I’m new here!
Hi, my name is PAHJolie. I've been diagnosed with
#MightyTogether #PulmonaryHypertension #PulmonaryArterialHypertension #breathtakingawareness
Hi, my name is PAHJolie. I've been diagnosed with
#MightyTogether #PulmonaryHypertension #PulmonaryArterialHypertension #breathtakingawareness

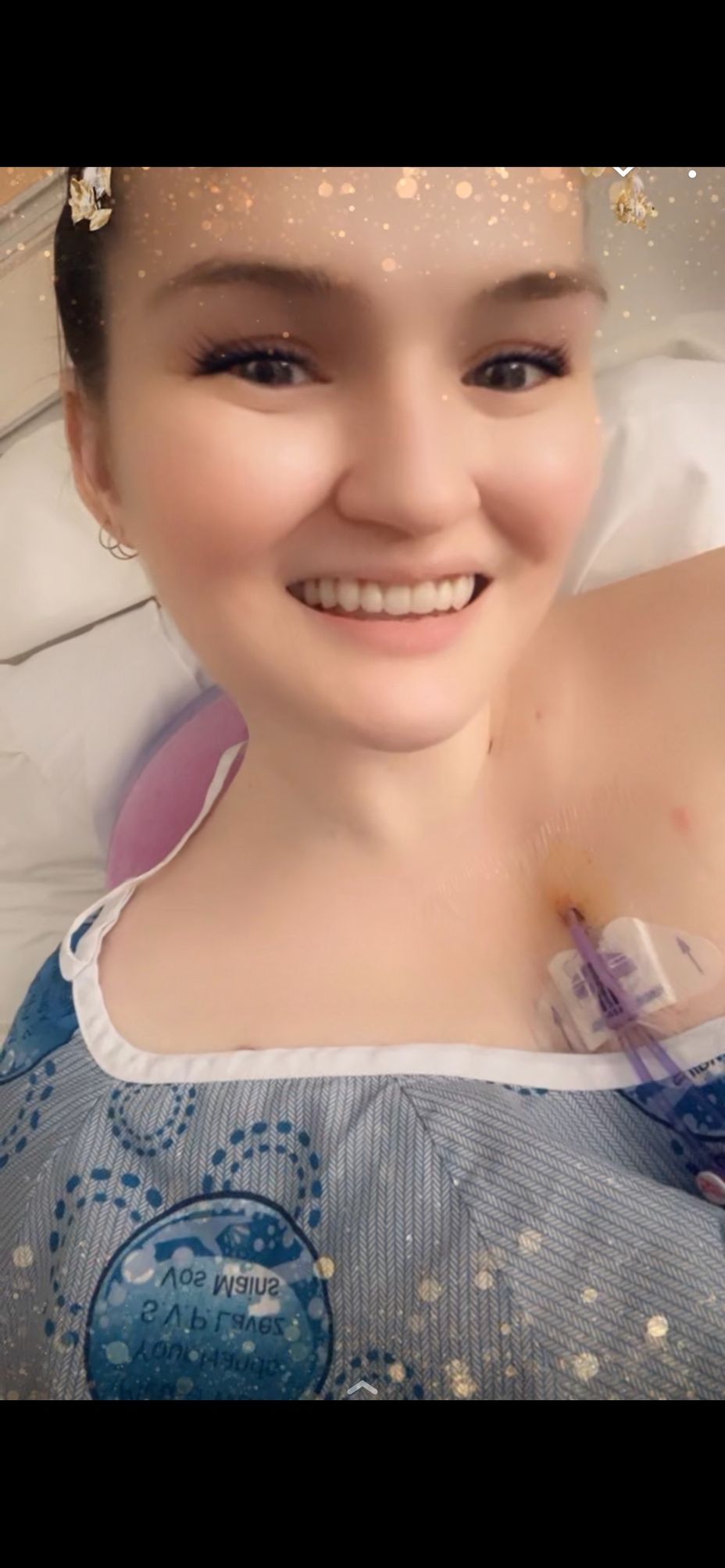
We sent all my medical records to UCSD and it was a huge surprise they told us I could also get a quote for a PTE. I really didn't want to get one even when it was possible, because I knew it is a very risky procedure, your chest gets opened like a hot dog, you basically get killed for several minutes in a hypothermic circulatory arrest.
