I’m new here!
Hi, my name is okeedokee.
#MightyTogether #Anxiety #Depression #PTSD #OCD #Gastroparesis #hypothyroidism(UnderactiveThyroidDisease)
Hi, my name is okeedokee.
#MightyTogether #Anxiety #Depression #PTSD #OCD #Gastroparesis #hypothyroidism(UnderactiveThyroidDisease)
Hi, my name is Andrea. I'm here because I was diagnosed with gastroparesis. And I am looking for help managing and just being around others with this disease.
Hey, whoever reads this. I’m new to the app and trying to find comfort in community. I apologize beforehand for the long winded mess but I’ve been really struggling with my sense of self. Over the past 5 years I’ve gone from being a “healthy” individual, working a full time job, a university student and regularly going to the gym and working on myself. I was a vegetarian for almost 4 years. Now mind you, I was not a healthy child, I was sick very often and had a history of stomach issues but to my knowledge at the time this was completely normal and not a worry to my parents (they didn’t believe in doctors so one had never been seen for these issues).
In 201 9 I started to experienced some concerns.
It started with small allergic reactions to food I had previously had no issues with (spinach, pineapple, carrots..etc). Then full blown anaphylaxis for seemingly no reason. I went from a full and reasonable diet to nothing but grilled cheeses to avoid having a reaction. After my third or fourth trip to the hospital, the ER doctor mentioned something I had never heard of before: MCAs. At the time I couldn’t afford further testing or treatment so I continued my very limited diet and kept working thinking “well that’s a little set back but I’ll be fine”
During this time I wasn’t going to the gym as much as I was previously (or at all) focusing instead on classes and working. I had always had some issues with “bone” and muscle pain. Growing up, I was told it was growing pains and completely normal. I go back to the gym, 5 minutes on the treadmill and my back seized. I thought “wow, I took a month off and this is the price, I need to build up my strength again”, except I couldn’t. I was in so much pain, not just my back but my arms, my legs, my hips, everywhere and anytime I ride to workout again, no matter the amount, it would just make it all worse.
During this time I was in a very high stressed state, I was homeless trying to find a place to live, struggling with daily allergic reactions, I was failing my classes due to the pain keeping me in bed day to day. I was seemingly “sick” for no reason other than the stress. My body felt heavy, sluggish and impossible to control properly. My diagnosis for Ehlers-Danlos wouldn’t come until a year or two later.
Despite the pain, I had no choice but to work as much as possible. I didn’t have health insurance and no place to call home besides an old pickup truck so I was working three jobs, only sleeping 4 hours a night, continuing my diet of cheese and bread. I was still having daily allergic reactions and at the ER one night, the doctor was doing an evaluation of my throat. To note, I can easily dislocate my trachyia and my neck has lot of mobility. He’s the one who mentioned EDS to me. I held onto that until I could afford to make a proper appointment, at which I was diagnosed with a physical evaluation. This is 2021. I’m still thinking “well, its not a big deal. I can deal with the pain, now I have an answer, I can go figure it out and return to normal”. WRONG.
I have always had issues with my digestion and stomach. As I mentioned when I was younger, I had very chronic diarrhea and would often be kept home from school due to illness. In 2022-2024, I began to develope severe pain after eating, what was once “normal pain” was now sharp and couldn’t be ignored. At an ER, I was diagnosed with gallstones and told that was the cause (surgery was not offered at this time). I was roughly 200-215 pounds and told to change my diet, loose weight and stop eating greasy foods. Only the other foods where causing a myriad a reactions, so I kept eating as I was before and just accepted the pain as normal.
In November 2024, I started to get really sick (sicker than I had currently felt). I began to throw up consistently, almost daily, sometimes multiple times a day. I went from 240 odd pounds to 145 in less than 8 months (June 2025) . I was told everything was fine with me, one doctor even noted in my chart that I appeared to be a “well fed individual” after I told him I hadn’t been able to keep down food for over a week!
It wasn’t until I went to the ER after going jaundice that they finally did something: remove my gall bladder. Only that wasn’t the only issue they found at the time. Kidney Failure. And they didn’t even tell me, I found out later, looking through my online test results and diagnosis sheet from the hospital. Nowhere on paper did they mention this, nor the fact that my liver enzymes are incredibly high. (I understand that their job is to treat emergencies and that a PCP should always be followed up with, but you’d think just once in my 4 day stay that they would have mentioned it.)
