Just thought I’d introduce myself 🫣
Before my illness/injuries took over, I used to really enjoy cooking— even thought about enrolling myself into a culinary arts program. However, I would eventually come to realize, through the years that it simply wasn’t meant to be.
My journey began in 2008, when I was diagnosed with multiple sclerosis. And despite having started a DMT (Copaxone), my symptoms took a turn for the worst in October 2013. One day, while showering, I got hit with an out-of-the-blue case of vertigo, resulting in a fall, which caused my lumbar spinal cord injury.
Despite my best efforts to communicate with my medical team, I wasn’t taken seriously. The only responses that my doctors repeatedly used whenever I’d express my concerns were, “Hmm… I’m not sure if this is from the MS”, or, “Why don’t we increase your medication dose and see what happens” 🙄🤕 This went on for about eight years.
By 2016, my digestive system decided that it’d had enough!!! And just like that 🫰🏾it quit on me. I’d spend the next four years shedding a drastic amount of weight, being unable to keep any food or liquids down, and frantically searching for a doctor to actually listen to me. And all I had to show for my efforts was a traumatic brain injury I’d acquired in November 2018, after having passed out, being rushed to a hospital that was close by at the time, and receiving treatment for dehydration— but not the concussion I’d sustained from having fainted, in the first place. 🙄🤨
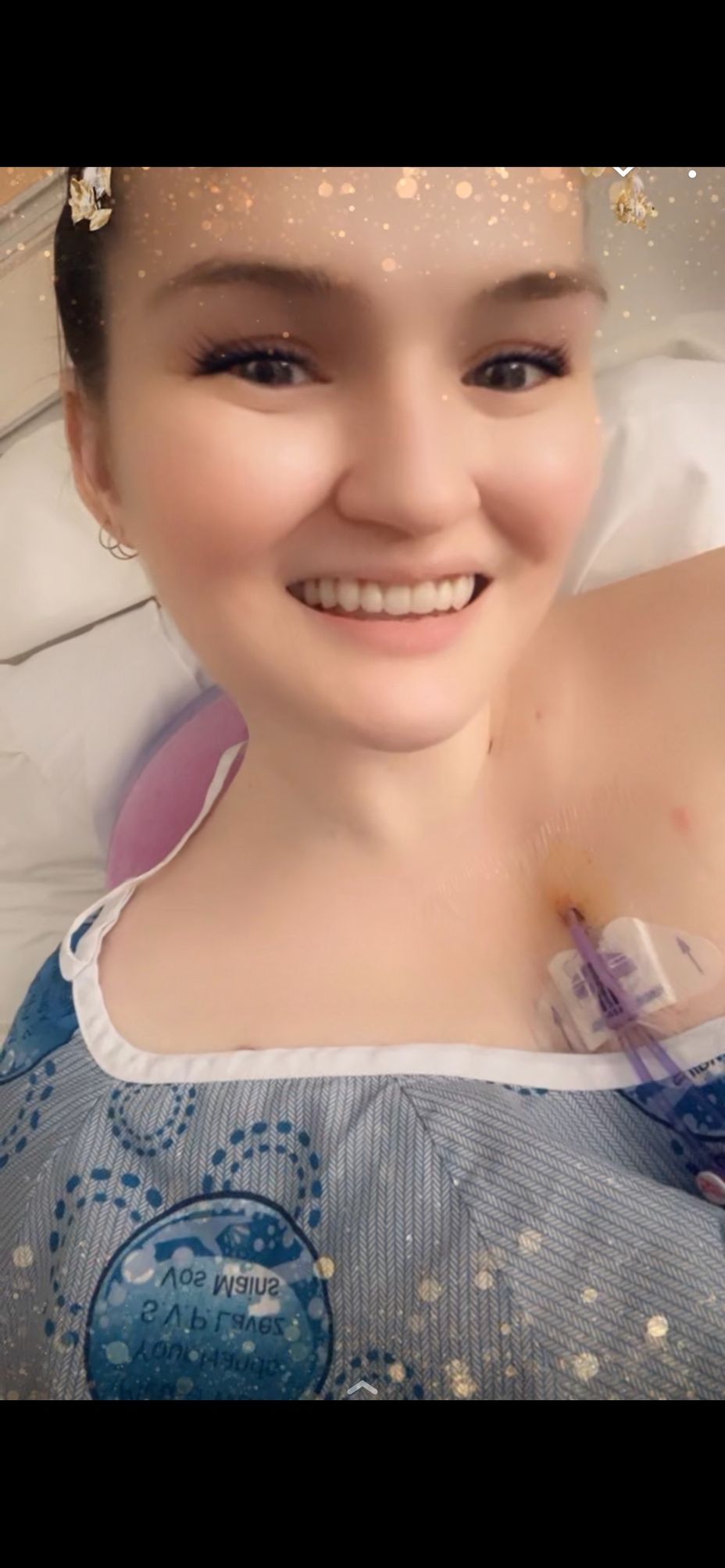
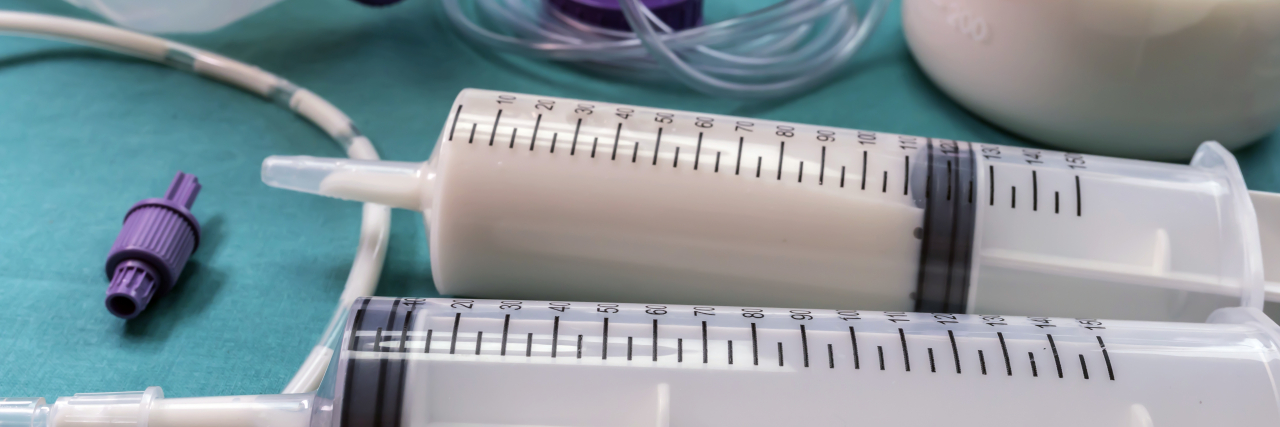
By 2019-ish, I’d finally found a team of medical professionals who were as compassionate as they were intelligent; and in March 2020, after I’d withered down to 105 lbs, I had a j-tube surgically implanted. It’s saving my life, for sure, but it still makes for a lonely existence.
