I'm new here!
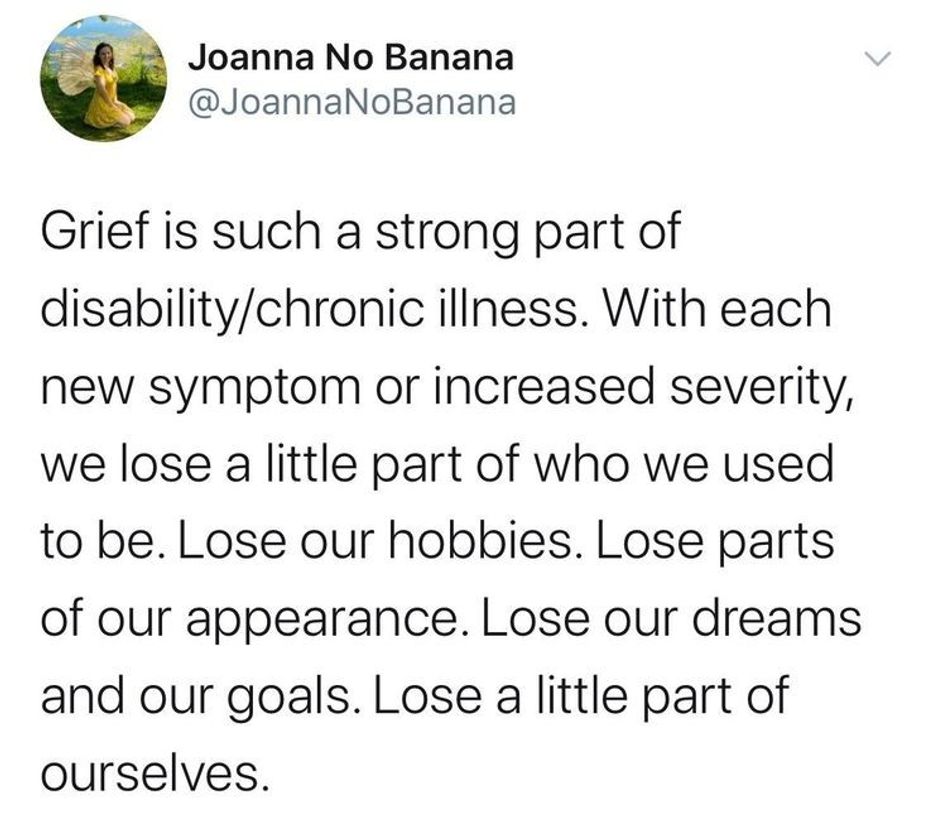
Hi, my name is psouerslpc. I've been diagnosed with CNS Vasculitis after having 3 strokes at the age of 7 (now I'm 33) and recently was diagnosed with Behcet's Disease. I'm interested in learning ways to support myself and others who have chronic illness and chronic pain as I am a mental health therapist. Just looking to learn more about myself and ways to help others :)