Immediately following my surgery and release from the hospital, I was readmitted after fainting later the same day. My resting heart rate after arriving at the ER was 169. After testing and a little more time spent watching hospital tv I was diagnosed with Postural Orthostatic Hypotension. After my stay and during my recovery, this definitely worsened, at one point lifting my head up would result in a BP crash. (I have had issues all my life with presyncope, blurry vision and numbness upon standing for years, I suspected POTS but hadn’t gotten into with a cardiologist at the time). This is my most recent diagnosis, with a few on the backburner awaiting further testing.
My biggest issue currently (aside from severe light headedness and fainting occasionally at work) is my digestion. I have suspected Gastroparesis (awaiting testing) and what was an already limited diet has become nothing but liquids, meal replacement shakes and applesauce. I still experience pain after eating and as it moves through my digestive system, and an issue with actually engaging the muscles “back there”. What used to be a passion for food has turned into bitter resentment, I’ve come to hate the ritual, having to force myself to swallow so that I might receive the nutrional content of what I’m consuming, or throw it up trying.
I have an endoscopy and a colonoscopy scheduled in two days, hopefully that will bring more answers.
I apologize again for the long story. I haven’t actually had a chance to write about the journey and, even if it may not appear so, there is a lot still missing. I have issues in almost every area of my body. I just want to feel “normal” again. I understand that what I had and where I was may not be obtainable, but id like to feel content at least with where I am in life. I’m 24 years old, I walk with a cane and outwardly I look healthy which tends to lead very uncomfortable situations with people believing in either faking or not sick enough to depend on a mobility aid/be receiving medical care (and its disgusting, why would you go up to anyone and tell them you don’t believe them or they aren’t sick enough. That its for attention. I hear this a lot in the gastro-waiting room).
And anyway, thank you if you did read this far. :)
#Gastroparesis #GastroesophagealRefluxDisease #PosturalHypotension #EhlersDanlosSyndrome #MastCellActivationDisorder #ChronicIllness #AutonomicDysfunction

Our next #Maladiemon is Spew Spew! People living with #chronicillness often get #nausea from their condition or medicines. #gastrointestinal problems like #Gastroparesis , #UlcerativeColitis , #CyclicVommitingSyndrome , and #crohnsdisease all collect #spewspew as a symptom.
Crohn’s and Colitis Foundation: www.crohnscolitisfoundation.org

Hi, my name is SassyKatie95. I’m here to learn more about what I’m going through and build connections
#MightyTogether #Anxiety #Depression #BorderlinePersonalityDisorder #ADHD #Migraine #AutismSpectrumDisorder #Gastroparesis #Dysautonomia
Hi, my name is adhdandme.
Hi, my name is Rae. I'm here because I have a lot of chronic disorders. I’m only 23 and it is almost impossible to live. Every year I get diagnosed with something new. I don’t know anyone like me. I know people who have the individual issues and disorders. But I’ve never met or talked to anyone who struggles with everything. I just want to know more about these things and how to deal with them. I came from nursing but it’s different to be in it. It’s also taken over my whole life to where I cannot work. I pass out consistently. I just need someone who can understand some what.
#MightyTogether #Anxiety #Depression #Migraine #PTSD #EatingDisorder #OCD #EhlersDanlosSyndrome #Dysautonomia #PosturalOrthostaticTachycardiaSyndrome #PolycysticOvarySyndromePCOS #Endometriosis #Gastroparesis #HypothyroidismUnderactiveThyroidDisease #CeliacDisease #IrritableBowelSyndromeIBS #Grief #Epilepsy #Arrhythmia

I got my CWD (Children with Diabetes) award for 25 years of type 1 diabetes! Just wanted to share this milestone. It was weirdly emotional to get the medal in the mail and be recognized for one of my hardest invisible battles. 💙
And no, I did not eat too much sugar as a kid. It was a total coincidence being diagnosed on Halloween! Type 1 diabetes is an autoimmune disease. 👍
*Been asked that question soooo much* 😅
#DiabetesType1
#Fibromyalgia
#ChronicFatigue
#PolycysticOvarySyndrome
#InterstitialCystitis
#ADHD
#Depression
#Undiagnosed
#GastroesophagealRefluxDisease
#IrritableBowelSyndromeIBS
#Gastroparesis
Come forth Lazarus!
Come forth Lazarus!
Wrapped up just like Lazarus,
Bound down in decay.
If He would have come sooner,
would life have gone that way?
They thought it was over;
But that’s when Jesus came!
