A Rebuttal to John Thune's Assertion That The Best Insurance is a Job
In September of 2023, my brother died of complications from melanoma. The cancer had advanced to stage four by the time he was diagnosed, including three lesions in his brain and intrusions into his spine that fractured two of his vertebrae. At that point, he couldn’t lift more than twenty pounds without risking paralysis. The insurance he had through his employer was terminated three months after his diagnosis. It was contingent on his being able to work and he could not. He then obtained insurance through the state at fifteen hundred a month. He would have received sixteen hundred a month in SSDI if he had lived long enough to start receiving benefits.
My brother didn’t fear dying. He feared surviving if he would be bankrupt from medical debt. Our mother worked with a woman who died of cancer and her family was saddled with nineteen thousand dollars in bills that the insurance company would not cover. If my brother had lived, he would have had to spend ninety percent of his disability compensation on insurance; his fear of massive medical debt seemed to be well founded, given our mother’s co-worker’s example and the fact that the one hundred dollars left over after paying his insurance premium wouldn’t have gone as far as it used to regarding his other bills.
Actress and neuroscientist Mayim Bialik returned to acting when she became pregnant, because the Screen Actors Guild insurance was excellent, in her opinion. It was better than the coverage available to her when she worked in academia at any rate. On the other hand, when actress and writer Jennifer Sky developed tumors in her liver, she was dropped from that same insurance because she was too sick to work the requisite number of hours. All of this goes back to one of the reasons Barack Obama wanted to reform health care. He said that our system worked well when a person was healthy, such as Mayim Bialik through her pregnancy. The system fails when the person is seriously ill. Jennifer Sky with her failing liver, or my brother, with three brain lesions and counting, two fractured vertebrae and so many other tumors his PET scan was lit up like a Christmas tree.
A job doesn’t provide the best healthcare when your coverage evaporates when you need it the most. And please spare me any discussion about early detection and “responsibility” and the rest of that drivel. My mother’s insurance didn’t cover yearly physicals because the insurance company calculated that it was cheaper to cover the treatment for the relative few who would develop cancer then pay for everyone to get screened. My brother, despite Obama's best efforts, couldn’t afford coverage under the ACA during periods when he worked for employers that didn’t offer insurance benefits. I remember being greatly amused when officials and politicians would talk about coverage people can afford, as if anybody in government has any clue about that at all. My brother’s commuting costs were substantially greater than average for this state, because his job required him to travel to distant job sites. Those costs were not reimbursed by his employer, and he had the additional burden of funding a more robust and expensive maintenance schedule for his vehicle. Those expenses were also not reimbursed. He couldn’t have managed that and his other expenses if insurance premiums had consumed half of his salary.
You can also spare me any bullshit about how kicking undocumented immigrants off of Medicaid would have helped my brother. My state offers no services to undocumented people; you can’t cut a service that doesn’t exist. The states that do offer services to undocumented immigrants pay for those services out of state funds, as federal law prohibits the use of federal funds to pay Medicaid costs for undocumented people. Furthermore, most of the states that offer such services pay more in federal taxes than they receive in federal aid. (Mostly blue states.) If the cuts to Medicaid are uniform, people in red states will have services cut to greater extremes, because federal money makes up a larger share of the money available for Medicaid payments. Your cuts would have hurt him.
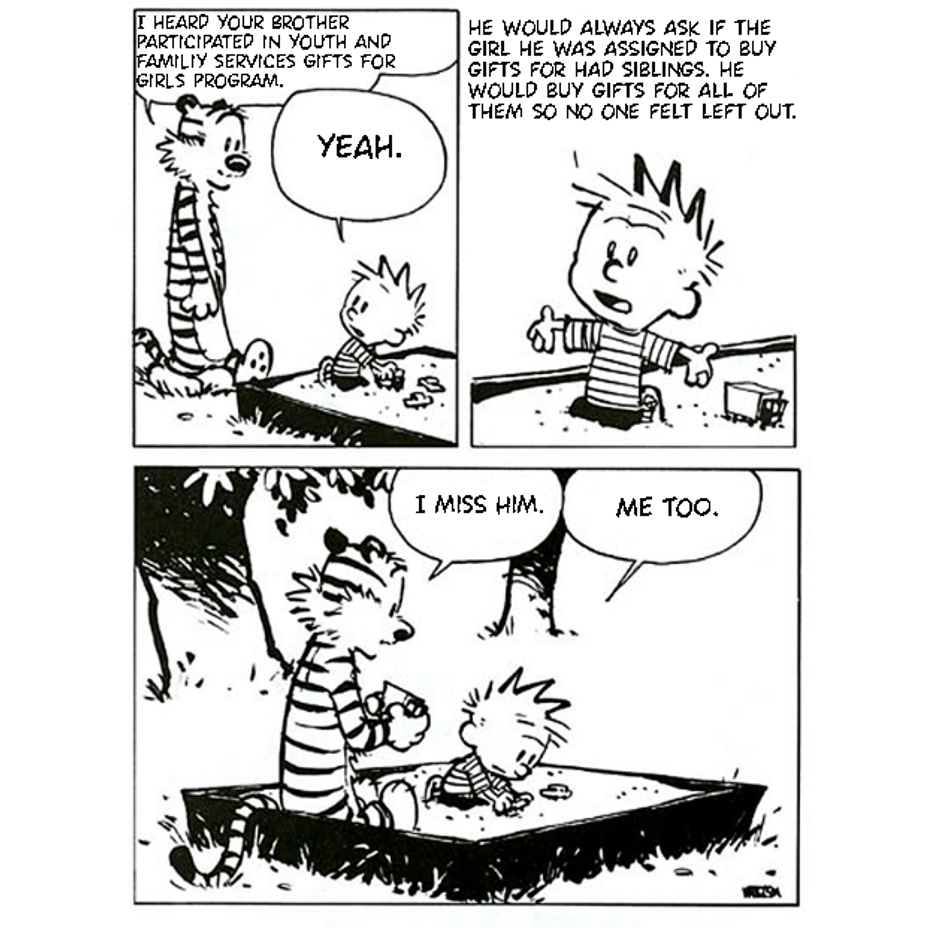
Every Christmas, my brother participated in a program that bought gifts for underprivileged children. He always asked that if his assigned child had siblings, that he be assigned the siblings as well. He would buy gifts for all of them so no one felt left out. This is the character of a man whose life you value so little, while aiding and abetting a man who spent sixty million dollars on a birthday parade for himself. In light of the cuts you say are necessary, I do not know how your government summons the strength to go on, making do with so little. #Depression #Suicide #MentalHealth #Trauma #PTSD #Disability #Cancer #Melanoma