In January 2021, I became ill in ways that defied explanation. My body, which had always been a mess and a mystery, turned into a battlefield where everything seemed to go wrong at once. My symptoms were baffling to local doctors, and despite countless tests and evaluations, no one could provide answers. It was then that I made the decision to seek care at the Cleveland Clinic—a place known for its focus on complex medical cases.
Walking through the Clinic’s halls felt like stepping into a different world. There was a level of expertise and attention to detail I hadn't experienced before at local hospitals, where I often felt like a burden—someone too difficult to treat. Cleveland Clinic is a specialty hospital, attracting some of the best minds in the world, especially in rare diseases and complex conditions. Here, I wasn’t dismissed because my case didn’t fit neatly into a box. Here, I was seen.
From 2021-2023, I would spend hundreds of hours in doctors’ offices, undergoing test after test: MRIs, CT scans, bloodwork, autonomic testing, genetic panels, endoscopies, and more. My appointments bled into each other—GI, vascular, neurology, rheumatology, and cardiology—all working together to put the pieces of my medical puzzle into place. It was at Cleveland Clinic where I was finally diagnosed with a cluster of rare conditions: hypermobile Ehlers-Danlos Syndrome (hEDS), Postural Orthostatic Tachycardia Syndrome (POTS), Mast Cell Activation Syndrome (MCAS), Superior Mesenteric Artery Syndrome (SMAS), Nutcracker Syndrome, and gastrointestinal dysmotility. My body, a connective tissue disaster, was now mapped out with labels that explained why it had been betraying me for so long.
It wasn’t just about the diagnoses, though. It was about the process—the wear and tear of being a full-time patient. Each appointment chipped away at my mental and physical strength. I adopted mobility aids slowly, first a cane, then crutches, and eventually a wheelchair. It wasn’t until then that people started seeing my disability. Before the mobility aids, I existed in that liminal space between visible and invisible disability—a place where I looked “fine” to outsiders, but inside I was constantly battling a body that refused to cooperate.
In the fall of 2023, I went out on Disability. It felt like a loss, but also like a surrender to the reality of my situation. My body could no longer keep up with the demands of the world. And while that decision was incredibly difficult, it was necessary. The transition from the workforce to a life dictated by medical appointments was both jarring and isolating. Being a rare disorder patient is profoundly lonely. Local hospitals often hesitate to treat patients like me because my conditions are so specialized, so misunderstood. Cleveland Clinic, on the other hand, embraced the complexity.
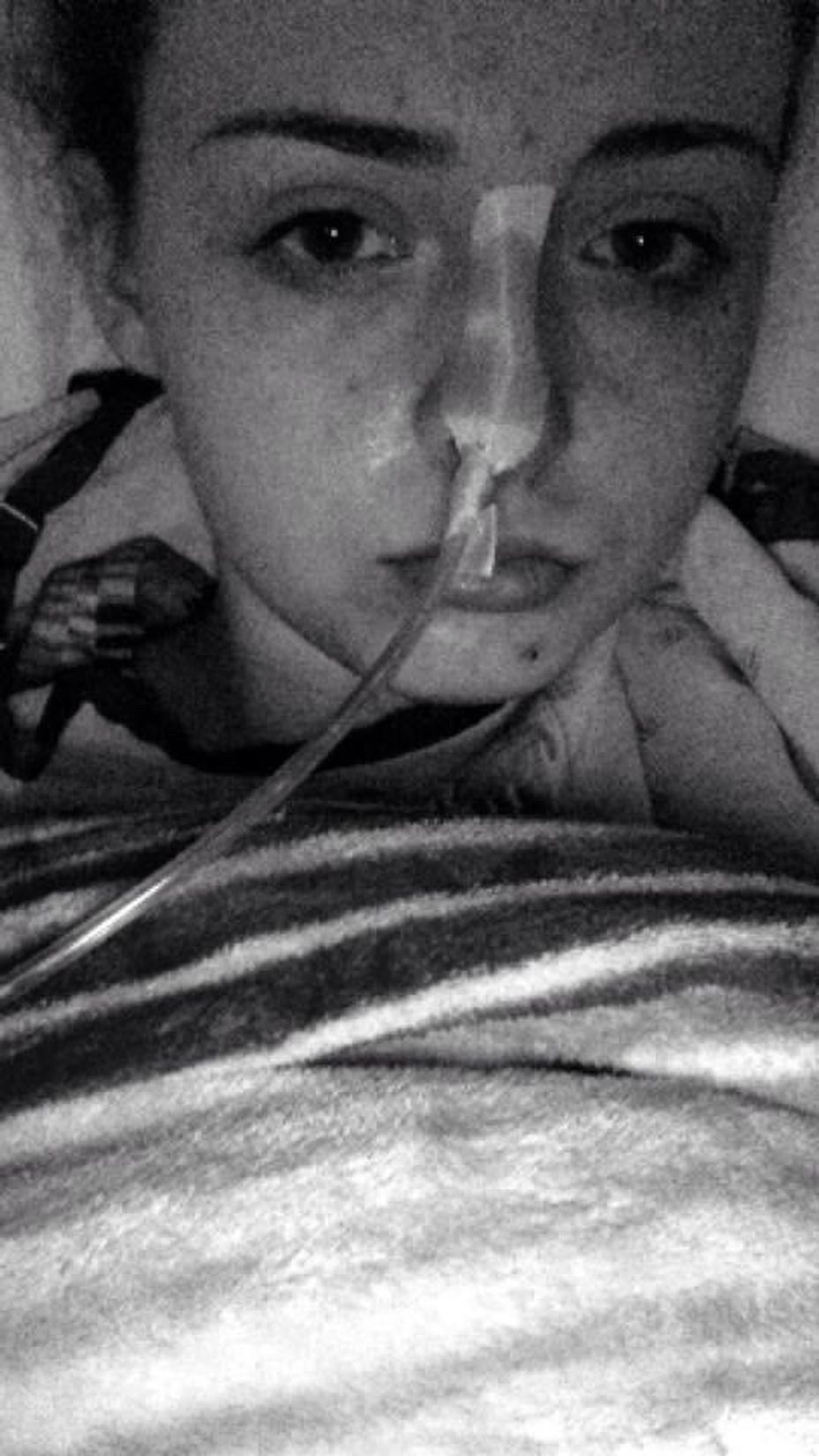
