Double OCD relationships
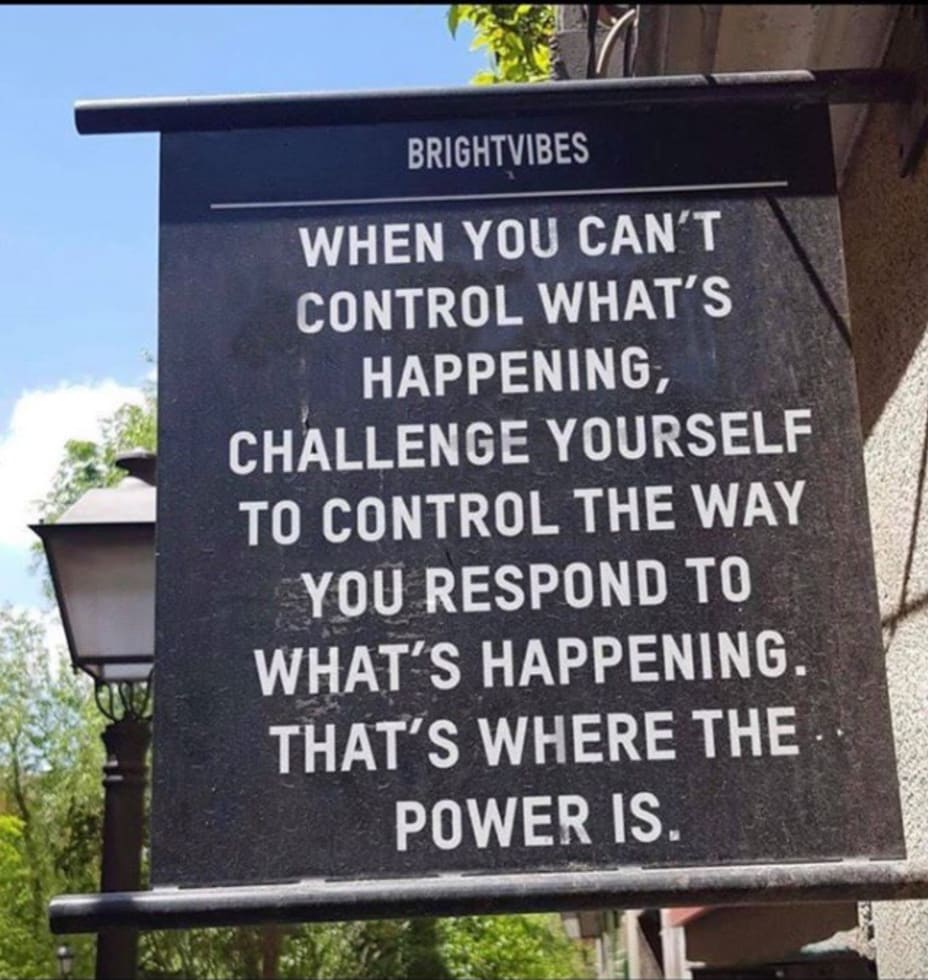
I love having someone who understands my brain, but it's so hard sometimes too. I am on hour 5 of resisting compulsively texting her, after receiving a barrage of compulsive texts from her and two compulsive calls. She knew what was happening and was trying really hard to resist, and I think she was eventually successful. But I am still having wave after wave of what-ifs about her safety. Logically I know she's probably asleep, but of course that does nothing for the doubts. For hour one I just handwrote a journal entry to her, and I thought that did it, but the compulsion keeps coming back. I wonder if I should just throw myself fully into an exposure session and try to speed up the process of no longer feeling like trash, but it's so late and I should have been asleep an hour ago (dr appointment, office hours, and lab meeting tomorrow, good lord), so maybe I should just rawdog it until I fall asleep. When the thoughts are so bad that I keep involuntarily hyperventilating for short periods, I don't know if an exposure would help or hurt.
I have however come up with a fun strategy: pretending that her compulsive texts are actually attempts to type out whale vocalizations. It removes the focus from the content of the messages and makes it easier for me to resist reassuring her and instead do/say things that are actually helpful (which is sometimes doing nothing). It's hard when it's relationship OCD-related, like today, because I automatically want to take it seriously and personally, but the silliness of imagining that all those texts are just like OOOOOoooaaauauuuuUu whale noises does kind of help.
#ObsessiveCompulsiveDisorder #ERP #ROCD #copingstrategies #Sleep #HarmOCD #Relationships #Autism #CheckInWithMe