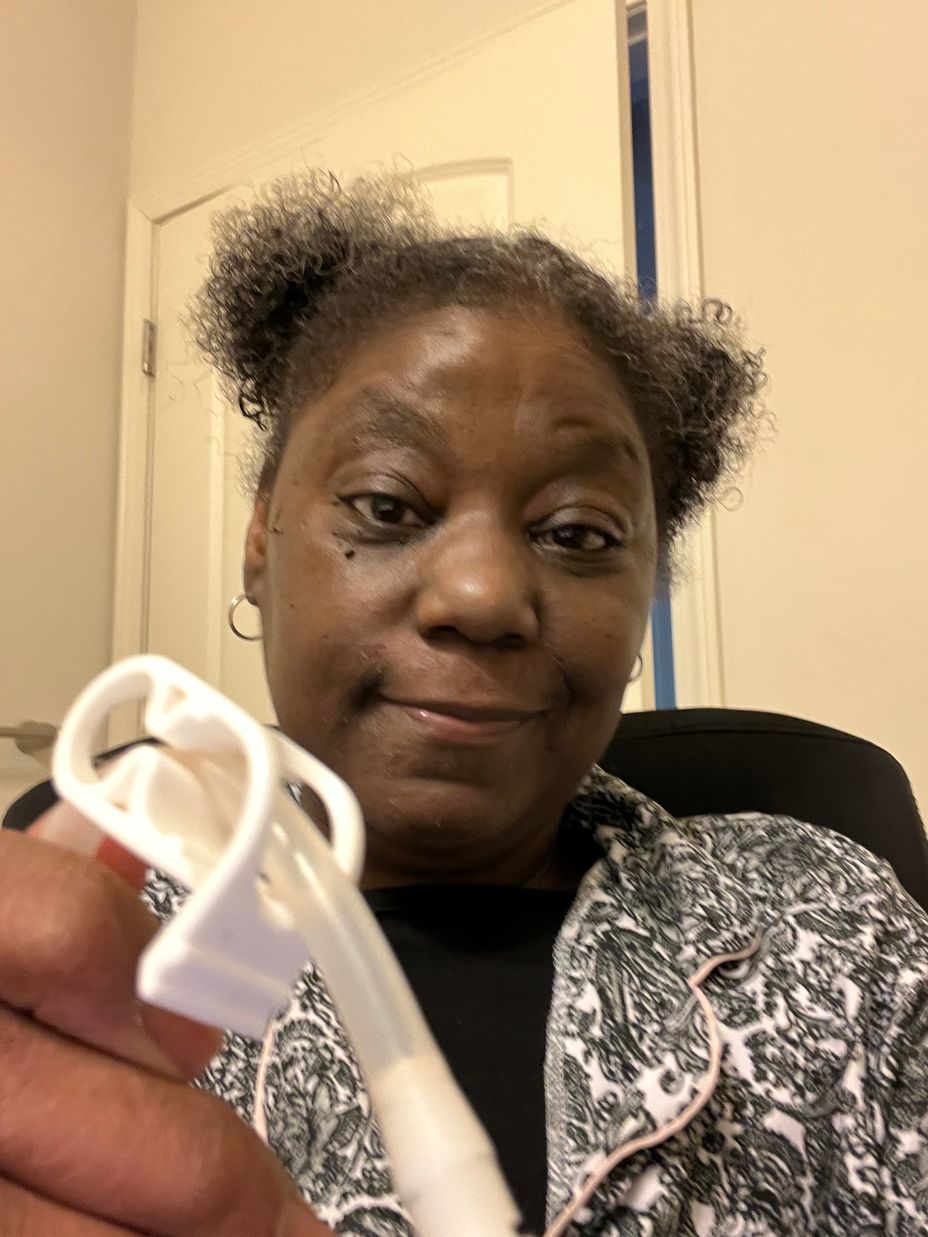
Once my digestive issues were “stabilized” (new normal = permanent), it was time for me to get the rest of my poor, exhausted body taken care of. My new neuro team placed me on Ocrevus, which helps tremendously at keeping my nervous system in line; I also have a little helper— a port-a-cath— that gives my medical team the necessary access to my stubborn veins for blood work and infusion days (it literally took a whole team of nurses, and one uncomfortable hour to finally got my veins to cooperate before my port 😳💉🩸).
Next up was Pain Management. After several unsuccessful attempts of conservative treatments (crushing pain pills and flushing them into my tube), it was decided that I would be an ideal candidate for an intrathecal Baclofen pump, which I had surgically implanted in January 2022.
