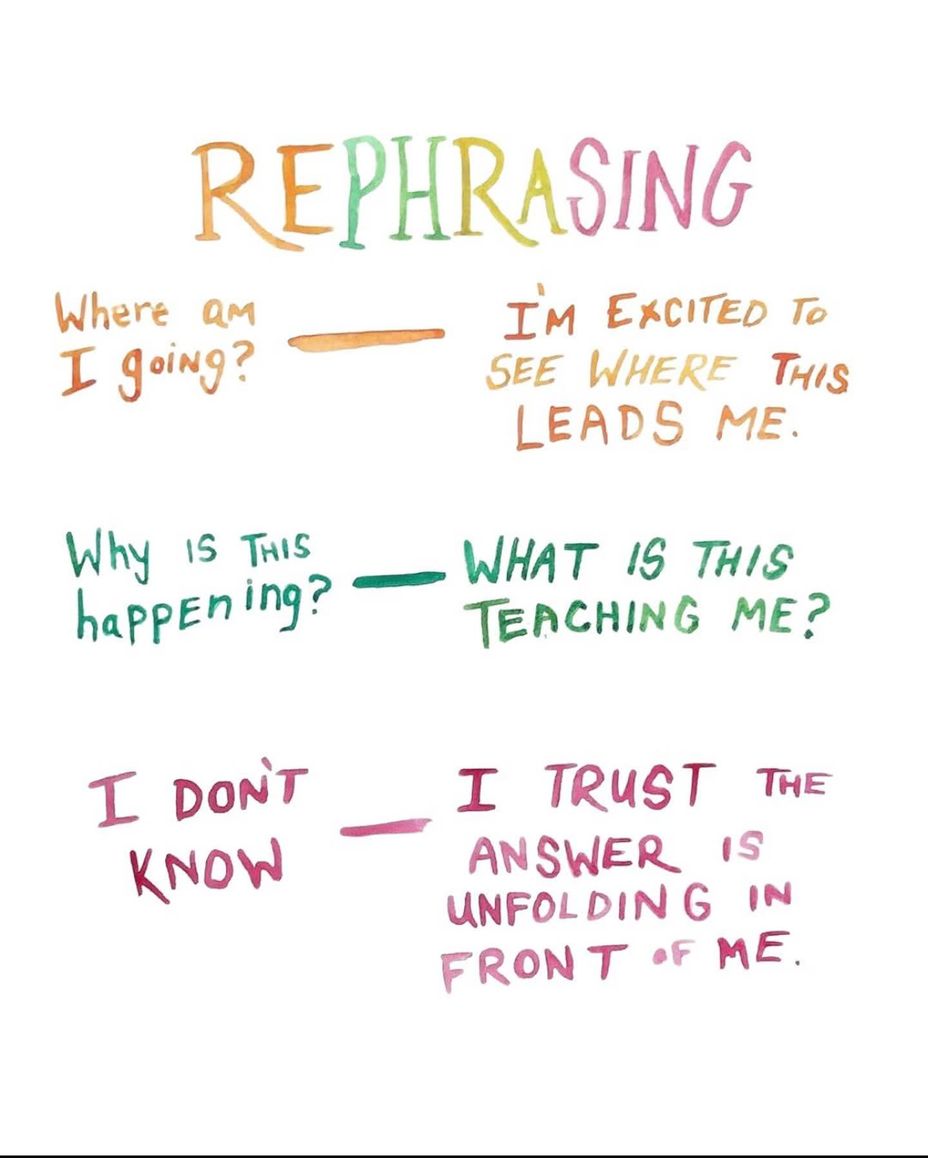
Which one of the rephrases is the most helpful?
#PTSD #Bipolar2 #MentalHealth #BorderlinePersonalityDisorder #BipolarDisorder #Agoraphobia #Anxiety #AnorexiaNervosa #Addiction #ChronicFatigueSyndrome #CeliacDisease #Depression #Grief #Epilepsy #ADHD

My cats, Ollie (back), Maggie (white cat) & Lily (black snuggled with Maggie) all agree with me that this time of year was designed for snuggling! I’m thankful for these cats every day, I wonder what I did for me to cross paths with such perfect examples of God’s creatures! They’re all foster fails (or foster successes!) which is where a fosterer decides they can’t possibly part with the animal (or animals) that they were only meant to have for a short time. They all have disabilities, Maggie is partially sighted (& takes meds for her eye pressure), Ollie has epilepsy (& ironically takes the same epilepsy meds as I do!) & Lily was born with half a pancreas (& takes oral insulin), meal times are a challenge, making sure they only eat their own food, with their meds on!
Hi Mighties! Can you stop what you're doing and join me in this grounding practice today?
#ADHD #AutismSpectrum #BorderlinePersonalityDisorder #BipolarDisorder #Addiction #Anxiety #ChronicFatigueSyndrome #CeliacDisease #Depression #Epilepsy #Cancer #Grief #Schizophrenia #AdrenalInsufficiency #Selfharm #ChildLoss #SuicidalIdeation
Hi, my name is Dylan Rothbein. I'm here because I'm always looking for support and I care about community and disability. I'm currently a rabbinical student and a musician and filmmaker. I have been and activist and disability studies scholar for 10 years. I have a BA in history and an MBA in music business.
