I'm new here!
Hi, my name is Sophia. I'm here because I want to talk to people like me.
Hi, my name is Sophia. I'm here because I want to talk to people like me.
Hi, my name is Sophia. I'm here because I want to talk to people like me.
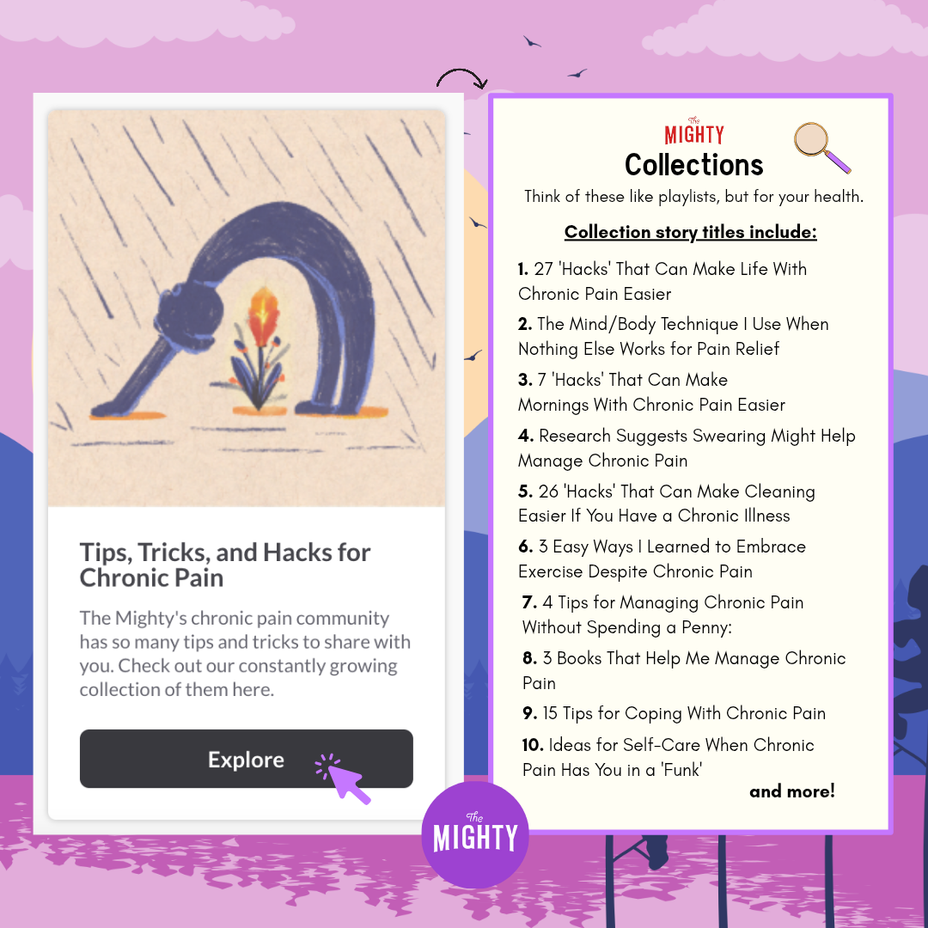
Managing chronic pain is challenging—physically, emotionally, and mentally. It can also feel isolating as you try to figure out what works best for you and your body. But discovering helpful coping mechanisms, tips and tricks for relief, supportive communities, and reliable resources can make a meaningful difference, even if just for a moment. You are not alone!
Our Tips, Tricks, and Hacks for Chronic Pain collection brings together real-life insights and practical strategies shared by people who understand. Whether you're looking for new ways to ease discomfort or simply feel seen, this collection—and our Mighty community—is here to support you. 🌟
Explore the collection here:
Tips, Tricks, and Hacks for Chronic Pain
#ChronicPain #ChronicIllness #MentalHealth #Disability #Caregiving #RareDisease #Migraine #Stroke #CardiovascularDisease #AutonomicDysfunction #POTS #Spoonie #Lupus #Endometriosis #Depression
#Cancer #Anxiety #PTSD #CheckInWithMe
Something on this platform has been bothering me lately.
People reach out because they’re suffering, but they feel ashamed of being perceived as negative and dragging others down. They apologize for “venting” or “ranting”.
I’ve turned to this community for help when I’m struggling, and I’m sure I’ll do it again in the future. I’ve been met with incredible empathy and love.
Journaling doesn’t work for me. It reinforces my pain. Reaching out does wonders.
This is a safe space. A place for affirmations, humor, knowledge, creativity, and gratitude. But also a place to lay bare a dark night of the soul.
I read an article about the benefits of expressing negative emotions by Malinda King, MA, LPCC. Some quotes:
“We cannot selectively numb or deny emotions so when we do that to our sadness, fear, and anger, we are also numbing out our ability to experience happiness, joy, and gratitude.”
