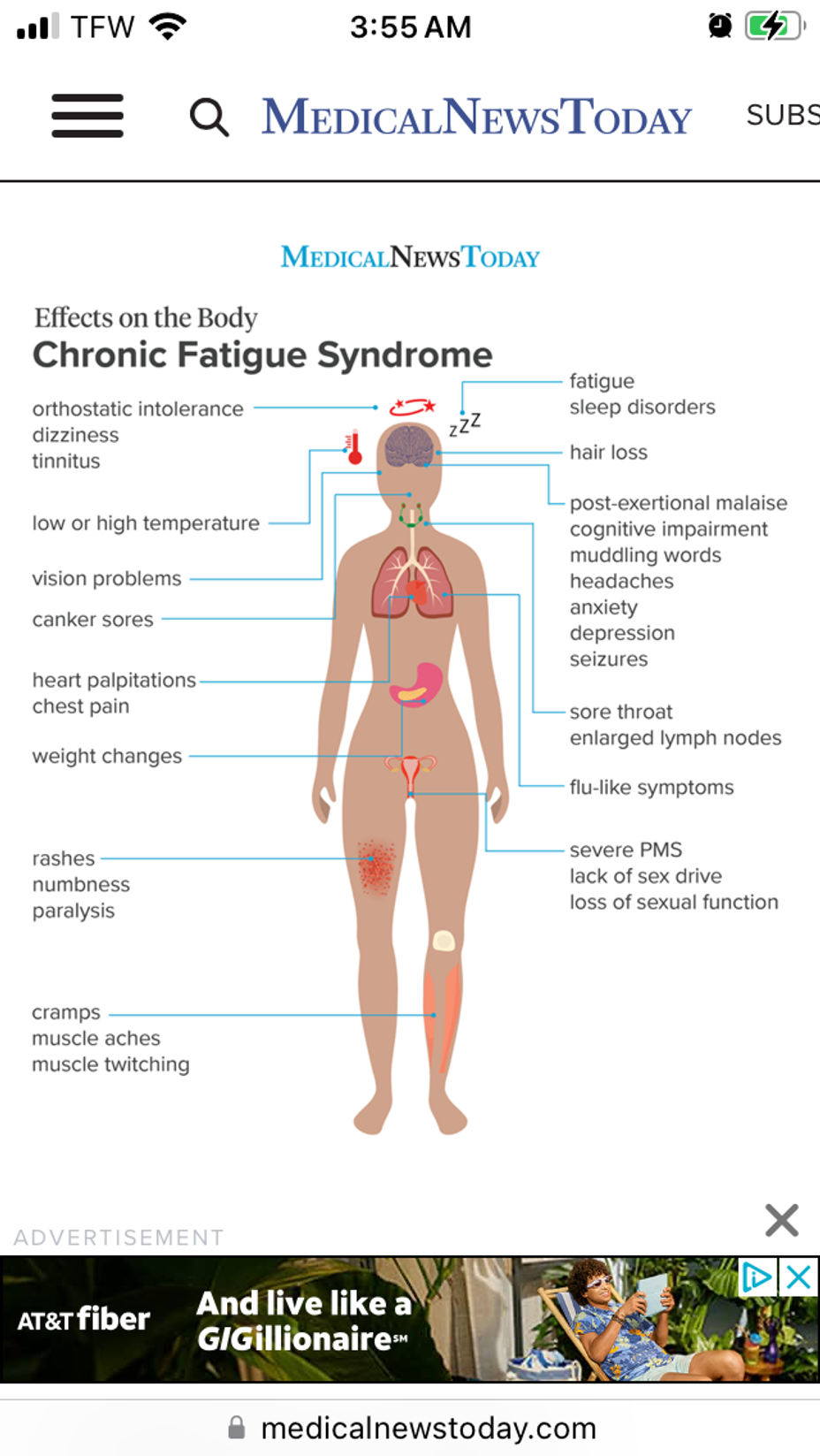
I’m not sure how to keep going. I’ve been doing my best to live with fibromyalgia, CFS, chronic migraines, and many other accompanying issues since 2017. It all began with a car wreck in 2016 that led to a cervical fusion. Fast forward through many different treatments and surgical procedures and we get to 2022 when, after being a stay-at-home homeschooling parent to 4 kids, I finally made the choice to leave my narcissistic abusive husband and had to go to work in retail. My health was not good to begin with and working has just made me go even further down hill. But I’ve had no other choice but to keep trudging through. My two daughters (20 & 22) are both living with me due to their health problems and I have been doing my best to take charge of their care. They are both disabled from chronic physical illnesses and mental and developmental problems. We are currently waiting to see if they are going to be approved for disability benefits. Several months back I began experiencing severe vertigo and vision issues/disturbances along with worsening cognitive function, disorientation and total inability to focus or multitask. My doctor thinks I’m possibly having ocular and/or vestibular migraine symptoms. However, I’ve had to wait almost 2 months to be seen by my neurologist and have an appointment at the end of January. Unfortunately at the beginning of December I ended up in severe pain and couldn’t walk without help due to a suspected herniated disc in my lower back. I have been referred to a neurosurgeon and will be seen at the end of January. I have been put on a three month medical leave from my job and am trying to survive on the tiny bit of savings I have. The money isnt going to last for long. Due to the meds I was given for my back (multiple rounds of steroids, pain meds and muscle relaxers) I have had horrible reactions and coupled with the pain and difficulty getting around, I have been sent into what feels like a never ending CFS crash and my brain function and emotions are severely affected. The fatigue and fibro pain and autonomic symptoms are so awful I feel like I’m dying. I’m barely eating because I’m constantly nauseous and I’ve lost 10lbs since this began. I’m basically living in my bedroom and bright lights and loud sounds are quite intolerable. My doctor doesn’t have a lot of knowledge about my conditions but is extremely willing to help me in any way she can with referrals or medication that I am interested in trying, but otherwise I’m on my own. I don’t yet know if surgery will be necessary for my back, but I’m also questioning whether I’ll be able to go back to work at all when the medical leave ends. If I can’t, then I’m not sure how I’m going to pay my rent/bills and take care of my daughters. I have no idea if or when my girls will be approved for disability and even though I could apply also, the process can take so long that I’m afraid we would be homeless before I got approved. Just not sure what to do anymore and I’m barely functional which just worsens it all. #ME /CFS #Fibromyalgia #ChronicMigraines #AutismSpectrumDisorder #Dysautonomia #EhlersDanlosSyndrome #EosinophilicEsophagitis #UlcerativeColitis #MajorDepressiveDisorder #cognitivedysfunction #Endometriosis #InterstitialCystitis #HerniatedDisc #Vertigo