#MightyTogether #BipolarDisorder #Migraine #LymeDisease #CerebralPalsy #EhlersDanlosSyndrome #Epilepsy #PTSD #Dyslexia #Blindness
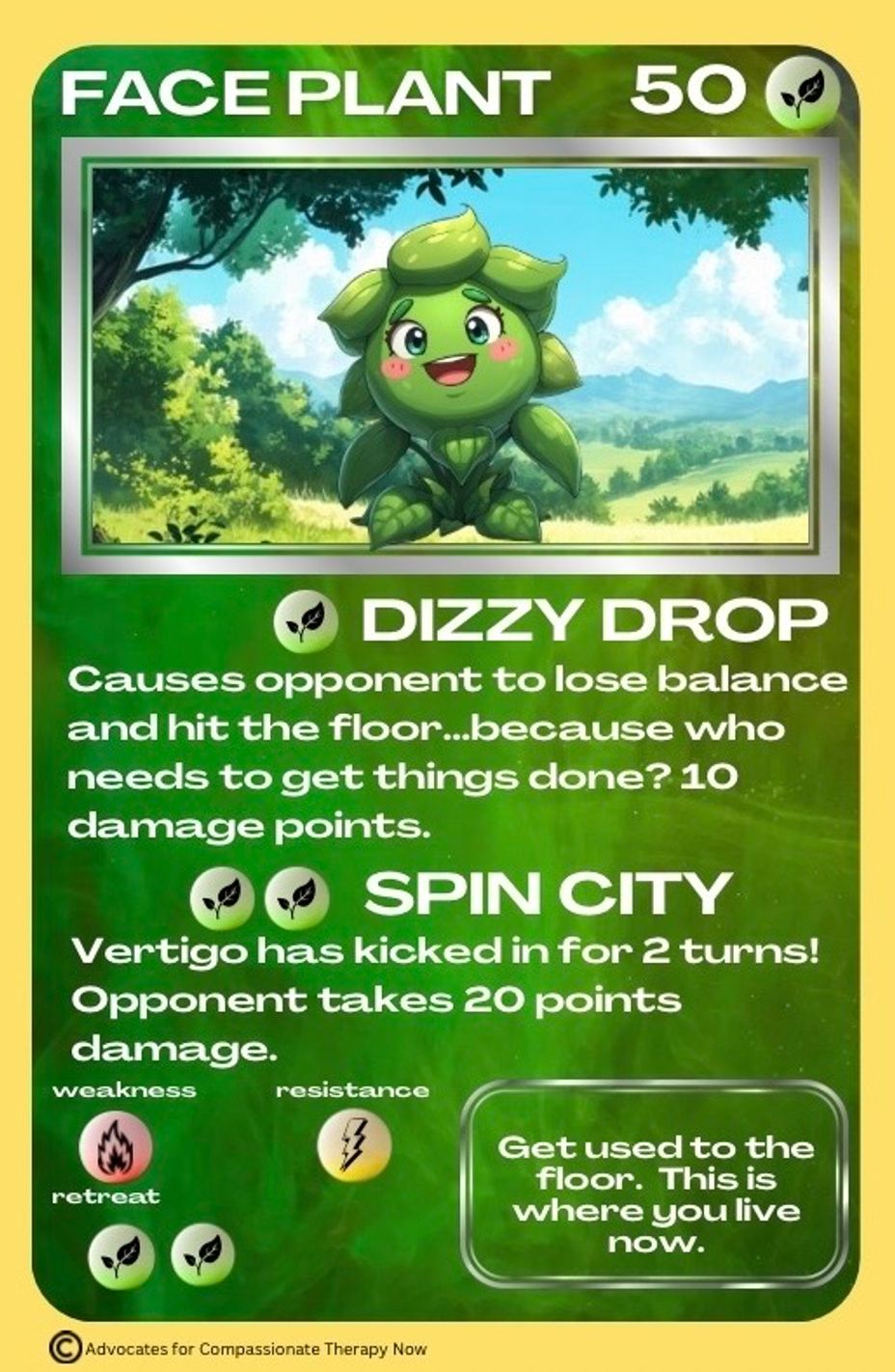
Today’s #chronicillness trading card is #FacePlant ! Many with chronic and rare diseases have bouts of #dizziness and #Fainting . Postural Orthostatic Tachycardia Syndrome (#pots ), #Epilepsy , and #Dysautonomia are some of the many conditions that have random #dizziness and #Syncope . #Maladiemon
Hi, my name is binxy888. You can call me Binx or Binxy. I've been diagnosed with Epilepsy, Lupus, Autism Spectrum Disorder, ADHD, Insomnia, Depression, Anxiety, and PTSD. I work as a director of programs at a major insurance company and own another company. I am a single mom of two teens. I spend most my time masking and hiding my conditions from people as most people do not understand chronic illness. It is very lonely and isolating. I am looking for people that are going through similar situations to relate to.
#MightyTogether #AutismSpectrumDisorder #PTSD #Anxiety #Depression #Lupus #Epilepsy
I keep having what I believe to be seizures due to my past experiences with them and the pattern, it scares me at times when I feel an aura. I don’t want to lose my awareness, I don’t want to suddenly be thrown in a void unable to register anything until passes. I am fortunate enough that I don’t convulse to my knowledge but they can be rather scary.
How do you cope?