“Blocked and suppressed emotions have been linked to physical problems like heart disease, intestinal problems, headaches, insomnia, and autoimmune disorders.”
“When we express vulnerable emotions like sadness, pain or fear with other people we care about, it actually creates bonding moments with that other person, making the relationship deeper, more meaningful, and intimate.”
So no, we don’t have to “accentuate the positive” at the expense of being authentic. (That doesn’t mean we have to abandon gratitude or finding “glimmers”- those are part of the picture, too).
I am so grateful that, when needed, I can “vent” and “rant” here. And I hope that new Mighties feel safe and supported when they do the same.
Hi, my name is Kpnuts123. I'm here because
Hi, my name is Kpnuts123. I'm here because
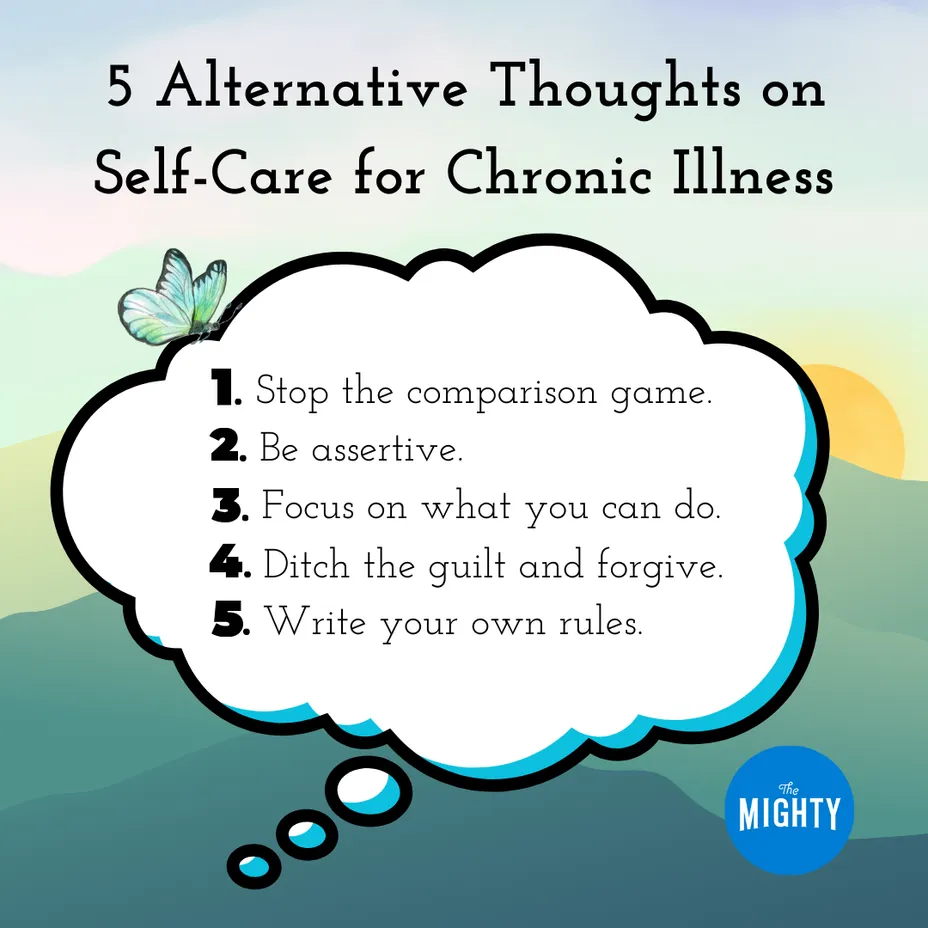
We often hear about self-care and think of it as prioritizing your needs, getting outside, taking breaks, or enjoying the occasional bubble bath. But self-care is so much more—especially when you're living with a chronic illness. There are added layers of considerations, demands, and limitations that are often overlooked.
What are your thoughts on self-care while managing a chronic illness or chronic pain? What does self-care look like for you? What do you wish others understood about taking care of your needs and health as someone with a chronic condition?
📖 Need a thoughtful read on the topic? Check out today's Story of the Week here: 5 Alternative Thoughts on Self-Care for Chronic Illness
#ChronicPain #ChronicIllness #MentalHealth #Disability #Caregiving #RareDisease #Migraine #Stroke #CardiovascularDisease #AutonomicDysfunction
#PosturalOrthostaticTachycardiaSyndrome #Spoonie #Lupus #Endometriosis
#Cancer #Anxiety #PTSD
#CheckInWithMe

Hi, my name is Tenngirl31_. I'm here because
Hi, my name is Tenngirl31_. I'm here because
Hi, my name is gwenmayes. I'm looking for people who share my experience of living with genetic mutation that causes heart disease and the associated anxiety of palpitations, atrial fibrillation and irregular heartbeats.