He cried out for Lazarus;
With a shout, He called his name.
And He said,”Come forth, Lazarus”!
“You’ve been dead four days;
Take off your bandages,
your life is gonna change!”
Come forth, Lazarus!
Jesus freed him from the grave!
Come forth Lazarus.
You came back from the dead-
Set free from the pain.
Come forth Lazarus!
Jesus freed you from the grave!
Come forth Lazarus!
Be free from all your bandages!
Your life is gonna change.
In Jesus name!!
Breathe again!
See the “Come Forth Lazarus”
song/video available on my
YouTube:
Melanie’s Melody
along with many other inspiring songs/videos. Enjoy and God Bless your health journey!
We CAN come back to life, and have our own resurrection experience. Maybe in different ways with health issues, but there is Life in Christ!
#ChronicIllness #ChronicInflammatoryDemyelinatingPolyneuropathy #ChronicPain #InsideTheMighty #PrimaryImmunodeficiency #PosturalOrthostaticTachycardiaSyndrome #MitochondrialDisease #Gastroparesis #MightyPoets #MightyTogether #CheckInWithMe
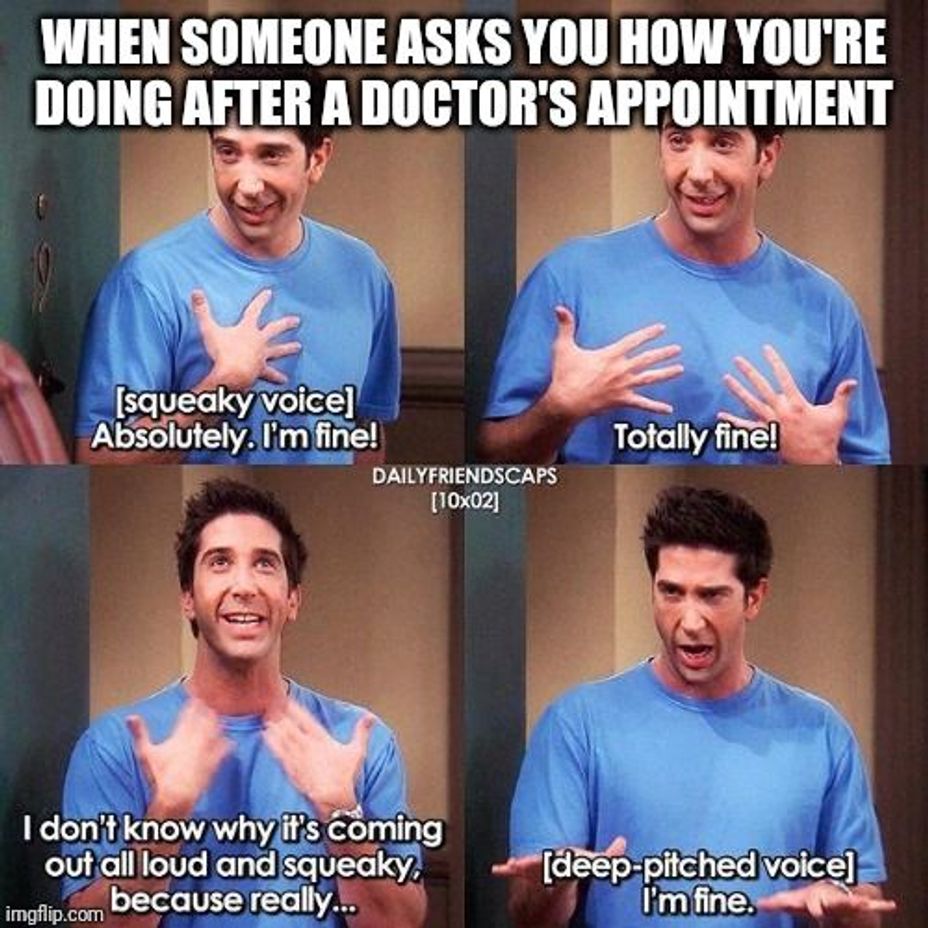
Exactly how I felt off my last appointment, but add to that extreme anxiety that made me physically sick to my stomach with the WORSE headache I ever had and feeling like screaming and crying and bundling up in a ball in my bed covers over me and just not participating in life for a bit... That's how I felt because I got diagnosed with yet ANOTHER autoimmune disorder... #autoimmunedisorders #SjogrensSyndrome #InflammatoryBowelDiseaseIBD #Gastroparesis #Gastritis #Colitis