I'm clumsy. I've always been clumsy. People are terrified of telling me to take a break because I do. I break cups, glasses, plates - you name it. They nicknamed me Zorba the Greek, one place I worked because of this. Talking of jobs - with me they've always been few and far between. nothing lasts long. I either get bored and leave or get sacked.
"Now look what you've done!" or "What happened to that order I gave you, to send out to Mr Harvey on the eighth?" (Well he didn't specify which month, did he?).
To say I was socially inept, is mildly true too. If I had a drink in my hand, I'd either drop it or spill it on someone.
"You clumsy idiot!" (Well yes, I know that - can you be more specific or add something else of interest to that point?).
I was never a great talker and got on better with kids and animals, than I ever did with adults or the human race altogether.
"Stop grimacing at me you nutter!" And other plaudits like this, would come my way. Talk? How could I? I could barely get my body to work, let alone my brain. Occasionally I'd let slip a terrible pun, to break the ice, in social situations. Every time I tried to be clever, an uncoordinated load of stumbling rubbish would come out.
"What do you mean, I-I-I, ig ag ooh?"
Ruthless Mickey takers at work or down the pub, would plough right into me as soon as I opened my mouth, so I shut up again or I'd burst into hysterical laughter as I found the joke funnier than anyone else.
"For Christ's sake shut up! The joke's over!"
Then there were the times I couldn't understand what anybody else said. It was like that Far Side cartoon - What you say and what a dog hears:-
"Blah, blah Rover. Rover blah, blah."
It was like I was hearing a foreign language or none at all.
"Cat got your tongue? Well it bloody should have - you don't use it enough, to need it!" (Ha-ha - very funny I thought but couldn't stand the humiliation of trying to actually say it).
Hugh and Milly Asian? Now that's a couple I know well! Yes, my literal sense of humour categorised me as autistic, even if nothing else did. Then there was phonetic spelling.
"That's not how you spell it Wright - get a dictionary!" ( Wright, wrong again! School, who needs it? If they want to spell it that way, why can't they say it that way too? It's all so jumbled up and illogical!).
There's some legend that says having Asperger's makes you a mathematical genius - not me. On the way to school I obsessively count the telephone poles, yes but I couldn't add up to save my life or yours, when in the classroom. Oh yes, the stories of us being selfish and self centred are true. We live in our own little world and you can't enter, even with a valid passport. Our borders are closed Mr Schickelgruber and nobody can come through without our express permission, so turn your tanks round and go home.
We are a strange mix of contradictions - egotistical, blunt in our speech, when we do open our mouths. Bloody minded and stubborn, yet fearing confrontation because in a fight, we wouldn't know when to stop - at least that is what we believe. It takes a hell of a lot to get us going and just as much to put the brakes on: Quick to anger, slow to cool down and come back into Earth orbit, if we don't miss it altogether. Innocent, vulnerable, trusting and blundering. It is this openness and honesty that turns us into the brainy creature we so often are. While others play about in the classroom or outside it in the playground, developing their social skills through interaction, we shut up, sit still and, look and learn. We shut them out and let the light of understanding in. Ordinary people connect with the outside world, through talk and physical contact - not us. We are geeky, clumsy and inappropriate in our comments and movements but we connect internally with ideas. They can dance, play football, cake on make up or make cup cakes but not us. Books are our only friends - failing that our computer screens are. We'd rather text than talk, write and read rather than speak - even to each other. We want to know how the universe works and maybe even one day, we'll find out how we work but not today, oh no, not today...
We know we are not liked - even feared and despised by some people or why attack us? (You only bully what you're afraid of - what challenges you to be what you are not or at least makes you think about it as a subject). Limited intelligence, criminality and defensiveness go together - leading to ignorance and suppression, by those wanting to shut out the light. Perpetual motion and emotion, keeps them on the move but not us. We don't want to leave home or even go out. We just want to collect our train numbers or plonk about on our computers in peace. Failing that we want to vegetate in front of the goggle box. We are not active participants in life. We are just passive viewers, along for the ride (Don't ask us to drive -we're not up to it or up for it either). We understand sound and motion go together (as with music and dance) but we are detached because we are observers of life, not activists (We don't move with the times because we are lumps of rock - orderly and controlled, not relaxed). We see only chaos and confusion in the world - danger we are not ready to face. Go for a swim? No thanks! You could drown and then there's all the pollution in the sea and God knows what in the rivers and swimming pools! We don't enjoy our lives, we study them for that great examination in the sky, when we all kick the bucket (Did we do well?). Live our lives? Maybe next time. Spontaneity is for wimps - we love routine. Order and discipline, that's us.