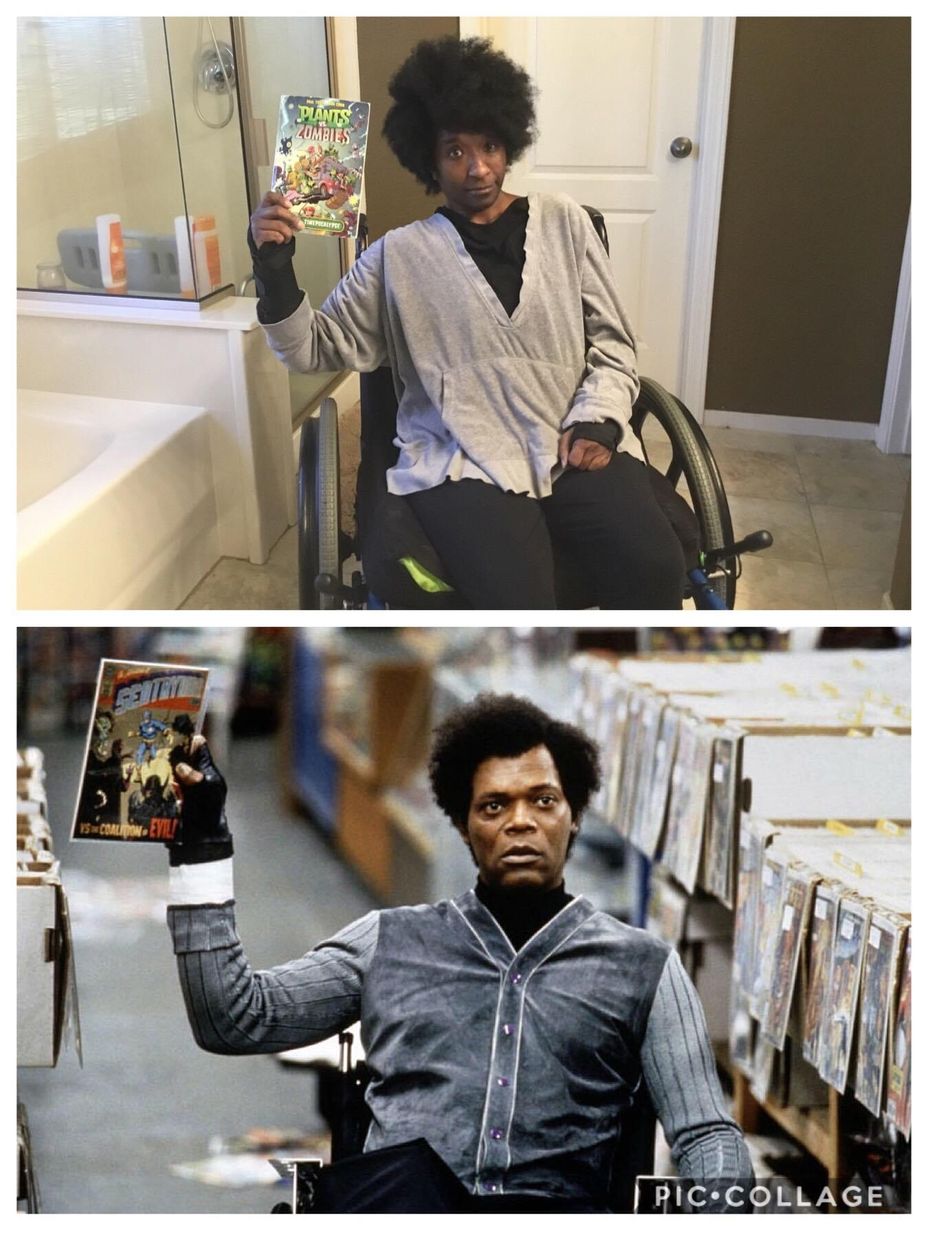
So, what brings me here to the forums? Isolation. As I mentioned previously, living life in a partially bionic body makes for a rather lonely existence 😔 After all, what are the chances of meeting someone else with MS, a TBI, an SCI, and a STRONG affinity for all things audio (unless it’s reruns of classic shows that I grew up with, documentaries, or pretty much ANYTHING to do with British TV, then nope, I probably haven’t seen/don’t want to watch whatever it is you were about to suggest 🤷🏾♀️🤣), who also enjoys Bible study, coloring, and word search puzzles? 🦗🦗🦗🦗🦗🦗🎤🎤🎤 (*ahem… um, hello… is this thing on?*)
Someone… Anyone… Bueller??? 🤓🤓🤓
Probably not… but a girl can dream, right? 😴🤣
At any rate, that’s my story. Hoping to find a lunch table to crash soon 👚👛🎀🛍💖🤣😊