Child welfare systems exist to protect children from harm. Yet for many children and families, involvement with these systems becomes another layer of trauma rather than a pathway to safety and healing. This paradox is not the result of individual failure—it is the result of systems responding to trauma without being designed to understand it.
Trauma-informed care is not an enhancement to child welfare practice. It is a foundational requirement for ethical, effective, and humane intervention.
Child Welfare Is Inherently Trauma-Exposed
The overwhelming majority of children and families involved in child welfare have experienced multiple, chronic adversities long before a report is ever made. These experiences often include:
*Physical, emotional, or sexual abuse
*Chronic neglect
*Exposure to domestic violence
*Parental substance use and untreated mental illness
*Poverty and housing instability
*Systemic racism and discrimination
*Intergenerational and historical trauma
*Separation from caregivers, siblings, culture, and community
Research consistently demonstrates that child welfare–involved populations have significantly higher Adverse Childhood Experiences (ACEs) scores than the general population, placing them at increased risk for lifelong physical, emotional, and relational difficulties (Felitti et al., 1998; Anda et al., 2006).
Without a trauma-informed framework, child welfare systems risk responding to trauma symptoms as behavioural problems, rather than as adaptive survival responses.
Trauma Shapes Behaviour, Not Morality
Trauma alters neurodevelopment, particularly when experienced in early childhood. It impacts:
*Emotional regulation
*Stress response systems
*Attachment and trust
*Impulse control
*Cognitive processing
*Sense of safety
In child welfare contexts, these trauma responses are frequently misinterpreted as:
*Defiance
*Aggression
*Manipulation
*Non-compliance
*“Lack of insight” or “poor motivation”
A trauma-informed lens reframes the central question from:
“What’s wrong with this child or parent?”
To
“What happened to them, and what do they need to feel safe enough to change?”
This shift is not semantic—it fundamentally alters assessment, intervention, and outcomes.
System Involvement Can Re-Traumatize
Even when removal is necessary for safety, child welfare involvement is itself a potentially traumatic experience. Children often experience:
*Abrupt separation from caregivers
*Loss of routine, identity, and belonging
*Placement instability
*Repeated retelling of traumatic experiences
*Lack of voice or agency in decisions affecting their lives
Parents experience:
*Shame, fear, and grief
*Loss of autonomy and parental identity
*Heightened surveillance
*Re-activation of their own unresolved trauma
Without trauma-informed care, standard child welfare practices—court processes, compliance-based case plans, rigid timelines—can unintentionally replicate dynamics of powerlessness and control, undermining engagement and long-term safety.
Trauma-Informed Care Improves Outcomes
Evidence-informed trauma-responsive child welfare systems demonstrate:
*Greater placement stability
*Improved caregiver-child relationships
*Increased family engagement