So we ignored the quote and just postponed the decision until one day Olga Cesena from the international department of UCSD called us directly and explained everything to us. She said that in Mexico it wasn't possible to do the PTE, but in San Diego it was, that they are more capable than anyone in the world and the mortality rates were about 1% , impressive considering anywhere else in the world the lowest mortality rates are about 15%. She also said that a BPA was possible but for my specific case it wouldn´t really make big improvments, the PTE was the way to go.
To get the PTE wasn't an easy decision, I was really afraid of dying, but we asked doctors here in Mexico their opinion and said it is the best decision I could take. My family was right all the time. When you're making life changing decisions such as choosing procedures and hospitals it's important to have other people help you find alternatives and show you the best options. We were told by Dr Madani and Dr Kim said it was very good i haven had any BPA before it would have been more difficult to perform the PTE, also that BPAs are not for young patients. So far my parents made perfect choices.
During my PTE I was in hypothermic circulatory arrest for 77 minutes in total, several more than other patients. Now I laugh about people that pretentiously say they have been clinically dead for 3 minutes. Dr Madani expected it to be of an average complexity but to his surprise he faced a challenge with my case.
Following the surgery, he remarked that he rated the difficulty level as a 9 on a scale of 1 to 10, with 1 being the easiest and 10 being the most difficult PTE he had ever performed. Typically, patients are able to resume eating and walking the day after surgery, but in my case, it took me 5 days before I could walk again.
Now it has been two months since the surgery and I feel amazing. I feel so much energy all day , I even started to run. Yesterday I ran and walked a 5k in 50 min. I often say to my mother Dr Madani gave me superpowers. Certainly it feels like superpowers, so much I just signed up for the San Diego Marathon 2024. I know I have a long way before running 42 kilometers but it has been my goal since the intensive care unit.
I want to give my medal to the UCSD team and show them how they gave me back my burning desire to live. Not enough can't be said about how good Dr Kim, Dr Madani and their team are. I always tell people I got presidential quality open heart surgery, and sure it was, my scar is barely visible now and it never hurt bad at all.
So now my CTEPH journey is over and I feel responsible for making awareness of this disease so no one else has to live like me for 7 years ignoring there is a cure. I also feel part of the community of people with Pulmonary Hypertension due to other causes I know, just like the PTE there are potential cures being developed. I know maybe 20 years ago a surgery like this wouldn't have been possible but we have people like Dr Madani and Dr Kim who push the boundaries and make modern medicine miracles.