I had multiple extended hospital admissions during that year, and each one felt like a lifetime. The mental toll of lying in a hospital bed for weeks on end, facing yet another abdominal surgery, was crushing. I lost count of how many times I’ve had feeding tubes placed, how many surgeries to repair my gut, how my once active body has been systematically taken apart and pieced back together. It was there that I had a total proctocolectomy—a surgery to remove my colon because its nerves had died and a duodenojejunostomy to relieve my SMA. These surgeries left me with an ileostomy, a permanent bag attached to my abdomen that collects waste. Each surgery came with its own set of physical scars and emotional wounds.
Living as a rare disease patient has taught me more than I ever thought possible about advocacy. The medical system is not designed for people like me—people who have conditions that most doctors have never heard of. There were countless times when I was told, “Your labs are fine,” or “It’s just anxiety,” but my body knew better. I learned to trust myself, to demand better care, to not take “no” for an answer. Every day that I wake up and face this uncooperative body feels like a victory. These are small health victories, yes, but they are victories nonetheless.
I’ve learned to take pride in those victories, even when they feel small. Every successful surgery, every day without a flare-up, every inch gained in physical therapy is something to celebrate. Being a patient—full-time, relentless—has taught me resilience in ways I never imagined. It has also taught me that the best care often means seeking out the right doctors, the right specialists, and not settling for less. Cleveland Clinic has become a lifeline, a place where I can be heard and understood, where I’m not reduced to just my symptoms. The toll of being a rare disease patient is profound, both mentally and physically, but it has also given me an unshakable strength.
Still, the isolation remains. It’s difficult to find others who understand this journey. Most people can't fathom what it’s like to live inside a body like mine—a body that feels like it’s 100 years old when I’m only in my 30s. But through it all, I’ve found a community of others with rare disorders, people who understand the loneliness, the grief, the resilience required to keep going. These connections, though few and far between, are everything.
My journey at Cleveland Clinic is far from over; there will be more surgeries, more admissions, more moments of despair. I’ve had to learn to advocate for myself, to push for answers, and to find strength in a body that continually tries to defeat me. But at the Clinic, I’ve learned to trust doctors again. I’ve learned that there are medical professionals who care if I live and how well I feel. They’ve never stopped fighting for me. More than just saving my body, my doctors have saved me. I’m determined to live a life worthy of what they’ve done for me.