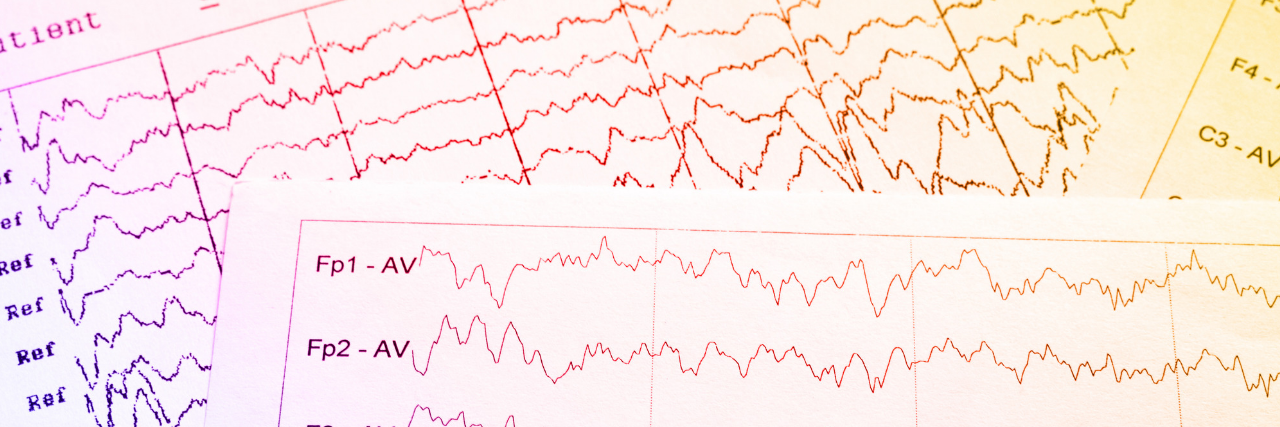
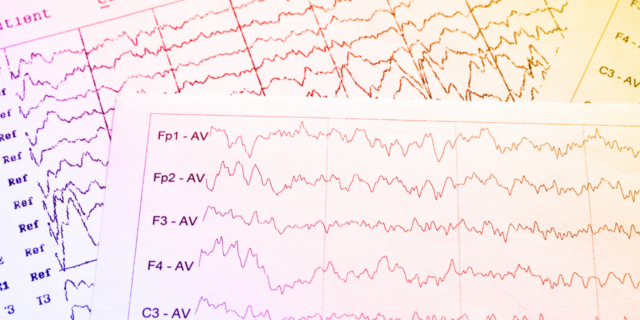
About 2 months ago I started seeing a new Neurologist...I've been having migraines since I was 7 and having seizures since I was 8...Having been twelve years since I began having seizures I still wasn't technically "epileptic" (as my former neurologist didn't believe I was)...My new neurologist then suggested a five-day epilepsy study and I happily agreed (as maybe I'd finally find something out)...And the results shocked me.
After the first day of my study, I expected my neurologist to say I was seizure-free (as I didn't feel like I had any that day), but I found out that I was having small 1-5 second seizures very often throughout the day, and having much longer 30-60 second seizures while sleeping!!
After the study was over she told me there was zero argument, I was epileptic...And even though we didn't find a trigger for my seizures, it was still somewhat comforting to know that I had proof of my seizures (as I've been doubted by nearly everyone)...The only thing left is finding out when I'm having these seizures (as I don't even notice) and then finding out what is specifically causing them...