#cteph #pte #ucsd #PulmonaryEmbolism #pulmonaryhypertension #PAH #APS
This statement is how I am currently feeling about my Mental Illness disability. It started at first at age 19 yrs old when I was an administrative assistant in a company in NYC and I wanted a higher position and was told no due to me not being of same race. So I quit and started working for law firm and just completed my paralegal certification. But yet, I was working as a clerk! I noticed first hand how my anxiety was kicking in. Ears hot heart pumping anger at its peak. I heard stuff only I hear and I was told by my mom I just stressed. Ok years went by I changed my career after several quitting episodes at different law firms and even started my own business . Now Ms Anxiety had a friend called Ms Stressor and sidekick Ms Depression who loves to hangout with the jokester Ms Boarderline Personality Disorder. I hope you all are following me thus far. Now I live in new state n raising 3 children and working 3 jobs away from my main support my mom. Because of all this I had to change my career 3 times and had 2 divorces under my belt. Now I am on disability for first time and I was angry 😡 at the world around me. I was introduced to inpatient and IOP and PHP and ACUTE PHP. During this phase in life I was giving up at age of around 30s. Here is Ms Suicidal Ideation with Sassy Auditorio and Haluscenary with OCD yup!! Good ole Pyschescefenia I still can not spell it smh. But I brushed myself off and change my career again after 5 yrs on disability . I continued with therapy and now my life puzzle and lite at end of tunnel was bright and I pushed myself and helped others. I learned Coping and acceptance and Recovery Wow!! This easy! Now I am in EMDR and DBT and Cognative Therapy and a provider too!! All these years I was angry because the people who wanted to be my provider learned it from books!! Here I am a consumer and learned more from books and education! Yup career change again but for purpose. Now it’s during pandemic and have adult kids n grandkids and at best job ever helping my community and getting paid to travel! Now it’s 2022 and that wrench 🔧 was tossed at my life once again!!! My disability have new names, PTSD and Childhood Trauma and Orthopedic issues and Pulmonary Hypertension and it’s hello Oxygen!!! But I say this, I may be temporary down but I will be back!!! 😉 #careerchange
Night time is probably the worst. Anyone else up? Let’s talk! :)
#ChronicIllness #SpoonieProblems #Spoonie #Gastroparesis #EhlersDanlosSyndrome #MastCellActivationDisorder #ChronicIntestinalPseudoobstruction #PulmonaryHypertension #PulmonaryArterialHypertension #Painsomnia
What’s worse than insomnia? Painsomnia.
Anyone else up and want to talk? Send me a message , let’s be friends :)
) #Insomnia #Painsomnia #Cantsleep #Gastroparesis #EhlersDanlosSyndrome #IntestinalPseudoOnbstruction #PulmonaryHypertension
I’m new to this app, I’m hoping to meet people who have similar illnesses and struggles, it’s hard finding anyone who can really understand what it’s like. Adding all my hashtags hoping that I’ll meet people going through the same things I am!if anyone wants to chat shoot me a message :) #ChronicIlless #Gastroparesis #PulmonaryArterialHypertension #PulmonaryHypertension #HeartTransplant #LungTransplant #heartfailure #MastCellActivationDisorder #EhlersDanlosSyndrome #HickmanLine #FeedingTube #Gtube #PrimaryImmunodeficiency
Pulmonary Hypertension and Scleroderma patient Nola Martin discusses her road to diagnosis and the importance of support groups and seeing a PH specialist.
My name is Nola Martin and I’m from Philadelphia, PA, and my journey with PH started about nine years ago.
I was actually at work exercising one day. I was so excited. We moved to a new building. They put a gym in for us, and I’m on the treadmill for not even two minutes, and I could literally feel my feet swelling in my sneakers, and I’m going, “Well, this is weird.” I was having a lot of shortness of breath, but I kept making up excuses. “If I diet and exercise more. Maybe if I lose a little weight, I’ll feel a little better.”
I was eating one orange a day. That was my meal for the entire day and it felt like I had a full course meal. Of course, I didn’t share this information with my doctor right away because, in my mind, I’m going, “Oh, diet and exercise more.” But how much more can you diet when you’re only eating an orange a day?
I got up to walk to the printer which was less than a foot from my desk, and it literally felt like all the oxygen was sucked out of the room. I called my doctor at the University of Penn. She’s like, “I think you need to be seen right away. Are you able to drive? Can you come in?” I’m like, “Sure, I can come in.” But I didn’t tell her I was at work which was an hour away, but I drove to the hospital and when I got in, they put a pulse ox on me and they’re like, “Okay, let’s see if you can walk around this desk.”
I took literally five or six steps, and all these alarms started going off. The next thing I know, they’re putting oxygen on me. They put me in a wheelchair. And she’s like, “We’re not even going to wait for transport.” They just wheeled me into the emergency room.