Higher rates of successful reunification
*Reduced use of punitive or coercive practices
*Improved permanency outcomes
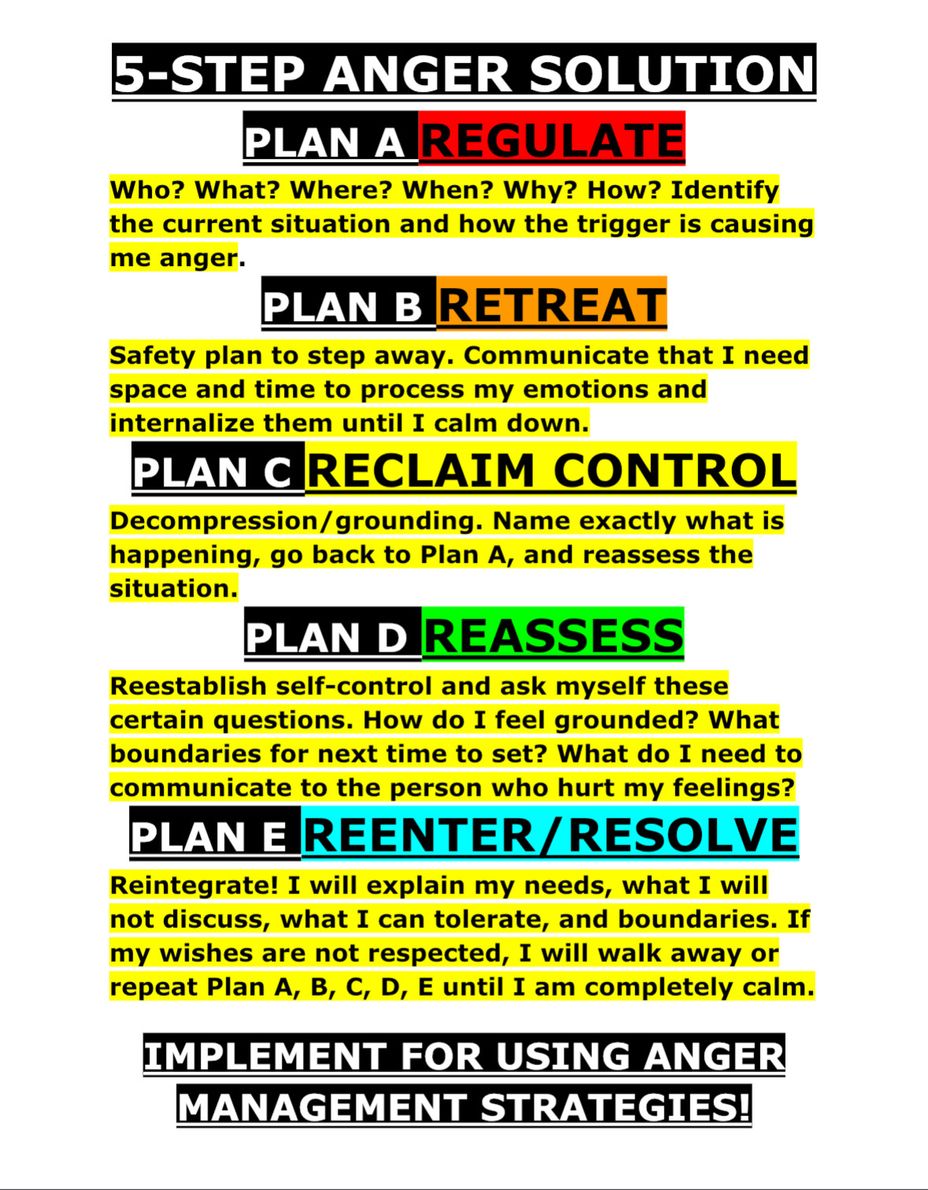
Trauma-informed care recognizes that regulation precedes reasoning. When people feel safe, they are neurologically capable of learning, reflecting, and changing.
Fear-based compliance may satisfy short-term system goals—but it does not create sustainable safety.
Reflection: A Child Welfare Lens
As a child welfare professional, I have seen how easily trauma is mislabeled as resistance—and how devastating that misinterpretation can be.
I have watched children punished for behaviours that were, in truth, survival strategies learned in unsafe environments. I have seen parents deemed “uncooperative” when their nervous systems were locked in fight, flight, or freeze. I have witnessed systems demand emotional regulation, insight, and compliance from people who had never been offered safety, consistency, or trust.
Trauma-informed care challenges us—not just to change how we intervene, but to examine how power is exercised within systems.
*It asks us to slow down in systems designed for speed.
*To listen in systems designed for documentation.
*To see humanity in systems trained to assess risk.
Child welfare does not operate in a vacuum. Many families enter the system already failed by mental health services, addiction supports, housing systems, education, and healthcare. By the time child welfare intervenes, the harm is rarely new—it is cumulative.
If we do not practice trauma-informed care, we become another chapter in that harm.
Trauma-Informed Care Is Also a Workforce Issue
Child welfare professionals are exposed daily to secondary trauma. Without organizational trauma-informed practice, workers experience:
*Compassion fatigue
*Burnout
*Emotional numbing
*High turnover
*Reduced decision-making capacity
A trauma-informed system must support reflective supervision, manageable caseloads, and psychological safety for staff. A dysregulated workforce cannot effectively serve dysregulated families.
Equity, Culture, and Historical Trauma
In Canada, Indigenous, Black, and racialized families are vastly overrepresented in child welfare systems. This reality cannot be separated from:
*Colonization and residential schools
*Forced child removals (e.g., the Sixties Scoop)
*Systemic racism
*Intergenerational trauma
Trauma-informed care, when paired with cultural humility and anti-oppressive practice, is essential to preventing the repetition of historical harm under modern policy frameworks.
Without this lens, child welfare risks perpetuating the very injustices it claims to address.
Call to Action
Trauma-informed care must be embedded at every level of child welfare:
*Legislation and policy
*Intake and investigation
*Court processes
*Placement decisions
*Case planning and timelines
*Permanency planning
Workforce development
Children and families do not come to child welfare because they failed.
They come because systems failed them first.
If child welfare is truly about protection, then trauma-informed care is not optional—it is an ethical obligation.
BigmommaJ
#traumainformedcare #MentalHealth #Recovery