We're not in our bodies but always outside, looking in. This explains our odd gait as we're not in contact with life or society's natural rhythms.
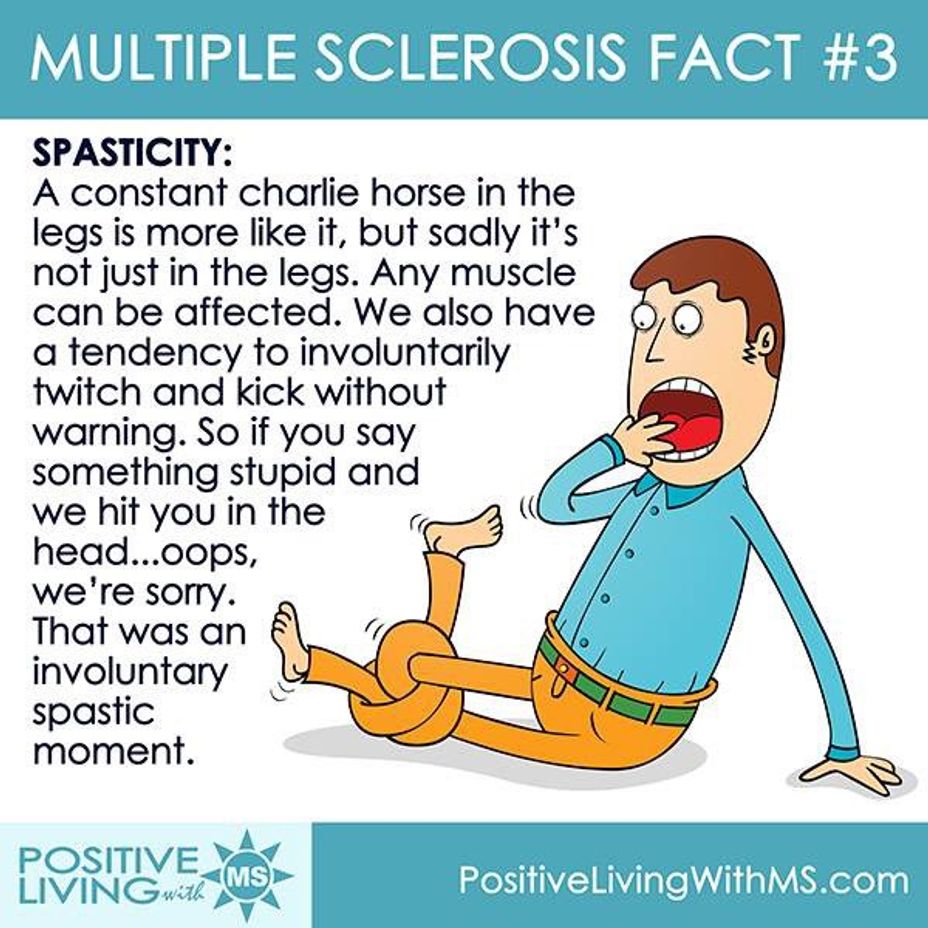
We feel continually under stress because we are. Our twitching, tics and odd mannerisms show this. I need to crack my joints continually because of this (neck, between the shoulders, lower back (especially this point), ankles, knee caps, wrists, fingers and toes - by the way did I mention we're obsessive list makers?). This is why you'll see me and others like me, suddenly tilt their heads to one side or move our hands and feet into strange positions, for no apparent reason - we need to relieve our spasticity (Perhaps this is where 'Jerk' comes from as an insult?). It could explain the difficulty swallowing, indigestion, sensory sensitivity and allergies as well. Maybe too, it explains the dietary fads of eating nothing but a particular food - like crisps, beans, bread or biscuits, for months, even years on end (I've heard that we're carb eaters, avoiding protein and choking on fats).
Is it any wonder that we're stressed? Our attention to detail driven characters, fear of making mistakes, rigid personalities (love of tight clothing), passion for order, discipline and routine - all contribute to the pressure we feel under and put ourselves under. If we weren't so visually orientated, we probably wouldn't be so language impaired, continually swallowing nervously in social situations. This passivity and receptivity is probably what allows us to be so logical but it also leads to the need for space and the temper tantrums that follow, should we not get it and find we cannot cope: The sensory influx that drives us insane - the obsessive compulsion to wash our hands and protect ourselves from every other potential danger , turns us into an explosive powder keg of emotions, which blows up like a volcano every so often.
They say it is a male thing - this turning down and in, in curiosity, then up and out with answers and insights. This mental pressure is the same as physical pressure as in sex and other expressions, I believe. The physics of it is male concentration versus female dispersal of attention and energy. This is why males are more volatile and suspicious because of it (wound up and easily triggered into