And that’s when I start hearing things like #PulmonaryHypertension, and I’m getting an echocardiogram and oh, you’ll need a right heart catheterization. I didn’t understand any of this stuff at all. But that began my journey with pulmonary hypertension. And from that, I found out mine is due to #Scleroderma. And in addition to the scleroderma, then it’s like, “Well, now you also have congestive heart failure” and I have GERD real bad, and I have Raynaud’s and all of these other things.
At first, when you first hear this and you go on the internet … most people want to google things and find out, because Google was the answer for everything. And I went onto Google and searched, and it was like oh, well you may have two to three years to live and you go through the whole depression thing. I said, “Wait, just let me talk to the doctors. Get my appointment, see what’s going on.”
I discovered through that support groups, which was a wonderful thing because I got to talk to people who understood what I was going through. It’s hard when you’re trying to explain something to somebody else when you truly don’t understand it yourself. I learned a lot of information about support groups, about making sure that you are at a hospital or center or have a doctor that understands pulmonary hypertension and that can treat you.
Because everybody has their own history and their story with pulmonary hypertension, and it may not be the same as yours. It’s very important, first of all, to make sure you get a good doctor, you get good treatment going, and that you learn the disease yourself and learn how it affects you personally.
Read the full story: I’m Aware That I’m Rare: Nola Martin (252)

Canadian pulmonary hypertension patient, Stacy Physick was diagnosed with PH in 2011. She immediately got her affairs in order, believing she only expected to survive 1-3 years. Now, 10 years post-diagnosis she shares her journey and her conscious decision to lead a normal life.
My name is Stacy Physick and I’m in Chilliwack, BC, Canada. It took a while for my pulmonary hypertension diagnosis. I actually didn’t start medication until 2011. My connection to PH is they believe it started because I had shortness of breath and a bunch of different symptoms, and I had a bunch of different tests done. Finally my doctors decided it was PH, but what they believed it was caused from was PVOD, pulmonary veno occlusive disease. They thought that was going to move fairly rapidly with me. When they finally decided to start medication, it was just to help slow that progression, hopefully, as well as the PH progression.
I also had open heart surgery when I was four and a half years old and I’m now 63. It didn’t stem from that. I’m left with a VSD, a ventricular sepal defect. I also have a small ASD that I’ve developed over the years, but I’ve held real stable my whole life with that. I’ve always been checked by a cardiologist. So that’s really where my journey began is because of my breathing issues and shortness of breath and tiredness and things like that.
How I knew the diagnosis was happening is I see a cardiologist on a regular basis. I’ve seen him annually for basically my entire life. He started with a change in my pulmonary pressure. He noticed, and he said, “You know, don’t worry about it yet. It might be okay.” I had been at that point already identifying that I had shortness of breath. I wasn’t remembering things quite as well. I was a corporate trainer and I also did a lot of presentations, pretty much daily. I did that for a few years. As the years progressed, I started getting shorter and shorter breath trying to talk. So he had noted this pulmonary pressure increase. Then what he did is he said, “We’ll just watch it.” Then six months later, I came back for a second echocardiogram and the pressures were even higher.
Then my doctor sent me to a pulmonary specialist and that’s when they did some more testing. I had pulmonary function tests, another echo. I had a heart catheterization and that’s when they determined that, “Nope, you’ve got pulmonary hypertension.” That’s where it started from.
The whole reality at that point was kind of a shock to me because he continued to do other tests and then he did the CT scan found out that looked like I was full of PVOD in my lungs. Then the diagnosis came that’s likely what it was. We were going to treat it as that. He had done all the clinical testing he said minus the fact of a lung biopsy, which would be the ultimate check off point to say that definitively it was PVOD. Then they set me up with a thoracic surgeon and it was at that time based on my pressures too, they said it was too risky to even do the lung biopsies. So I sort of started with that.
Read the full story: I'm Aware That I'm Rare: the phaware® podcast: Stacy Physick...